Introduction
Central venous catheterization (CVC) is a technical procedure used increasingly in the hospitals in the more critically ill patients with greater comorbidities. The majority of the indications are related to the need for parenteral nutrition, long-term antibiotic therapy, use of high-osmolarity drugs, chemotherapy, renal replacement therapy, or when a peripheral access is impossible. The growing use of CVC leads to an increase in complications, even more so when existing international recommendations1-3 are not followed.
Patient information
We present the case of a 56-year-old female patient who developed a vertebro-vertebral arteriovenous fistula following internal jugular CVC and required embolization treatment for symptom remission.
Clinical findings and diagnostic assessment
The patient had a history of hiatus hernia and bilateral radical mastectomy with breast reconstruction because of bilateral lobular carcinoma and presented to the emergency service with pain and functional impairment of the left shoulder following a fall. X-ray imaging ruled out bone fracture, and the patient was discharged on anti-inflammatory therapy. Three days later she again presented to the emergency service with persistent shoulder pain, a low-grade fever, signs of inflammation, and functional impairment. Ultrasound scanning revealed an infected deltoid hematoma with signs of cellulitis. The patient was admitted for drainage, cultures and antibiotic treatment. Because of isolation of methicillin-resistant Staphylococcus aureus, treatment with intravenous daptomycin was initiated, requiring CVC due to poor peripheral venous access. After several attempts at venous catheterization through the right internal jugular vein without ultrasound guidance, the left internal jugular vein was cannulated successfully. Five days later, and coinciding with clinical improvement of the infectious process, the patient reported tinnitus and a murmur sensation in the neck since the CVC was secured. Physical exploration revealed an audible cervical murmur, more evident in the para-cervical muscles and diminished intensity toward the head and chest, also with evidence of cervical thrill. The patient did not report any other symptoms and did not have a neurological deficit. Based on a suspected iatrogenic arteriovenous fistula, the CVC was removed and a cervical computed axial tomography (CT) scan and arteriography of the supraortic trunks were requested (Figs. 1 and 2).
Source: Authors.
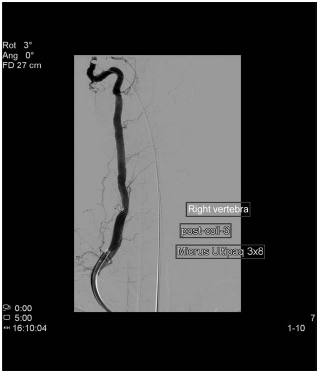
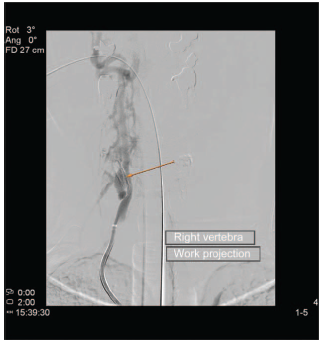
Figure 1 CT angiography of the right vertebral artery. The arrow points to the site of the vertebro-vertebral arteriovenous fistula with paracervical venous plexus overload. CT=computed axial tomography.
Therapeutic intervention, follow-up, and outcome
Endovascular treatment was scheduled based on the diagnosis of direct high-flow arteriovenous fistula of vertebro-vertebral location in the right V2 segment with overload of the cervical vertebral perispinal plexus and final drainage into the internal jugular vein. The treatment was performed 2 days later under general anesthesia for selective right vertebral artery catheterization through the femoral approach and embolization with platinum coils, resulting in uncomplicated complete fistula occlusion. Twenty-four hours later, the patient reported that the murmur and the rest of the symptoms were gone, and she has been asymptomatic since then.
Discussion of the medical literature
CVC is an invasive technical procedure, and, consequently, it gives rise to complications. Non-mechanical complications include infections, with an incidence ranging between 5% and 26%,4 the most important being bacteremia, sepsis, septic thrombosis, septic metastases, and endocarditis. According to the work by Pronovost et al5 and their recommendations on the insertion and maintenance of catheters and their generalized use, incidence of these types of complications will probably drop over the next few years.
Among the mechanical complications, with incidence ranging between 5% and 19%,1 the most frequent are local hematomas, arterial puncture, simple pneumothorax, and venous thrombosis. Sometimes, complications may be life-threatening as in the case of hemothorax, tension pneumothorax, air embolism, or malignant arrhythmias.6-8
Vertebro-vertebral arteriovenous fistulas of different etiology have been described in the literature. Ramos et al9 describe a vertebro-jugular fistula following cannulation of the internal jugular vein, requiring stenting for its resolution. Parsons and Alfa10 describe a case of common carotid artery dissection following accidental cannulation while attempting internal jugular CVC; the dissection required surgical repair and evolved with no neurological sequelae.
Other types of arteriovenous fistulas following CVC have also been described. Sato et al11 describe a subclavian arteriovenous fistula following attempted CVC, and Brzowski et al12 report pseudoaneurysm formation following subclavian CVC. Iatrogenic puncture of the vertebral artery following CVC has been described, either without sequelae or associated with neurological clinical manifestations.13,14 On occasions, arteriovenous fistulas are associated with clinical neurological manifestations of vertebrobasilar insufficiency, and sometimes only with symptoms such as tinnitus, cervical or subclavian murmur described as a "waterfall" sensation, and thrill on palpation. High-flow fistulas may give rise to right ventricular overload and, occasionally, heart failure, as well as thromboembolism. Regarding incidence, Asteri et al estimate it a 0.2% in cases of internal jugular CVC, and 0.03% in cases of subclavian CVC.15,16
Other etiologies of vertebro-vertebral arteriovenous fistulas have been described. They may be spontaneous, congenital, secondary to vertebral artery puncture for arteriography, or accidental arterial puncture not secondary to CVC, the majority of cases reported being complications following cervical trauma.17-19
We have found only 2 reports in the literature of vertebro-vertebral arteriovenous fistula following internal jugular CVC. In 1 case, the presence of the catheter in the vertebral artery and vein was identified. Two years after removal with no complications, the patient presented with vascular murmur in the chest and neck, and a fistula was confirmed by means of angio CT. The other case was a patient who presented with cervico-thoracic murmur described as "running water" 3 years after undergoing cardiac surgery in which CVC was obtained. These cases confirm the frequency with which clinical findings of fistula manifest late in relation to the underlying20,21
Lessons
A rare but potential complication of CVC is vertebro-vertebral arteriovenous fistula secondary to accidental puncture of those vessels. Clinical symptoms, as in the case presented here, manifest usually in the form of tinnitus and cervical murmur, and the condition must be suspected following cannulation either recent or distant in time, for jugular vein CVC. This case illustrates the importance of ultrasound during CVC as a tool to reduce potential complications of the procedure.3
Ethical responsibility
Protection of human subjects and animals: The authors declare that no experiments were conducted in humans or animals for this study.
Data confidentiality: The authors declare having followed the protocols of their institution regarding patient data disclosure.
Right to privacy and informed consent: The authors obtained informed consent from the patients and/or subjects referenced in this article. This document is in the care of the corresponding author.











 text in
text in