Images
Epidural analgesia in abdominal major surgery: pros, cons, and unresolved issues beyond pain control
Fredy Arizaa
b
c
*
Hector Rodriguez-Mayoralb
Karen Villarrealb
a Universidad ICESI, Cali, Colombia
b Universidad del Valle, Cali, Colombia
c Fundación Valle del Lili, Cali, Colombia.
Keywords: Analgesia; Epidural; Pain; Morbidity; Acute Pain; Image
Palabras clave: Analgesia Epidural; Dolor; Morbilidad; Dolor agudo; Imágenes
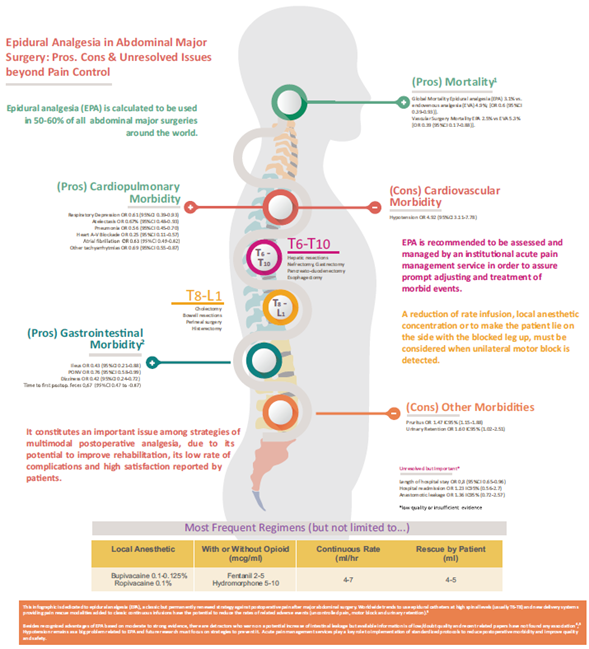
Epidural analgesia (EPA) is a recognized approach to pain control that is used in approximately 50% to 60% of all abdominal major surgeries around the world. It constitutes an important issue among strategies of multimodal postoperative analgesia, due to its potential to improve rehabilitation, low rate of complications, and high satisfaction reported by patients.1,2
Worldwide trends to use epidural catheters at high spinal levels (usually T6-T8) and new delivery systems that provide pain rescue modalities added to classic continuous infusions have the potential to reducing the rates of related adverse events (uncontrolled pain, motor block, and urinary retention).3 Besides recognized advantages of EPA based on moderate to strong evidence, there are detractors who warn on a potential increase of intestinal leakage, but available information is of low/doubt quality and recent related papers have not found any association.4,5
Hypotension remains as a big problem related to EPA and future research must focus on strategies to prevent it. Acute pain management services play a key role to implementation of standardized protocols of EPA in order to reduce postoperative morbidity and improve quality and safety (Fig. 1).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
References
1. Popping D, Elia N, Van Aken H, et al. Impact of epidural analgesia on mortality and morbidity after surgery. Systematic review and meta-analysis of randomized controlled trials. Ann Surg 2014;259:1056-1067.
[ Links ]
2. Guay J, Nishimori M, Koop S. Epidural local anesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting, and pain after abdominal surgery: a Cochrane review. Anesth Analg 2016;123:1591-1602.
[ Links ]
3. Ahmed A, Latif N, Khan R. Post-operative analgesia for major abdominal surgery and its effectiveness in a tertiary care hospital. J Anaesthesiol Clin Pharmacol 2013; 29:472-477.
[ Links ]
4. Piccioni F, Mariani L, Negri M, et al. Epidural analgesia does not influence anastomotic leakage incidence after open colorectal surgery for cancer: a retrospective study on 1,474 patients. J Surg Oncol 2015;112:225-230.
[ Links ]
5. Wang W, Zhao G, Wu L, et al. Risk factors for anastomotic leakage following esophagectomy: impact of thoracic epidural analgesia. J Surg Oncol 2017;116:164-171.
[ Links ]











 texto en
texto en