Introduction
The practice of anesthesia recently experienced a revolution with the use of ultrasound for perioperative management. This new approach uses point of care ultrasound as an additional imaging tool in the clinical setting.1
Trichobezoar is a rare condition consisting of a collection of indigestible particles-hair-in the gastrointestinal tract. Its management is primarily surgical based on the endoscopic or laparotomy extraction, depending on the size and localization of the particles. The procedure may be elective or in an emergency setting.2-4
The management of anesthesia in patients with trichobezoar needs to consider the patient's hydration and nutritional status, as well as the existence of any comorbidities, gastric emptying dysfunction, and gastrointestinal motility which may have pre-disposed the trichobezoar development. Likewise, airway management in these patients requires evaluating the risk of regurgitation and bronchoaspiration during the induction of anesthesia, to adopt proper preventive measures.5
Following is a discussion of a teenager with gastric trichobezoar, the perioperative evaluation, and the imaging findings, including the gastric contents evaluation using ultrasound as a complementary tool. We shall discuss the clinical significance of using this diagnostic tool in this particular scenario, and its impact on the management of anesthesia.
Clinical case
A 14-year-old female patient admitted to the emergency department with localized abdominal, colic-like pain in the mesogastrium and left hypochondrium, of moderate intensity, non-radiated, unrelated to food intake. The associated symptoms included asthenia, adynamia, and non-quantified febrile peaks. No nausea or food intolerance.
The personal, pathological, pharmacological, and surgical history was negative. A systems review showed chronic constipation with bowel movements every 2 days and pellet stools for the last 2 years. The physical examination indicated good general conditions, afebrile, normal vital signs. A palpable mass was identified in the epigastrium that extended into the mesogastrium, mildly painful to palpation, with no signs of peritoneal infiltration.
As part of the tests ordered, an abdominal X-ray showed a radio-opaque image from the epigastrium to the mesogastrium, with displaced transverse colon and no evidence of intestinal air. An abdominal ultrasound performed by the radiology service showed evidence of a significant dilatation of the intestinal loops at the level of the epigastrium and the left side, with no mass description or characterization. The abdominal computed tomography (CT) showed that the gastric lumen was occupied by heterogeneous material, mostly hypodense, with concentric rings of different density which extended into the first duodenal segment and was surrounded by contrast medium allowing for distal passage that was consistent with Trichobezoar. However, the differential diagnosis needed to consider any type of intestinal mass that was usually non-Hodgkin lymphoma and gastrointestinal stromal tumors tumors.
The psychiatric evaluation evidenced a behavioral eating disorder-hair swallowing-without any depressive/anxiety or psychological symptoms.
The patient was initially evaluated by the pediatric surgery department that decided to program the patient for elective exploratory laparotomy. However, during the hospitalization, the patient presented symptoms of systemic inflammatory response associated with abdominal pain exacerbation and peritoneal irritation, so the decision was made to do an emergency exploratory laparotomy.
The findings of the pre-anesthesia evaluation included an American Society of Anesthesiology (ASA) 1-U patient, functional class above 4 metabolic equivalent of tasks, with no cardiovascular or respiratory symptoms. After a period of 12-hour fasting, no difficult airway predictors were identified in the physical examination. The mother authorized taking images for publication with academic purposes and signed the informed consent, which was approved by the ethics and research committee of the Hospital Universitario San Ignacio.
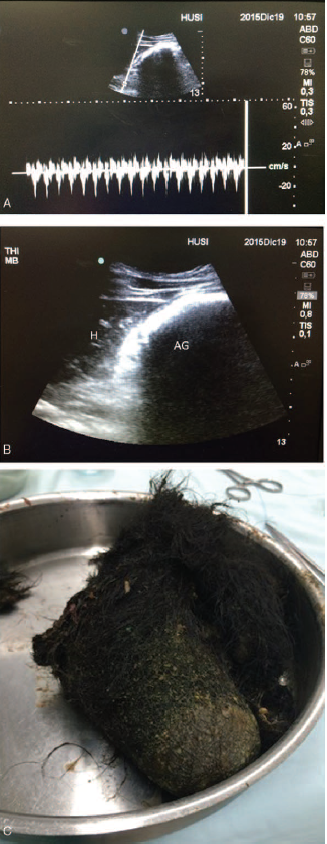
The pre-operative evaluation included ultrasound assessment of the gastric contents using a convex 3 to 7 MHz transducer (Sonosite; Edge, Bothell, WA). That produced the following images.
Anesthesia plan: Balanced general anesthesia with rapid sequence induction using the following drugs: remifentanil initial dose 60 μg (1.3 μg/kg), propofol 130 mg (2.8mg/kg), succinylcholine 90 mg (2mg/kg), and rocuronium 12.5 mg (0.3mg/kg). Laryngoscopy with a curved Cormack I blade, orotracheal intubation with # 7.0 tube with no complications. Maintenance of anesthesia with remifentanil (between 0.3 and 0.5 mg/kg/minute) and sevoflurane of 0.8 a 1.5 minimum alveolar concetration. Uneventful extubation.
The intrasurgical laparotomy finding was compatible with trichobezoar totally occupying the gastric chamber and was completely. In addition, a perforated antral ulcer was identified and corrected with omentoplasty.
The immediate perioperative analgesia was managed with dipyrone at a dose of 30 mg/kg, morphine in boluses of 1.5 mg titrated down to a pain level below 4/10. The patient continued under in-hospital multidisciplinary management with analgesic agents, antibiotics, gastric protection, peripheral parenteral nutrition and psychiatric follow-up. Oral feeding was introduced on day 5 after surgery, with adequate tolerance; the patient was discharged with no complications.
Discussion
"Bezoars" are defined as concentrations of indigestible particles in the gastro intestinal tract. Their classification is based on the origin of the constituent particles. One of the most common types are the trichobezoars (hair particles), phytobezoars (indigestible vegetable particles), and pharmacobenzoars (medications or drug additives).6
The origin of benzoars is multifactorial, including the combination of motility disorders and/or alterations of the gastrointestinal anatomy with the intake of indigestible particles (in patients with psychiatric disorders or mental retardation). Trichotillomania (compulsive hair-pulling habit) and trichophagia (compulsive habit of eating hair, associated with trichotillomania), both pre-dispose to trichobezoars.7
The treatment is based on the mechanical or chemical fragmentation of the trichobenzoar, and depending on size and localization. The elective endoscopic or laparotomy removal. In case of an emergency, laparotomy is mandatory.2-4
It is estimated the 0.5% of patients undergoing IG endoscopy present with benzoars.6 The diagnosis usually requires the use of diagnostic images to identify the presence of the benzoar.
Preoperative evaluation is essential to optimize the patient's clinical condition before the procedure and to decide on perioperative management strategies.
The ASA established in its guidelines the minimum number of fasting hours required to reduce the risk of regurgitation in patients, based on the last meal.8 In addition, special considerations are suggested in patients with conditions that may delay gastric emptying. However, there are no studies in the literature evaluating the gastric emptying behavior of patients with bezoars.
The use of ultrasound in anesthesia is increasing frequent and currently there are many applications of the technology to guide procedures and as an additional tool in the perioperative evaluation of the patient. One of the most recent and promising applications is the qualitative and quantitative ultrasound evaluation of the gastric contents to verify the actual prandial status.9,10 There are several studies in the literature showing a strong correlation between the evaluation of gastric contents with ultrasound versus CT and have suggested the use of this technology to assist in decision-making.11,12 However, there is no available evidence to date about the ultrasound evaluation of gastric content in patients with bezoars.
In the case discussed, based on the low prevalence of this condition, the decision was made to do all ultrasound evaluation of the gastric contents to report the ultrasound characteristics of the trichobezoar. There was significant gastric content as a result of the dilatation of the gastric chamber and beveled glass sign. The ultrasound findings (Fig. 1A) is consistent with a diagnosis of full stomach described in the literature.13 This qualitative evaluation of the gastric chamber at the level of the antrum helped in making the clinical decision to do a rapid sequence induction to reduce the risk of regurgitation and bronchoaspiration, notwithstanding the extended fasting of more than 12 hours. It must be highlighted that the findings of the total abdominal ultrasound performed by radiology reported dilatation of the intestinal loops at the level of the epigastrium, but failed to specifically describe the stomach or the characteristics of the mass, emphasizing the importance of using perioperative ultrasonography to assist clinicians in identifying specific findings that guide management.
Source: Hospital Universitario San Ignacio.
Figure 1 (A) Ultrasound image with low frequency convex transducer in sagittal paramedical position of the epigastrium. This ultrasound section confirms the adequate plane on the gastric antrum, thanks to aortic pulsed wave Doppler. (B) Ultrasound image with low frequency convex transducer. The left hepatic lobe is visible (H) and there is evident distention of the gastric chamber with beveled glass image (AG). (C) Surgical specimen: Trichobezoar. AG=gastric antrum, H=left hepatic lobe.
Conclusion
The trichobezoar is a rare entity that consists of a mass of hair in the gastrointestinal tract. Its management is mostly surgical. Currently, there are no studies evaluating the behavior of gastric emptying in patients with bezoars. The qualitative evaluation of the gastric content with ultrasound is extremely useful in case of a poor medical record, a surgical emergency, or the lack of more sophisticated diagnostic images, when suspecting the presence of such entities. The use of ultrasound enabled the identification of a patient at risk of regurgitation, to assist in decision-making. This reinforces the use of ultrasonography as an additional tool in the pre-operative evaluation of patients, particularly patients under special circumstances, in whom the pre-operative evaluation is not enough to make a decision regarding the adoption of particular approaches.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document work in the power of the correspondence author.











 texto en
texto en 


