Introduction
Medical practices used in the operating room are increasingly safer, both surgically as well as from the point of view of anesthesia. Protocols and management guidelines contribute to this advancement through the prevention of adverse events, early identification of complications, and effective standardized management should they occur. However, surgical procedures still involve considerable risk.1,2 Postoperative hypoxemia is one of the most frequent anesthetic complications in the postanesthetic care unit (PACU), with incidences ranging from 14% to 80%.3-6 This wide range probably depends on the definition of hypoxemia used, the type of anesthetic and surgical intervention, and the clinical characteristics of the populations studied.
Hypoxemia is considered a pathological state in which peripheral arterial oxygen saturation (SpO2) measured by pulse oximetry is lower than 90%, corresponding to an arterial oxygen tension of less than 60 mm Hg.7,8 It may be early or late, depending on the triggering factors.4,9 Some authors define early postoperative hypoxemia (EPH) as hypoxemia that manifests within the first 2 hours after surgery, while late hypoxemia is defined as that which manifests after the patient has been discharged from the PACU. Others set the first 12 hours after surgery as the threshold between these 2 presentations.9,10 EPH is associated more frequently with anesthesia-related factors, while in late hypoxemia surgical factors, pre-existing conditions, pain, and other postoperative complications have a higher influence.4,11,12
There are circumstances that affect lung function and pre-dispose to hypoxemia. These include the presence of atelectasis, reduced residual functional capacity with greater airway collapse, and altered ventilation/perfusion ratio.6 However, central nervous system depression and inadequate neuromuscular blockade (NMB) reversal are major contributing factors during early recovery from anesthesia.6,13 Age, body mass index, ASA (American Society of Anesthesiologists) classification, anesthesia time, and positioning during surgery, are related clinical characteristics that may influence the onset of pulmonary collapse and deterioration.2,6,14
Postoperative hypoxemia has been a subject of research over the years, because it may result in different outcomes, from longer PACU stay to neurological deterioration and even death. Incidence is known in referral centers around the world. However, as far as we know, the incidence of this condition in PACUs in Colombia is still unclear. The objective of this study is to determine the incidence of EPH in the PACU and to identify related clinical factors in a high complexity centre in Cali, Colombia.
Methodology
Cross-sectional observational analytical study conducted in adult patients taken to surgical procedures with anesthesia recovery in the PACU. This study analyzed secondary data of the Institutional Post-anaesthetic Care Registry (RePACU) of a high-complexity medical center in southwestern Colombia.
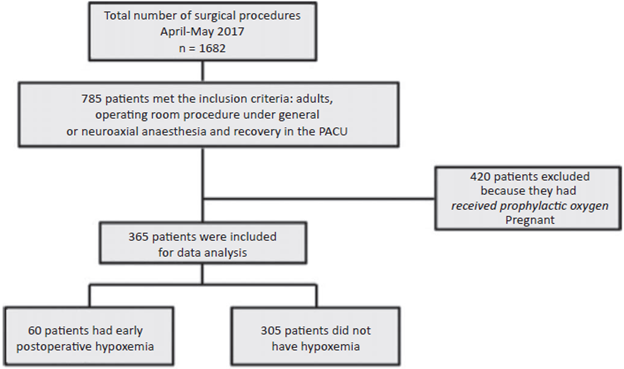
Prospective data of patients taken to surgery under general and neuroaxial anesthesia, with anesthetic recovery in the PACU, were entered systematically in the RePACU. For the study population, all the patients entered in the registry between April and May 2017 were included. Excluded were those patients who were receiving oxygen supplementation on arrival to the unit without having developed peripheral oxygen desaturation (prophylactic oxygen) and pregnant women, due to the increased risk of hypoxemia because of their condition (Fig. 1). Data were obtained from the review of the clinical records, including medical history, demographic, surgical, anesthetic, and analgesic characteristics, he-modynamic variables, and anesthetic complications such as pain, hypoxemia, and postoperative nausea and vomiting.
Source: Authors.
Figure 1 Flowchart of patients entered in the post-anesthesia care registry between April and May 2017. PACU = post-anesthesia care unit.
The type of anesthesia was determined by the attending anesthetist, taking into consideration individual patient characteristics. The types of anesthesia were total intravenous general anesthesia with remifentanil and propofol, balanced inhaled anesthesia with a volatile agent plus remifentanil, or neuroaxial anesthesia. Remi-fentanil and propofol were administered using target controlled infusion and transitional analgesia was then provided with morphine 0.05mg/kg, oxycodone 0.05 mg/ kg, or hydromorphone 2 to 10 µg/kg. For neuroaxial anesthesia, local anesthetics such as heavy bupivacaine plus fentanyl 15 to 30 mg were used, or bupivacaine and morphine 1 µg/kg in patients under 50 years of age requiring postoperative hospitalization. Train-of-four monitoring was used for residual muscle relaxation.
SpO2 and other basic vital signs measurements such as heart rate and blood pressure were performed as part ofthe routine postoperative management in the PACU. They were made every 15 minutes during the first hour, every 30 until the second hour, and then everyhouruntilpatientdischarge from the PACU. In those cases in which anesthesia recovery did not follow a normal course, these measurements were modified based on medical judgment and individual patient needs, and the required therapeutic measures were initiated.
EPH was defined as a drop in SpO2 levels under 90% measured by pulse oximetry at any time point.7,8 It was classified as mild hypoxemia if SpO2 was between 90% and 86%, moderate between 85% and 81%, severe between 80% and 76%, and extreme if SpO2 fell below 76%.6
This study was endorsed by the Biomedical Ethics Committee of Fundación Valle del Lili as stated in approval minutes No. 06 of March 22, 2017. Considering that it was a secondary analysis of the RePACU, no informed consent was required.
Statistical analysis
Data were analyzed using the Stata 14 software package (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). Quantitative variables were presented using the median as central trend measurement and the interquartile range (IQR) as scatter measurement, in accordance with the Shapiro-Wilk normal distribution test.
The incidence of EPH was estimated taking the number of patients with the first episode of hypoxemia as the numerator and, as denominator, the total number of patients at risk of developing EPH for the first time.
In order to identify statistically significant differences in exposure variables (medical history, demographic, surgical, and anesthetic characteristics) between patients with and without hypoxemia, the MannWhitney test was used for continuous variables and the Chi2 or the exact Fisher test for qualitative variables, according to patient distribution in each category. Simple logistic regressions were done using those variables with differences considered as a P value lower than 0.1, estimating odds ratios (OR) and 95% confidence intervals (CIs) in order to estimate their independent effect on the presence of hypoxemia. Finally, a multivariate logistic regression model was built step by step, and likelihood ratio tests were performed. The goodness-of-fittest or model calibration to the data was done using the Hosmer-Lemeshow test, and the discrimination ability of the model was determined with the area under the receiver operating characteristic (ROC) curve, both with a non-supervised sample. A 5% significance level was considered for the multivariate model.
Results
Overall, 365 patients were taken to surgical interventions and admitted to the PACU during the study period. The demographic and clinical characteristics of the population are shown in Table 1. Median age was 49 years (IQR 36-63 years), half were females (55.3%), and 82.2% were classified as ASA I and II. The most frequent medical pre-existing condition was arterial hypertension (21.1%).
Table 1 Demographic and clinical characteristics of the population.
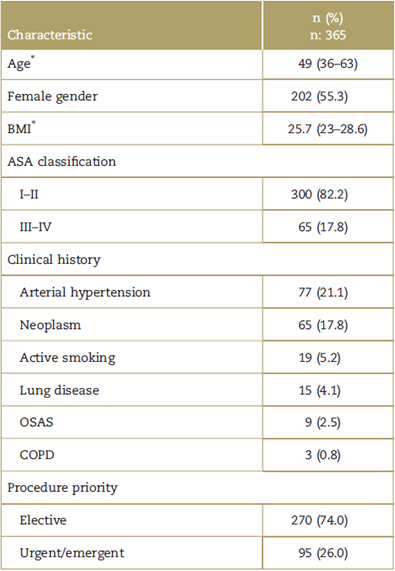
ASA classification=classification systemof the American Society of Anesthesiologists, BMI=body mass index, COPD=chronic obstructive pulmonary disease, IQR, interquartile range, OSAS=obstructive sleep apnea syndrome.
* Value presented as median (IQR).
Source: Authors.
Of the 365 patients included in the study, 60 had a first episode of EPH, for an incidence of 16%. The distribution of EPH-related factors known in the literature2,4-6 is shown in Table 2.
Table 2 Distribution of demographic and clinical variables according to the presence of early postoperative hypoxemia in the postanesthetic care unit.
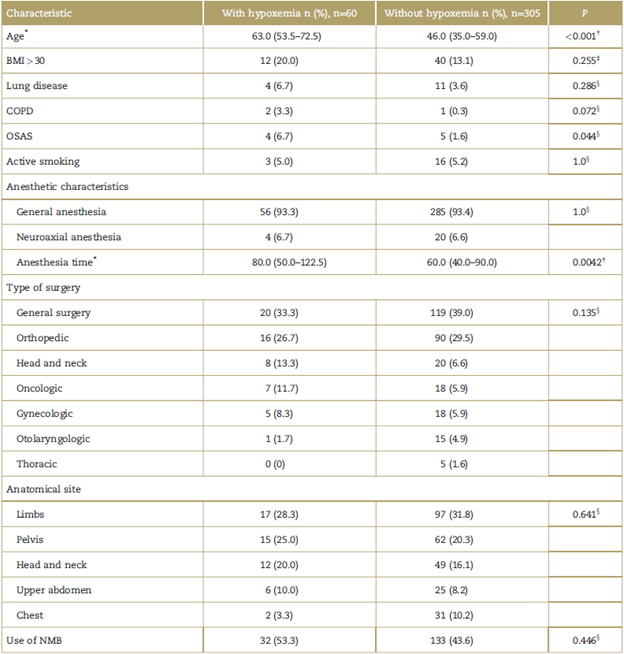
BMI=body mass index, COPD=chronic obstructive pulmonary disease, IQR=interquartile range, NMB=neuromuscular blockade, SAS=obstructive sleep apnea syndrome.
* Value presented as median (IQR).
† Mann-Whitney test.
‡ Chi2 test.
§ Fisher exact test.
Source: Authors.
The median age of patients who developed an episode of hypoxemia was 63 (IQR 53.3-72.5) and patients who did not develop hypoxemia had a median age of 46 years (IQR). Based on simple logistic regression, a statistically significant association was found between EPH and advanced age (OR 1.05, 95% CI 1.03-1.07, P value <0.001) (Table 3).
Table 3 Factors associated with early postoperative hypoxemia in the postanesthesia care unit.
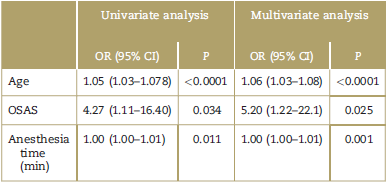
95% CI=95% confidence interval, OR=odds ratio, OSAS=obstructive sleep apnea syndrome.
Source: Authors.
The proportion of hypoxemic patients with chronic obstructive pulmonary disease and active smoking was 3.3% and 5.0%, respectively, with no evidence of statistically significant difference when compared with patients without hypoxemia Table 2). Statistically significant differences were found for the proportion of obstructive sleep apnea syndrome (OSAS) between the patients with and without hypoxemia (Table 2). Both in patients with and without hypoxemia, the most frequent type of anesthesia employed was general anesthesia, and NMB was used only in 53.3% (Table 2). Median anesthesia time was longer in patients with hypoxemia (Table 2). The types of surgery associated with a higher proportion of hypoxemia were general surgery (33.3%) and orthopedic surgery (26.7%), the most common anatomical site being the limbs, 28% in the population with hypoxemia, and 31% in patients who did not develop hypoxemia (Table 2).
Of the 64 episodes of EPH, the most common classification was mild at 3 measurement time points (51.7% on admission to the PACU, 57.8% during the first postoperative hour, and 62.5% during the second hour). The majority of patients presented with EPH on admission to the PACU, resulting in a smaller number of patients in subsequent measurements (29, 19, and 16, respectively) (Fig. 2).
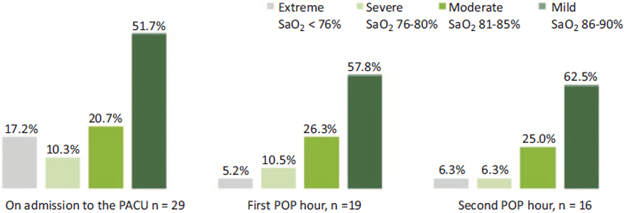
Source: Authors.
Figure 2 Severity classification of early postoperative hypoxemia at the different measurement points. PACU=postanesthetic care unit, POP=postoperative, SaO2=peripheral arterial oxygen saturation.
Age, OSAS, and the type of anesthesia were the variables included step-by-step in the multivariate logistic regression, and it was found that each continued to be associated with the development of EPH while in presence of the other variables (Table 3). The opportunity for a patient developing hypoxemia grows by 6% each for every year of additional age, adjusted for history of OSAS and anesthesia time. The opportunity for hypoxemia in patients with a history of OSAS is 5.2 times higher than in patients without this history, and the effect is greater when adjusted for age and anesthesia time. In addition, it was found that the opportunity for hypoxemia increased by 1% for every additional minute of anesthesia, adjusted for age and a history of OSAS. The final regression model showed adequate fit to the data (Hosmer-Lemeshow test, P = 0.5336) and acceptable to excellent discrimination (area under the ROC curve = 0.7824).
Discussion
Risks and complications arising in the PACU have been reduced with the development of management manuals and practice guidelines.1 Despite this improvement, hypoxemia continues to be one of the most frequent and feared postoperative adverse events. A 16% incidence of EPH was observed in our study population, showing a trend towards the lower limit in the wide range between 14% and 80% found in the literature, and lowerifcompared with studies conducted many years back.3-5 It is evident that patient-related, surgery-related and anesthesia-related factors pre-dispose to this complication, and they have been found to be known factors related to the development of EPH.6,7,15 This study shows that old age, a history of OSAS, and long anesthesia times are factor associated with the presence of EPH.
The population of patients taken to elective and urgent surgical procedures in whom the incidence of EPH is studied varies depending on the region and country where the study is conducted.2,16,17 The demographic characteristics of our population are no different from those found in any other medical centre in this country. In accordance with the selection criteria for the study, patients admitted to the PACU were included, hence the expectation that the majority of the procedures were elective in ASA I and II patients.
Our findings are consistent with those of prior studies, which suggest an association between EPH and age,2,13,18a history of OSAS,18 and anesthesia time.14,19,20 Table 4 shows the results of studies available in the literature on the incidence of postoperative hypoxemia and associated factors. There are other factors described in the literature which were not found to have a significant association in our population, namely, general anesthesia,6 ASA classification,19 and type of surgery.
Table 4 Comparative studies of the incidence of postoperative hypoxemia.
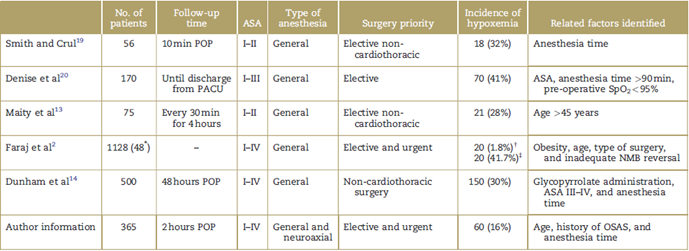
ASA classification=classification system of the American Society of Anesthesiologist, NMB=neuromuscular blockade, OSAS=obstructive sleep apnea syndrome, PACU=postanesthesia care unit, POP=postoperative, SpO2=peripheral arterial oxygen saturation.
* Patients who developed different postoperative complications apart from hypoxemia.
† Incidence of hypoxemia for the general study population (n=1128).
‡ Incidence of hypoxemia in patient population with different postoperative complications (n=48).
Source: Authors.
Age is among the factors most commonly related with EPH.2,13 Increase in the opportunity for hypoxemia with older age is due to the gradual physiologic decline of organ function, with a higher risk of airway obstruction and postoperative hypoxemic events.6 A recent study showed that patients over 70 years of age had more residual NMB, possibly because of altered pharmacokinetics when there is diminished liver, heart, and lung reserve. These patients had more hypoxemic events, postoperative pulmonary complications, and longer stay in the PACU, when compared with patients of a younger age.18
Anesthesia time is directly related with the incidence of hypoxemia, as described by Smith and Crul19 in 1988, Denise et al20 in 1991, and Dunham et al14 in 2014. Surgical procedures lasting longer than 60 minutes are associated with a higher incidence of EPH.6 A possible cause may be the progressive development of abnormal ventilation/ perfusion ratios. However, there are many factors that may have an impact when longer anesthesia times are considered. The information derived from our study is consistent with the findings of these authors, given that there was a higher frequency of EPH in surgical procedures lasting more than 80 minutes.
According to the literature, the intervention which most frequently gives rise to hypoxemia is thoracoabdominal surgery.16,17,21 In this study, although patients taken to thoracic surgery were included, they did not develop hypoxemia. One possible explanation is the use of oxygen supplementation while the patient is transferred to the PACU due to the surgical site and the existence of pulmonary disease, given the higher risk of hypoxemia per se. The complexity of these procedures may be another reason, since most patients are transferred to the intensive care unit for anesthesia recovery. In our institution, the use of prophylactic oxygen is determined by the attending anesthetist. Patients in those 2 situations were excluded from this study, which might explain the results obtained. However, a review of other references show that patients taken to cardiothoracic surgery are not included,13,14,19 given that the incidence of EPH is expected to be much higher, preempting any inferences in the general population taken to elective and urgent surgical procedures.
It is worth highlighting that the use of general anesthesia6 and a history of cigarette smoking are described in prior studies as risk factors for hypoxemia.5,22,23 Our study found the same proportion of these 2 conditions in the patients who developed EPH and those who did not. These results may be due to sample size, limiting the possibility of establishing statistical relationships.
The most frequent type of EPH at the different measurement time points was mild hypoxemia (SpO2 86%-90%), similar to what is described by Maity et al.13 At our institution, pulse oximetry is constant and mandatory as part of monitoring in the PACU. When a patient developed hypoxemia, oxygen supplementation by face mask was administered in order to prevent progression, new hypoxemic episodes, or more serious complications. Despite this measure, some patients had more than 1 hypoxemic episode at more than 1 measurement time point. The highest incidence of EPH occurred on admission to the PACU, and it dropped the longer the patient remained in the unit. These results are consistent with those obtained by Oliveira Filho et al7 and may be due to residual effects from anesthesia24,25 such as central nervous system depression and residual NMB. This trend is to be expected, and it is consistent with the results obtained, considering that the majority of cases with extreme hypoxemia occurred on admission to the PACU.
In terms of limitations of this study, the inability to establish causal associations due to the study design need to be mentioned; both the exposure characteristics as well as the development of the event (EPH) were measured at the same time point. The statistical analysis included tests that show adequate internal validation, but there is no external validation. In terms of strengths, the study allows to recommend that older patients, patients with a history of OSAS and with exposure to prolonged anesthesia time should be considered as a population at risk of developing EPH. Adequate medical control of existing conditions and strategies to minimize surgical time are factors that need to be taken into consideration.
Conclusion
The observed incidence of EPH in our study population was 16%. Old age, a history of OSAS, and long anesthesia time showed a statistically significant association with the presence of EPH. Unlike other reports in the literature, the type of anesthesia, the type of surgery, and anatomical site did not show a significant association with the presence of EPH. Identification of these factors during pre-operative assessment in order to plan for adequate control of existing conditions, and the implementation of institutional strategies aimed at minimizing surgical times is recommended.
Ethical responsibilities
Human and animal protection: The authors declare that procedures were performed in accordance with the ethical standards of the Committee on responsible human experimentation, the World Medical Association and the Declaration of Helsinki.
Data confidentiality: The authors declare having followed the protocols of their institution regarding disclosure of patient information.
Right to privacy and informed consent: The authors declare that patient names do not appear in this study.











 text in
text in 


