Introduction
Mechanical ventilation (MV) is a vital support strategy frequently used in the intensive care unit (ICU). Multicenter studies have shown that, of the population requiring management in the ICU, 35% need MV support.1 The majority of these patients are capable of spontaneous breathing once their clinical condition has been stabilized, and consequently, 60% to 70% are extubated early on (within the first 24hours); however, a minority corresponding to 20% to 30% have failed weaning episodes. Of this population, close to 50% requires MV for a period of 7 days or more, and, consequently, close to 15% of the patients admitted to the ICU need prolonged MV.2-6
The incidence of reintubation within 48 to 72 hours after extubation ranges between 10% and 20% of the total population requiring MV support.7-10 Patients in MV are exposed to significant risks and complications, and these increase with failed extubation episodes.11-13 Survival after discharge of patients requiring prolonged MV has been reported to be significantly lower than in patients requiring MV for a period of up to 48hours.3 Moreover, studies have determined that the time on MV is one of the main factors associated with significantly higher costs in the ICU. Consequently, prolonged MV and difficult weaning results in higher consumption, accounting for 40% of the ICU resources.14-16
Lung gas exchange capacity, cardiovascular integrity, neuromuscular status, psychological conditions, and nutritional status, among other things, have been described as determining factors for the process of weaning from MV. Therefore, failed weaning from MV is considered a multifactorial event.6
Prior studies that have examined factors associated with failed extubation taking into consideration variables related to the ability to protect the airway17-19 have reported an increased risk of failed extubation with ineffectual cough patterns and accumulation of endotracheal secretions. Frutos-Vivar et al20 assessed risk factors for failed extubation and determined that a high fluid balance 24 hours after extubation and the presence of pneumonia at the start of MV are the best predictors for failed extubation.
There are few studies on factors associated with failed weaning from MV, and there are no local reports. The main objective of this research was to evaluate factors associated with failed weaning from MV in patients needing MV support during 48hours or more, and to determine the incidence of failed weaning in the same population.
Methodology
Observational study of a cohort nested in the controlled clinical trial (CCT) Eficacia del entrenamiento muscular respiratorio en el destete de la ventilación mecánica en pacientes con ventilación mecánica por 48 horas o más: un ensayo clínico controlado (Efficacy of respiratory muscle training [RMT] in weaning from MV in patients with 48hours or more of MV: a CCT)21 which assessed the efficacy of RMT for weaning from MV and inspiratory muscle strength in an adult intensive care unit of a Level IV clinic in the city of Cali.21 The main outcome variable analyzed from the data gathered during the trial was failed weaning from MV, and the secondary outcome variables were need for reintubation, need for tracheostomy, or death. Exposure variables were those related to the clinical and socio-demographic conditions of the study population.
The study followed the standards set forth under Resolution 008430 of the Ministry of Health and Social Protection and the Declaration of Helsinki, and was reviewed and endorsed by the Ethics Committee of Santiago de Cali University, pursuant to approval minutes No. 01 of February 3, 2017.
Patients who met the inclusion criteria were enrolled in the study only if they agreed to participate and signed the informed consent. The informed consent was based on the guidelines contained in Resolution 8430 and was taken only by the principal investigator during the recruitment phase of the macro study. During the study, the patients authorized the use of their data for further studies.
The population consisted of records of patients who were part of the macro study and met the following inclusion criteria, which were the same inclusion criteria for the patients in the macro study: "Ventilation support during 48 hours or more; 18 years of age or older; first event requiring ventilation support; intubation in a Level IV healthcare institution or in peripheral centers and referred within 12 hours after intubation; with oxygen blood pressure (PaO2) > 60 mm Hg, FiO2 < de 0.5, positive end-expiratory pressure (PEEP) < 8cmH2O, Richmond Agitation-Sedation Scale (RASS) between -1 and 022,23 and mean arterial pressure greater than 60mmHg, in the absence of vasopressor support or minimum requirement (dobutamine or dopamine <5 µg/kg/min or epinephrine <1 µg/kg/min). Patients with any of the following conditions were excluded: progressive neuromuscular disease; central nervous system lesion; spinal lesion above T5; skeletal disease of the rib cage or spine; ventilation support at home before admission; tracheostomy; infection from multiresistant germs; and pregnant women."21 The sample consisted of 139 patients corresponding to the calculated sample size for estimating a 15% incidence of failed weaning,5 an alpha error of 5%, and a 20% adjustment for losses.
Clinical as well as sociodemographic exposure variables were considered; these variables were recorded upon admission of the patients to the ICU. The sociodemographic variables were age, sex, and height, and the clinical variables were diagnostic classification and main system compromised on admission to the ICU, Apache severity index, time on MV according to the assisted, controlled or spontaneous ventilation modalities, dose of sedatives and analgesics received, inspiratory muscle strength measured by means of maximum inspiratory pressure (MIP), receiving non-invasive ventilation after extubation, receiving pulmonary rehabilitation treatment or physical rehabilitation, and receiving RMT. The main outcome variable was failed weaning from MV, defined as the need for reintubation or tracheostomy within the next 48 hours following extubation, and the need for tracheostomy during MV after a failed attempt at spontaneous breathing.7
Variables in the macro study were documented by 5 physical therapists trained in accordance with the guidelines of the Standard Operating Manual designed by the research team of the CCT.
The information was entered in a database previously designed in EpiInfo and later exported to STAT14 for analysis. Data entry was performed by an individual who received training to that effect, and adjustments and analyses were conducted by the researchers of this study using the STATA14 software package (Licencia de la Universidad del Valle. ESP 02. Numero serial: 1910557280).
Statistical analysis
Data behavior and normality, linearity, and homoscedasticity assumptions for the application of a given test were evaluated by means of an initial exploratory analysis.
Continuous quantitative variables with a normal distribution were expressed as means and standard deviations (SDs), and variables with asymmetrical distribution were expressed as medians and interquartile (IQ) ranges. Categorical variables were described by means of the proportions calculation and 95% confidence intervals (CIs). Univariate and multivariate analyses were performed afterward. The overall incidence of failed weaning from MV was determined as well as incidence according to the clinical and sociodemographic characteristics identified.
Relative risks (RRs) with their respective 95% CIs were estimated using the Poisson regression for estimating crude associations between independent variables and failed weaning from MV, given that the dependent variable of interest (failed weaning from MV) corresponds to a rate with dichotomic outcome, explained by categorically defined predictors.24
The respiratory muscle strength variable (MIP) was dichotomized according to the cutoff point reported in the literature as predictor of failed intubation.25
Variables that showed statistical significance lower than 0.2 (P < 0.2) in the univariate analysis were selected to construct the final multivariate model. Later, the backward methodology was used to build and select the final multiple model. The models were then evaluated using the likelihood ratio test, and the presence of confusion and interaction was also evaluated.
Results
The clinical and sociodemographic characteristics of the patients enrolled in the study are shown in Table 1.
Table 1 Sociodemographic and clinical characteristics of the cohort.
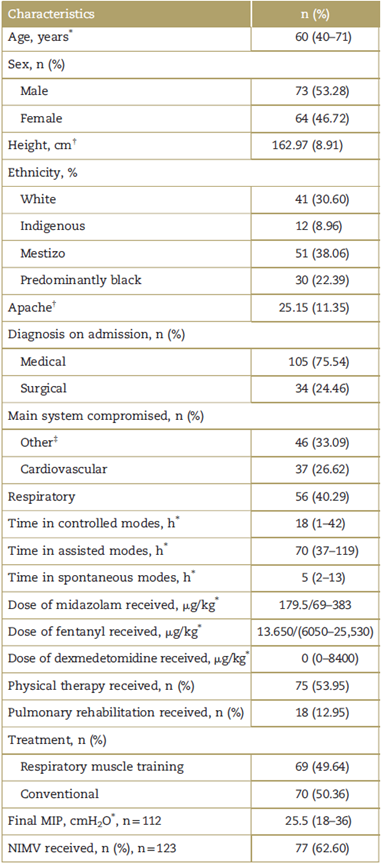
MIP=maximum inspiratory pressure, NIMV=non-invasive mechanical ventilation.
* Median and interquartile range.
† Mean and standard deviation.
‡ Other systems include: muscle skeletal, gastrointestinal, genitourinary, renal, and soft tissues.
Source: Authors.
Mean age was 60 years (IQ range: 40-71), and mean height was 162.97 cm (SD: 8.91). Of the study population, 73 patients were males and 64 females; 105 were admitted to the ICU with a medical diagnosis and 34 with a surgical diagnosis; the median time in controlled MV modes was 18hours (IQ range: 1-42), median time in assisted modes was 70 hours (IQ range: 37-119), and the median time in spontaneous MV modes was 5 (IQrange: 2-13); the median midazolam dose received was 471 mg/kg (IQ range: 69-383); the median fentanyl dose received was 13,650mg/kg (range: 6050-25,530); physical therapy was implemented in 75 patients, and pulmonary rehabilitation was implemented in 18.
Table 2 shows the incidence of overall failed weaning in the study patients.
Table 2 Incidence of failed weaning in the study cohort.
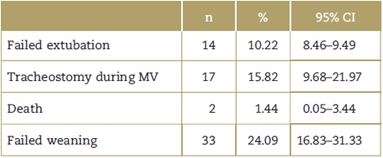
CI=confidence interval, MV=mechanical ventilation.
Source: Authors.
The incidence of failed weaning from MV in the study population was 24.09%, 95% CI (16.83-31.33).
Table 3 presents the incidence and RR of failed weaning from MV according to clinical and sociodemographic characteristics. The univariate analysis showed association between failed weaning and the respiratory system as the main compromised system (RR: 6.9, CI: 2.36-20.10 P = 0.00), and with assisted and spontaneous MV modes (RR: 1.00, 95% CI 1.000-1.007 P = 0.03) and (RR: 1.00 95% CI: 1.00-1.01 P = 0.007), respectively. In average, the incidence of failed weaning from MV dropped 0.96 for every increment in the Apache score; therefore, the Apache score was significantly lower in patients with failed weaning (RR: 0.96, 95% CI 0.92-0.96, P = 0.02). Analyses did not show association between failed weaning and having received RMT, pulmonary rehabilitation, physical rehabilitation, or with any other sociodemographic or clinical characteristics assessed.
Table 3 Incidence and relative risk of failed weaning from MV according to clinical and sociodemographic characteristics.
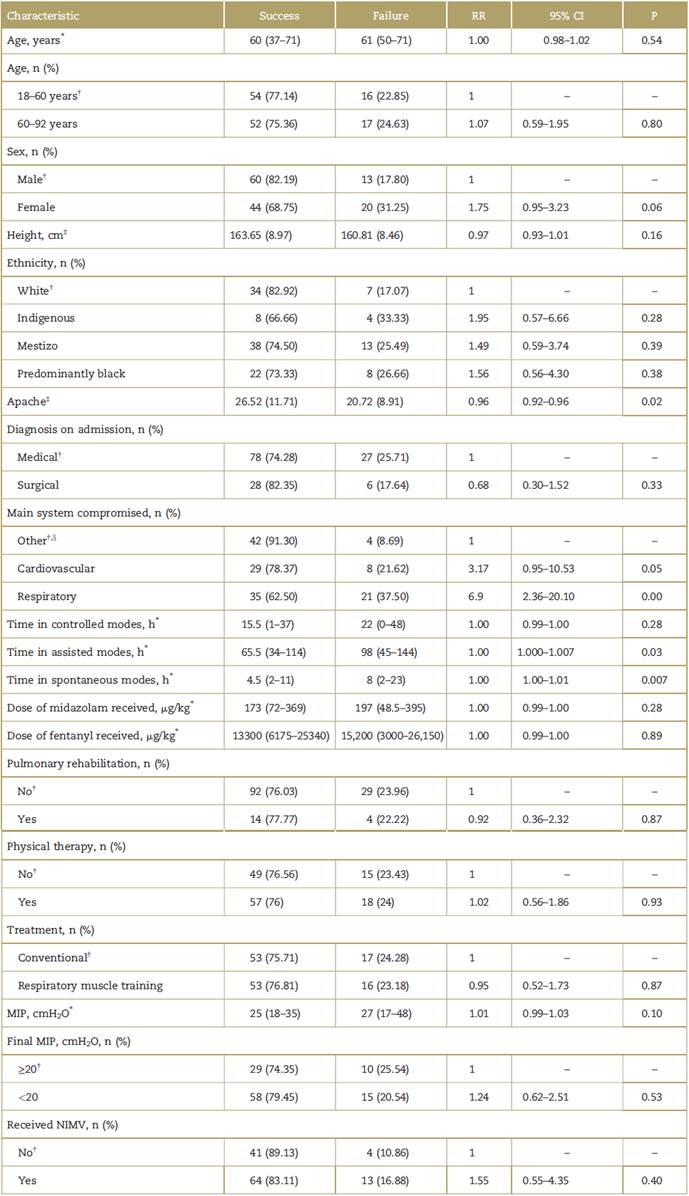
CI=confidence interval, MIP=maximum inspiratory pressure, NIMV=non-invasive mechanical ventilation, RR=relative risk.
* Median and interquartile range.
† Reference category.
‡ Mean and standard deviation.
§ Other systems include: muscle skeletal, gastrointestinal, genitourinary, renal and soft tissues.
Source: Authors.
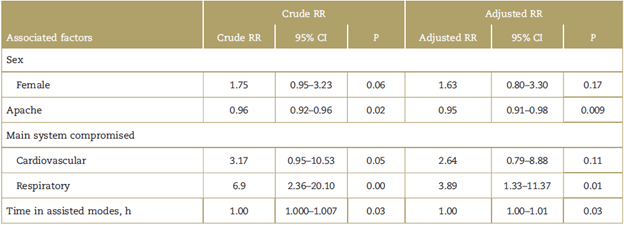
Table 4 shows factors associated with failed weaning from MV. The variables included in the multiple are sex, Apache score, main compromised system, and time in assisted modes. Independent factors associated with failed weaning were compromise of the respiratory system as the main compromise on admission to the ICU (RR 3.89; 95% CI 1.33-11.33) and the Apache score (RR 0.95; 95% CI 0.91-0.98, P = 0.009).
Discussion
The results obtained indicate that factors associated with failed weaning from MV in patients with MV support for 48 hours or longer were identified. Those factors were non-modifiable factors and the most frequent was admission to the ICU with the respiratory system being the most compromised (RR 3.89; 95% CI 1.33-11.37; P = 0.01), whereas the incidence of failed weaning dropped with the increase in the Apache level (RR 0.96; 95% CI 0.92-0.98; P = 0.02). The incidence of failed weaning from MV in the cohort was 24.09%, 95% CI 16.83-31.33.
Of the patients with failed weaning (n = 33), the largest proportion (n = 17-15, 82%) needed tracheostomy during the period of MV. Consequently, the main mechanism for failed weaning in the study cohort was apparently related to the lack of airway integrity, considering that patients with upper airway obstruction or disorder were not excluded. This may also explain why the incidence of failed weaning dropped as the Apache score increased (RR 0.96; 95% CI 0.92-0.98; P = 0.02), probably as these patients had respiratory compromise only with no other system compromise, hence the lower Apache score.
Factors such as the neuromuscular component, nutritional status, respiratory and cardiovascular integrity, and psychological conditions did not influence weaning from MV.6
In this study, compromise mainly of the respiratory system on admission to the ICU was the risk factor most frequently associated with a higher frequency of failed weaning. This category includes patients with respiratory disorders involving the lung parenchyma, the pleura cavity, airway integrity, or rib cage mechanics as main diagnoses on admission to the ICU.
Modifiable factors, such as receiving physical therapy or RMT, were not found to be associated with failed weaning from MV. Therefore, data related to the characteristics of physical therapy such as the number of sessions, goals, and activities were not recorded or evaluated as part of this study. On the other hand, patients who received RMT (n = 69) received between 1 and 14 sessions; 50% (n = 34) received up to two sessions and the remaining 50% (n = 35) received between 3 and 14 RMT sessions; this was due to the short period of MV received by the patients once they met the inclusion criteria. Authors have determined that close to 14 days of RMT are needed to produce significant changes in muscle strength that may be reflected on weaning from MV26,27; consequently, the patients did not receive the number of RMT sessions needed to create significant clinical changes.
Prior studies have evaluated factors associated with failed weaning from MV and failed extubation.
In 1998, Capdevila et al,28 in 17 patients with prolonged MV followed prospectively, determined that failed weaning is associated with prolonged MV, minute ventilation, respiratory rate, high arterial CO2 pressure, and presence of intrinsic PEEP. In 2009, Carlucci et al29 identified, in a population of 30 patients with difficult weaning from MV, that inspiratory burden is higher in relation to neuro-muscular capacity, and this is a pathophysiological determining factor for failed weaning.
In 2000, Coplin et al determined, in 136 subjects with brain lesion, that the risk of failed extubation increases in the absence of reflex cough and the presence of secretions in the respiratory tract.18 In a prospective study with 91 patients conducted in 2001, Khamiees et al concluded that the coughing force and the volume of endotracheal secretions are determining factors for extubation results.19
In 2003, Smina et al determined, in a cohort of 95 patients, that coughing force is an important predictor of extubation outcomes.20 In a multicenter study conducted in 2006 by Frutos-Vivar et al in 900 patients who passed a spontaneous breathing test, the authors identified that a high positive fluid balance and the presence of pneumonia as the main reasons for requiring MV were the main factors associated with failed extubation.21
The results of this study and of prior studies are related to differences in the target population, the methodological design, sample size, exposure variables measured, and the definition of the outcome variable.
This study is an observational study of a cohort recorded during an experimental trial conducted with 139 patients exposed to ventilation support during 48 hours or more; it included patients with various diagnoses and excluded patients with tracheostomy. Studies that have evaluated associated factors are prospective analyses, and 2 of them have been conducted in patients with prolonged MV and included patients with tracheostomy.25,26 The remaining studies were conducted in patients that passed a trial of spontaneous breathing, without specifying MV time,18-20 and in the case of the study by Coplin et al, only patients with brain injury were included.18
On the other hand, only 1 study with a multicenter design has been conducted to date with a sample size larger than the one included in this research,21 and moreover, each author has focused on the measurement of specific exposure variables. Carlussi et al assessed respiratory pattern, respiratory mechanics, respiratory muscle function, and diaphragm tension-time index.30 Capdevila et al measured respiratory pattern, fast and shallow breathing rate, tracheal occlusion pressure, MIP, and inspiratory muscle tension-time index.25 Coplin et al assessed neurological status and airway function.18 Frutos-Vivar et al measured secretions, coughing pattern efficacy, presence of leukocytosis, temperature higher than 38°C, and positive fluid balance.21 Smina et al measured length of intubation, the Apache score, fast and shallow breathing rate, hemoglobin levels, peak expiratory volume, and volume of secretions.20 This research assessed clinical factors considered critical for weaning from MV, as well as sociodemographic factors such as age, height, sex, dose of sedative and analgesic medications received, time on MV according to each ventilation modality, Apache level, respiratory muscle strength (MIP), and the main system compromised on admission to the ICU, among others, are already mentioned.
The outcome variable assessed in this study was failed weaning from MV, defined as the need for reintubation, tracheostomy, or death up to 48 hours following extubation, or the need for tracheostomy after 1 or more failed trials at spontaneous breathing.7 Frutos-Vivar and Ferguson20 evaluated risk factors associated with failed extubation without setting a time threshold, including only patients who required reintubation, and excluding patients who required tracheostomy or who died.
Previous studies have reported values for failed weaning from MV ranging between 26% and 42%,11,25,30,31 and, therefore, the results of this study are similar.
Given that specific conditions are required for measuring and recording exposure variables such as secretion volume and consistency and fluid balance, this study did not consider those variables, and that is a limitation. Other variables such as the level of consciousness and oxygen status were not considered as this study included patients with no oxygenation disorder and with the ability to respond to commands (PaO2 > 60 mm Hg, FiO2 < 0.5, PEEP < 8cmH2O, RASS between -1 and 0). Another limitation was the sample size which may have been insufficient to identify modifiable factors associated with weaning from MV.
Standardization of the process for measuring the study variables and recording the data, and the quality control over the collection, entry, and storage of the original data during the CCT, Efficacy of RMT in weaning from MV in patients on MV during 48hours or more: a clinical controlled trial,1 minimize the possibility of information bias and are a methodological strength.
In conclusion, this research determines that non-modifiable conditions such as the compromised system that leads to ICU admission and the Apache level are mainly associated with failed weaning episodes; modifiable factors such as the level of muscle strength, lung rehabilitation, physical rehabilitation, RMT interventions, and specific ventilation strategies did not show association with this event in the study population.
Ethical disclosures
Human and animal protection: The authors declare that no experiments were conducted in humans or animals for this research.
Data confidentiality: The authors declare having followed the protocols of their institution regarding disclosure of patient information.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document work in the power of the correspondence author. The authors declare that the names of the patients do not appear in this study.











 texto em
texto em