Introduction
Anaphylaxis is a systemic life-threatening hypersensitivity reaction (HR).1 Perioperative anaphylaxis is among the main causes of anesthetic complications, with an incidence rate of 1/1250 to 1/18,600 procedures and a mortality rate between 4% and 4.7% (pharmacological anaphylaxis).2 It is caused by the stimulus of bioactive mediators releasing mast cells and basophils, in 2 or more body systems, resulting in increased capillary permeability, vasodilatation, bronchoconstriction, and hypotension.3
Intraoperative anaphylaxis is a complex diagnosis as several symptoms cannot be evaluated in a sedated or unconscious patient, the cutaneous signs are hidden under the surgical drapes, and several drugs are administered simultaneously.3,4 A total of 90% of the cases develop during induction, although there are late reactions as well, and the symptoms exhibit varying intensities, ranging from mild HRs with a preponderance of cutaneous manifestations (grade I) to cardiac and/or respiratory arrest (grade IV).3,5,6 In the presence of only 1 symptom, intraoperative anaphylaxis may be misdiagnosed, in addition to the lack of an evaluation by the allergy clinic, and the risk of a new-potentially lethal -exposure to the agent involved.6
The most frequent signs in the presence of adverse reactions are the absence of pulse, difficult ventilation from bronchospasm, desaturation, and even cardiovascular collapse or cardiac arrest as the primary manifestation.3,5 The reduction in end-tidal CO2 (ETCO2) below 20mm Hg has also been considered a valuable marker.6,7
Patient information
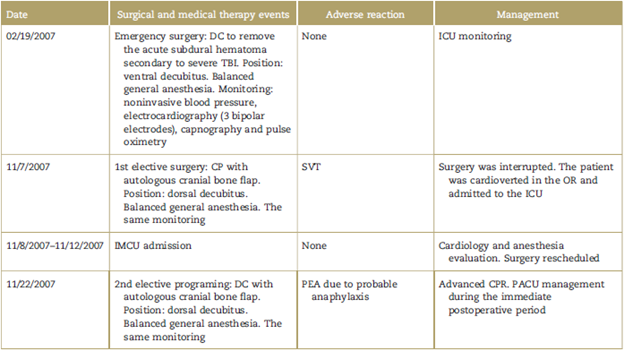
A 44-year-old male patient from a rural area, admitted to the intermediate care unit following his discharge from the intensive care unit (ICU), as a result of supraventricular tachycardia (SVT) over an elective cranial surgery which led to the interruption of the procedure (Table 1). A mild right hemiparesis was identified in the patient on clinical examination. The cardiology evaluation failed to identify any alteration and concluded that the SVT was the result of surgical manipulation or autonomic reflex. An amount of 10 mg of propanolol b.i.d. were prescribed, with a Goldman 2 index classification. No allergies (neither food nor drugs) were reported during the anesthetic evaluation and the patient was classified as American Society of Anesthesiologists (ASA) class 2 and was rescheduled.
Clinical findings
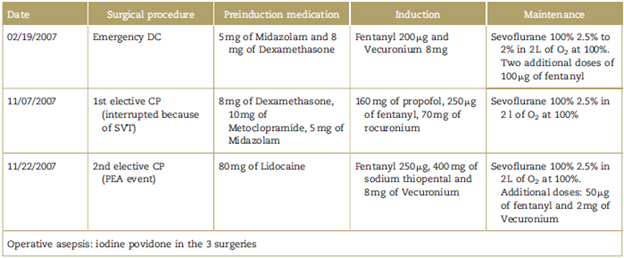
The patient was admitted to the OR with normal vital signs and 95 kg of body weight. Balanced anesthesia was administered for induction (Tables 1 and 2) and endotracheal intubation was performed with a No. 8.5 endotracheal intubation tube (ETT). The surgical procedure began with a 99% oxygen saturation (SpO2) and 30mm Hg of ETCO2. Vital signs were normal during maintenance. One hour after induction, suddenly and with no previous blood pressure (hypotension) or heart rate (bradycardia) alterations, sustained and progressive declines in ETCO2 and SpO2 (down to 24 mm Hg and 92%, respectively) were recorded.
Diagnostic evaluation
Due to the alterations in ETCO2 and SpO2, malfunction of the ETT device was ruled out initially. Immediately after, the absence of palpable pulse and SVT was identified in the multiparameter monitor, with signs of pulseless electrical activity (PEA). Furthermore, when removing the surgical drapes, generalized edema was evidenced and consequently the patient was diagnosed with probable grade IV anaphylaxis.
Therapeutic intervention
Advanced cardiopulmonary resuscitation (CPR) was initiated with continuous chest compressions, IV administration of 1 mg of adrenalin and manual ventilation. Two minutes later, return of spontaneous circulation (ROSC) developed and the compressions were discontinued. However, they had to be reinitiated 1 minute later because of ventricular fibrillation (VF) requiring a 200 joules biphasic shock. A second dose of adrenaline was administered. The VF relapsed on 3 occasions and the same treatment was repeated. After 2 minutes, ROSC was confirmed and a subclavian venous catheter and a radial arterial catheter were placed.
Follow-up and results
The patient was admitted to the postanesthesia care unit with 70/50 mm Hg of invasive arterial pressure, 130 bpm, 90% SpO2, central venous pressure of 10cmH2O, under volume controlled mechanical ventilation and dopamine at adjustable dose. 250mg of hydrocortisone t.i.d. were administered 10hours after PEA, and the patient was extubated without any complications with a Glasgow score of 14 points, 15 hours later. The patient was then transferred to the intermediate care unit where dopamine was then withdrawn after 3 days and 6 days later was transferred to the general hospitalization floor from where he was finally discharged.
Discussion
The intermediate care unit evaluation focused on the SVT that led to the interruption of surgery because of an initial suspicion of cardiac pathology. However, the medical record indicated that the patient was admitted to the ICU following distributive shock resulting from anaphylaxis secondary to an adverse drug reaction (ADR), with hypotension and generalized erythema. Consequently, this first event was probably consistent with grade III anaphylaxis.
The primary cause of perioperative HRs is neuromuscular relaxants (NMRs) (50% to 70%), followed by latex (12% to 16.7%), and antibiotics (15%).2,6 Reviewing the role of the various drugs administered over surgery in the case of immediate HRs (Table 2), sodium thiopental is often involved (incidence 1:30,000), although propofol may also be the culprit. Midazolam (administered in 2 surgeries) and fentanyl (administered in all of them) rarely trigger these reactions.8
Two steroid monoquaternary compounds were used (Rocuronium and Vecuronium), with replaced ammonia ions. These ions represent allergenic sites involved in the specific immunoglobulin E (IgE) recognition which could explain the crossed reactivity (CR) in skin tests of 60% to 70% of patients allergic to NMRs. CR to all relaxants is more frequent when a steroid compound triggered the initial reaction. There were also HRs in NMRs-naive patients because there is CR with cosmetics, foods, and disinfectants.9
Other late intraoperative anaphylaxis-causing agents are iodine povidone and chlorhexidine.10 In a previous report11 Naranjo's algorithm was used to assess the causality of an ADR. This algorithm enabled the analysis of a second HR, with a score of 5 for the relaxant and povidone, which makes them potential ADR agents.12 Considering that few cases were reported in response to topical povidone, the NMR would then be the causal agent.13
Investigating the cause of anaphylaxis may be complex, since there may be several agents involved.8 3 necessary evidences have been described: medical record, biological evaluation, and skin tests.14 The biological evaluation identifies the presence of an allergic mechanism in the reaction through early laboratory tests (total tryptase blood test and plasma histamine) and late laboratory tests (prick test, basophil activation, challenge tests, and specific IgE immunoassays).1,3,5,8,14 In this 2 potential anaphylactic events, only clinical evidence was available. Moreover, the availability of the other tests required in our setting at the time of presentation is unclear.
The critical situation was neglecting the first HR since the patient should have been evaluated by the allergy clinic and the procedure rescheduled, once the agent involved was identified. Failure to do so led to a new exposure to the agent, resulting in a more severe preventable reaction.6,15 Actually, every perioperative reaction must be investigated to ensure safe anesthetic procedures in the future, because even a mild reaction may be due to hypersensitivity and hence be neglected or attributed to unspecific reactions.8,16,17
Some therapeutic approaches to these potential HRs may be optimized; for instance, administering IV fluid challenges, Chlorphenamine and Amiodarone (to avoid the relapse of atrial fibrillation)1,18 (Table 3). The value of the acronym dislodgement, obstruction, suspected pneumothorax and equipment or operator problem (DOPE) has been recognized to address the deterioration of the patient in mechanical ventilation.20
Table 3 Differential diagnosis and management of perioperative anaphylaxis in the adult.
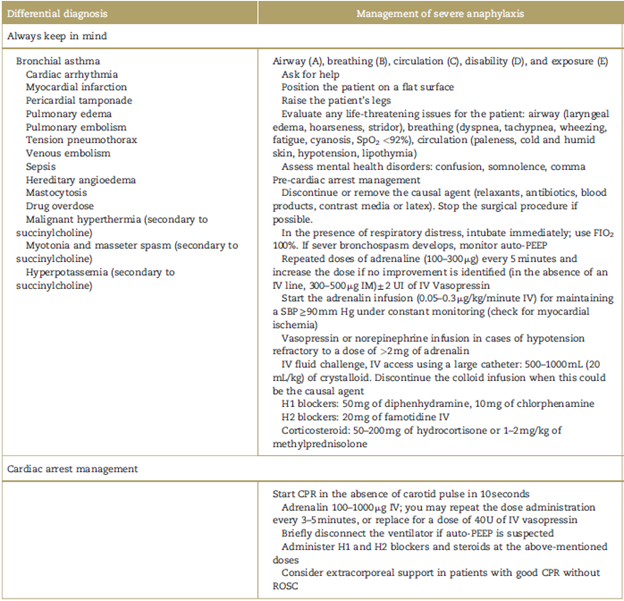
CPR=cardiopulmonary resuscitation, FI02 = fraction of inspired oxygen, PEEP=positive end-expiratory pressure, ROSC=return of spontaneous circulation. Adapted from Chapman and Lalkhen,1 Mertes et al,6 and McEvoy et al.19
Source: Authors.
Following a HR, the anesthesiologist shall request laboratory tests that contribute to a clinical diagnosis, in addition to interconsulting with the allergy clinic to investigate the causal agent. Furthermore, all the Peruvian anesthesiology services nowadays have a mandatory record of adverse events. Finally, the early identification of the disruption in ETCO2 y SaO2 enabled the introduction of timely CPR measures to avoid a fatal outcome.
Patient's opinion
There were no follow-up anesthesia visits to give the patient a detailed written pharmacological report, and the result of the patient's allergy evaluation is unknown.
Informed consent
The Hospital Ethics Committee approved the publication of this case report because the patient is not a resident of the hospital jurisdiction to be able to obtain a written consent.
Ethical responsibilities
Protection of persons and animals: The authors declare that the procedures followed were consistent with the ethical standards of the responsible human experimentation committee and pursuant to World Medical Association and the Declaration of Helsinki.
Confidentiality of the information: The authors state that they have followed the institutional protocols regarding the publication of patient information.
Right to privacy and informed consent: The authors have obtained the informed consents of the patients and/ or individuals mentioned herein. The custodian of this document is the corresponding author.











 text in
text in