Introduction
Achondroplasia is an autosomal dominant disease resulting from fibroblast growth factor receptor 3 mutations,1 which is the most common skeletal dysplasia worldwide, with a global prevalence of around 1 per 15,000 to 25,000 live births,1 with 80% of the cases secondary to de novo mutations.2,3
This clinical entity is characterized by disproportionate dwarfism associated with craniofacial and musculoskeletal malformations, with alteration of the central nervous system, the respiratory, and the cardiovascular systems.2,4 Women affected have low fertility rates and the delivery approach at the end of pregnancy is usually cesarean section because of the cephalopelvic disproportion.5
The management of anesthesia in a pregnant achondroplastic patient undergoing cesarean section is a clinical challenge.5-9 In general, there is no consensus regarding the ideal anesthetic technique as the evaluation of both, general and regional anesthesia, in conjunction with the anatomical alterations typical of the disease and the physiological changes of pregnancy, results in a different risk and complications profile. Consequently, the approach in each case is based on individualized decision-making.10
This article discusses a case of a successful management of an achondroplastic pregnant patient undergoing lower segment cesarean section under subarachnoid anesthesia, and reviews the general guidelines for the management of anesthesia, emphasizing the role of regional anesthesia in this type of patients.
Case description
This is a 23-year-old patient in her first pregnancy, with achondroplasia-functional thanatophoric dwarfism-in her 38.5 weeks of gestation, programed for lower segment cesarean section + surgical sterilization. The patient has a history of occasional alcohol use, with no allergies or prior surgeries, and normal pre-natal control visits. The ultrasound records show a normal development fetus and apparently normal anatomy for gestational age. The patient was admitted to the institution's delivery room with irregular uterine activity. The physical examination indicated the following findings: height: 117 cm, weight: 50 kg, Body Mass Index (BMI): 36.76 (obesity Grade 2), blood pressure: 118/70 mm Hg, Heart Rate (HR) 90xmin, respiratory rate (RR) 19xmin, O2 sat: 96%. Mallampati 2, short neck, thyromental distance less than 6cm, and mild limitation for cervical extension, uneventful cardiopulmonary auscultation, bulky abdomen due to pregnant uterus with fundal height of 32cm, fetal tachycardia: 145 bpm, present uterine activity with irregular contractions. The osteomuscular exploration showed thoracolumbar scoliosis and short extremities with preserved mobility and no evidence of neurological dysfunction.
The patient was admitted to the operating room (OR) after obtaining her informed consent for the suggested subarachnoid neuraxial anesthesia. The 8-hour fasting time was confirmed, basic American Society of Anesthesiology (ASA) monitoring is conducted, and the difficult airway cart is readied. Intravenous fluids are initiated- bolus of 10 cm3/kg (500 cm3). With the patient in the sitting position, the intervertebral L2-L3 space is identified using anatomic landmarks and a puncture was performed using a 27-G Quincke needle, with a successful first attempt to reach the subarachnoid space, which was confirmed with the return of clear cerebrospinal fluid and normal pressure. An amount of 6 mg of hyperbaric bupivacaine with 15 mg of fentanyl was injected, confirming sensitive blockade down to T4. There were no complications over the course of the procedure.
The intraoperative period evolved with hemodynamic stability and no vasoactive support was required. An amount of 1500 cm3 of intravenous fluids was administered and supplementary oxygen with a face mask at 5 L/min, pursuant to the institutional protocol. The patient was placed in lateral decubitus with lateralization of the uterus to the left, to facilitate the venous return and avoid compression of the aorta and the vena cava. In addition, anti-emetic prophylaxis was administered using intravenous (IV) dexamethasone 4 mg, 30 minutes before the start of the surgical procedure and analgesia was supplemented with Nonsteroidal anti-inflammatory drugs (NSAID)-IV diclofenac 50mg after birth. A full-term baby was born, with no anatomic alterations, and a 1-minute Apgar score at birth of 8/10, and of 9/10 after 5 minutes. The weight of the baby was 2970g. There were 600cm3 of intraoperative bleeding with no complications. The patient signed her consent to write the case report, which was endorsed by the local ethics committee.
Discussion
The management of anesthesia in an achondroplastic patient undergoing lower segment cesarean section is a clinical challenge for the anesthesiologist, not just as a result of the anatomic and pathophysiological changes, but also due to the particular influence of these changes on the selection of the anesthetic technique (Table 1).4,7
Table 1 Characteristics of the achondroplastic pregnant patient and anesthetic considerations
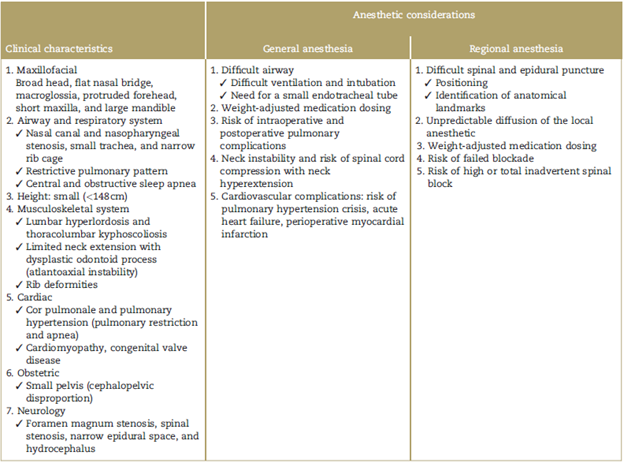
Source: Authors.
Some of the relevant anatomic characteristics include the maxillofacial and airway morphology, with patients usually presenting with broad head, prominent forehead, short maxilla, large mandible, macroglossia, limited neck extension, and pharyngeal, laryngeal, and/or tracheal stenosis,4,7 which in combination may lead to difficult airway management during general anesthesia.
A different but no less important consideration-when considering the possibility of a neuraxial regional anesthesia technique-are the musculoskeletal abnormalities of the spine, such as lumbar hyperlordosis, thoracolumbar kyphoscoliosis, and spinal stenosis, combined with the physiological changes typical of pregnancy that may give rise to technical complications and increased risk of complications.4,7
Considering these 2 probable scenarios, it is absolutely critical to do a complete and rigorous pre-anesthetic evaluation that contributes to a sound clinical judgment to select the appropriate anesthetic technique for each individual case, and to plan in advance for any potential complications.11
There is the idea that general anesthesia is the preferred technique in patients with achondroplasia4,11; however, this recommendation lacks a strong evidence to proof its superiority against regional anesthesia.11 Moreover, a review of the various cases available in the literature suggests that the latter option is indeed a management option.7,10,12-14
Among the regional techniques, the single-dose spinal anesthesia is one of the most frequently used techniques for managing cesarean sections in achondroplastic patients.7,11,15 However, there are also some failed case reports8 that may be accounted for on the basis of the anatomical alterations of the neuroaxis4; depending on the severity of these alterations, spinal anesthesia may be technically challenging, and some authors do not recommend its routine use due to the potential risk of a neurological injury or even to avoid blaming the anesthetic technique for any neurological anomaly.2,4 It should be noted that currently there are no reports in the literature of neurological injury in this type of patients due to the use of regional nauraxial anesthesia. So the recommendation is to conduct a strict perioperative neurological evaluation and to maintain a close clinical follow-up of the patient's postoperative recovery of the motor and sensory function.2
In the case herein discussed, a successful management was achieved using a subarachnoid regional anesthetic technique with single-dose local anesthetic and opioid adjuvant, consistent with the reports in the literature.7,11,16 It is worth noting that a difficult airway team was constantly available as a safety measure.
With regards to the selection of the anesthetic agent, and the dose used in the neuraxial technique, there is no consensus yet on this matter,8,11,12 although the trend in most successful cases reported is toward the use of bupivacaine in combination with various opioid adjuvants (fentanyl or morphine).7 In this particular case, the level identification based on the spinal anatomy allowed us to use relatively low doses of bupivacaine (6 mg that ensured adequate conditions for this type of surgery.
Furthermore, in terms of needle selection for the lumbar puncture, a 27-G Quincke needle was used as this is the only needle routinely available in the institution; however, it should be noted that the use of pencil point needles, such as Whitacre, significantly reduces the incidence of postpuncture headache as an emerging complication.17
Although in this particular case the single-dose neuraxial anesthesia technique led to an adequate clinical outcome, with no perioperative complications, it is also worthwhile considering the use of a titrated regional technique such as the combined spinal-epidural or continuous spinal as a management option, with a higher safety profile.7,8,11,15,16 Moreover, with the advent of tools such as ultrasound, a US-guided puncture may contribute to lower the risks and increase the success rate of the technique.18
Conclusion
A pre-anesthesia evaluation is essential in every achondroplastic pregnant patient to lower the risk of potential complications during the perioperative period, considering the number of morphological and physiological alterations present in these patients. The choice of which anesthetic technique to use is a controversial topic and the decision shall be based on the individual patient characteristics, the experience of the surgical team, and the technical devices available. Moreover, the spinal technique was satisfactory and safe in this particular patient as an anesthetic approach for lower segment cesarean section. The difficult airway team must always be available in case of an event or a potential failed or incomplete anesthesia.
Ethical liabilities
Protection of persons and animals. The authors declare that no experiments were made in humans or in animals for this research.
Confidentiality of information. The authors declare that their workplace protocols on disclosure of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data are disclosed in this article.











 text in
text in 


