Introduction
Burns are the fourth cause of trauma around the world, with 90% of the cases reported in low-income countries, resulting in high mortality and morbidity, prolonged length of hospital stay, disfigurement, and disability. 1 The World Health Organization estimated a total of 265,000 deaths per year as a result of burns in 2016; in 2004, approximately 11 million people experienced severe burns requiring medical care worldwide. 2 In Colombia, the most recent reports date back to the December holidays and are associated with firework burns. SIVIGILA (Public Health Surveillance System) reported 879 cases from December 1, 2016 through January 14, 2017, of which 385 (43.8%) were minors.3
It has been a usual practice to intubate patients with airway burn or inhalation injury early, because of the risk of edema and loss of patency. For several decades reports have been published of studies suggesting that prophylactic intubation of patients with inhalation injury or airway burn may decrease mortality4-6; consequently, the Advanced Trauma Life Support (ATLS) and the Advanced Burn Life Support (ABLS) recommend an early intubation threshold for these patients. 7
The purpose of this article is to review whether patients with airway burn or inhalation injury should be prophylactically intubated, or if different approaches are available to make an airway management decision. A non-systematic literature review shall be discussed in an attempt to answer these questions.
Methodology
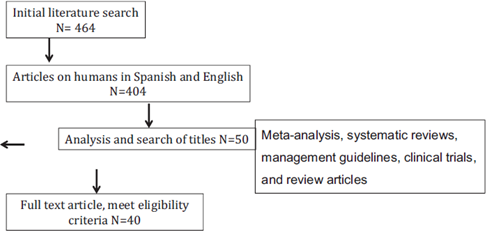
A non-systematic literature review was done including databases such as Pubmed, Medline, UpToDate, and LILACS, using the following keywords in English for the search: "Airway Management" OR "Intubation, Intratracheal" AND "Burns" OR "Burns, Inhalation". Meta-analyses, systematic reviews, management guidelines, clinical trials, and review articles in humans were considered, without a publication deadline in both English and Spanish. Articles for which the full text was nor available were excluded, as well as those where the airway approach in the acute burn patient was not discussed. A total of 50 articles were reviewed to meet the initial objective.
Review
Pathophysiology
The skin is one of the largest organs, representing 16% of the total body weight8; it is responsible for protecting the inside of our body from the environment, preventing fluid loss, and maintaining body temperature. 9 When the skin is injured, as is the case of a burn, there is significant fluid loss and an inflammatory process develops that may be severe and cause death.
Airway burn of inhalation injury is a non-specific term referring to respiratory tract injury caused by heat, smoke, or irritating chemical substances during inspiration. 8 There may be local thermal exposure due to heat exchange and/or exposure to combustion byproducts (lower respiratory tract). The diagnosis may be suspected because of a history of burn inside a closed area, physical examination with declining awareness, soot inside the oral cavity, singed vibrissae, dyspnea, and associated facial burns. 8,10
Locally, in the course of burning, there is protein denaturalization, disrupted collagen links, cell damage, and release of proinflammatory substances leading to increased vessel patency, and hence, the development of edema. 8,10 In the presence of inhalation-associated injury, the oral cavity and the throat develop erythema, ulceration, and also edema, all of which results in airway obstruction. 11-13 In many cases, significant obstruction only develops or further deteriorates as a result of water resuscitation, particularly in burns involving over 20% of the body surface, typically between 8 and 36 hours after the injury and may last for several days. 8,14 If additionally, there are face and neck burns, these may result in anatomical distortion or external airway compression (secondary to edema), that further complicate any respiratory efforts and intubation. 15
The lower airway injuries are of chemical origin and are associated with inhalation of smoke, irritants, or toxic combustion byproducts, 16 presenting with ciliary epithelium damage with impaired physiological clearance, occasional distal obstruction, (secretions that fail to clear or precipitating inhaled particles), secondary atelectasis, impaired gas exchange, and increased risk of bacterial infection. 10,11,17 Furthermore, the major innervation of the tracheobronchial tract is stimulated by the lesion, releas ing neuropeptides and cytokines, further potentiating the initial inflammatory response, increasing cell damage, the loss of hypoxic vasoconstriction with reduced PaO2/FiO2 ratio, leading to respiratory failure. 10,18,19
Among the systemic effects, in addition to the inflam matory response, carbon monoxide poisoning is fre-quent. 20 The diagnosis is based on the medical record (history of burn in closed space, head ache, nausea, muscle weakness, altered consciousness) and carboxyhemoglobin levels above 3% in non-smokers and over 15% in smokers. 11 Likewise, in inhalation lesions cyanide exposure shall be suspected, particularly in unconscious patients or in patients with persistent acidosis. 18,21,22
All of these local and systemic effects in patients with airway burn or inhalation injury, may result in major edema, not just at the skin level, but also of the respiratory tract, 23 with a subsequent loss of patency and the need to secure the airway through intubation or tracheostomy as needed. 10 Moreover, if associated with carbon monoxide and/or cyanide poisoning, it further contributes to the decline of the respiratory function and reduced consciousness.
Should all patients with airway burn or inhalation injury be intubated to prevent airway edema?
Matsuda et al 1981, in a trial with 900 patients, suggest prophylactic intubation in patients with inhalation injury, as a tool that may decrease mortality. 5 Another trial by Phillips and Cope, with a similar number of patients, found a statistically significant relationship between respiratory tract damage (burn sustained in closed spaces and face involvement) and respiratory distress. 4 According to the evidence, inhalation injury is a mortality-independent factor in the burned patient, 4,10,11,23-25 although inhalation injury associated mortality is in itself low (0%-11%), it may be fatal when associated with skin burn in 30% to 90% of the patients. 26,27
A low threshold or intubation is maintained in clinical practice, based on findings as mentioned above. An article published in 2011 showed increased use of mechanical ventilation in patients with over 30% body surface burns, between 1997 and 2006 (76% of the patients require intubation and mechanical ventilation) as compared against the period from 1987 to 1996 (just 38%), with no significant differences between the 2 groups. The authors attribute this increase to the introduction of ATLS in 1995, with its training program and strong emphasis on airway protection. 28
It is too simplistic to state that all patients should be prophylactically intubated. 7,24,29 Keep in mind that the decision to intubate a patient entails risks, increases morbidity, mortality, tracheal injury, repeated laryngoscopies, need for sedation, mechanical ventilation, associ ated pneumonia, and healthcare costs, inter alia. 14,30
Several studies have shown a rise in the number of unnecessary intubations. Romanowski et al31 in a retro spective trial in 2015, including 416 burn and intubated patients, before being transferred to a specialized care center, evaluated the relevance of intubation and found that 171 patients (40.1%) were extubated in less than 2 days (128 patients [31%] on day 1) with no further intubations; the conclusion was that over 1/3 of those intubations were unnecessary. The limitation of these findings is the failure to specify which patients were intubated because of alteration of consciousness but because of resolution of their clinical condition were extubated early; this lack of specificity may result in a bias. Eastman et al, 32 from 1982 through 2005, studied 11,143 patients; 1272 (11.4%) were intubated, of which 527 (41.4%) were extubated in less than 2 days (33.2% on day 1); none required reintubation. The reasons for deciding to intubate included airway edema in 34.1%, prophylaxis 27.9%, and need for oxygenation or ventilation 13.2%. In Portugal in 2015, 33 there were 284 burned patients treated in the course of 57 months; 136 patients (47.9,%) presented with facial burns; 52 of these patients required intubation, 38.5% were extubated in the first 2 days (11.5% at arrival to the emergency room). The reasons reported for the intubation were 72.5% face burn, singed vibrissae, lip edema, and the need to transport the patient; 15% had airway edema (tongue and pharynx) or a positive laryngoscopy; 10% presented with respiratory distress or low saturation, and 2.5% were unconscious.
A late airway approach in patients with progressive edema is catastrophic34,35; in contrast, the current literature based on some studies similar to those above-mentioned, recommends a rational approach when making the decision, as around 30 to 40% may be unnecessary intubations, 30-33 exposing patients to an additional risk. The first 2001 clinical practice Internation al Society for Burn Injury guidelines for caring of the burn patient, state that upper airway obstruction only occurs in 20% to 30% of patients with thermal and inhalation injury26,36; the 2016 updated guidelines recommend intubation or tracheostomy only if the airway patency is endangered and the additional recommended treatment for secondary upper airway inhalation burns is observa tion and monitoring. 36,37
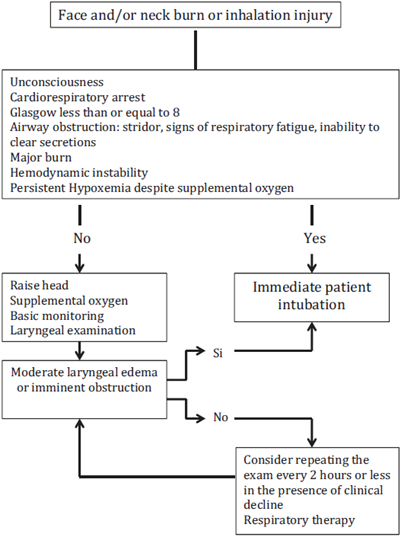
Immediate orotracheal intubation is indicated under the following scenarios: unconscious patients, cardio-respiratory arrest, Glasgow less than or equal to 8, airway obstruction (stridor, respiratory fatigue signs, inability to clear excretions, evidence of burn inside the mouth and larynx), over 40% burned, or persistent hypoxemia despite supplemental oxygen.7 In addition to the previous indications, the ABLS suggests intubation whenever the treating physician has some doubts about the safety of airway patency. 38 When there is no immediate indication for intubation, the recommendation is to do an oropharyngeal examination of all patients with a history of face and neck burn, with or without associated inhalation injury, to decide whether to intubate or keep the patient under observation. 7,18,39
The clinical parameters of facial and nasal hair burn, hoarseness, and carbon-like sputum are sensitive but not specific. 37,40-43 A retrospective study in 2006 involving 41 patients with a history of clinical suspicion of inhalation injury, 44 in which bronchoscopy was performed, showed no correlation between the diagnosis of injury by inhalation and the classical signs of stridor, hoarseness, dysphagia, and increased salivation. However, there was a strong relationship with the finding of soot in the oral cavity, with false and true vocal folds involvement. A prospective, observational trial with 100 patients suspected inhalation injury based on the patients medical record. 45 An endoscopic evaluation of the nasopharynx and tracheobronchial tree was performed in all patients during the 1st hour and follow-up is continued in patients with no initial intubation requirement. Some patients with no vibrissae burns and endoscopic lesion, in contrast with patients presenting singed vibrissae with no airway injury were identified, leading to the conclusion that singed vibrissae and the suspicion of inhalation based on the medical record are insufficient diagnostic criteria. Consequently, the literature recommends a comprehensive clinical evaluation and the use of diagnostic aids for a more accurate judgment to support the intubation decision.
Numerous examinations have been described to clarify the diagnosis and involvement of the airway burn lesion: chest X-ray, arterial blood gasses measurement, Xenon 133 ventilation scan, flow-volume curves, inter alia. However, no test has been able to exceed the results obtained using fibrobronchoscopy, as the current gold standard for diagnosing inhalation injuries, 11,16,23,36,41,42 evaluating not just the upper airway and the tracheobronchial tree, but is also highly effective in removing foreign bodies and accumulated secretions that may further impair the inflammatory response and prevent ventilation. 11,16,23,36,41,43 Fibrocronchoscopy enables a diagnosis of inhalation injury identifying congestion, hyperemia, edema, bullae, ulceration, or soot deposits in both the upper and lower airway, 16,44 and several studies endorse its use based on a sound correlation between the clinical findings and the level of injury and the severity of the airway involvement. 14,39,46,47 A number of scales have been proposed to establish the consistency between these diagnoses and mortality or patient's prognosis, but further validation is needed. 45,48,49
In many emergency departments in Colombia, fibro-bronchoscopes are not permanently or immediately available; this is a costly device that requires special care and a learning curve; hence, the literature recommends as an alternative option, during the resuscitation phase, serial laryngeal examinations by means of a direct or indirect laryngoscopy, aimed at establishing which patients require intubation based on the findings of airway edema or progression thereof.44 The presence of mucosal edema during the laryngeal examination is indicative of thermal injury. Although there is no evidence of the use of videolaryngoscopy in burn patients to assess the airway, this may be an interesting option because of its tolerability in the patient awake and the facility to get a better laryngeal image. Another tool that may be useful in the evaluation of airway edema is ultrasound. Some recent case reports mention the usefulness of tracheal ultrasound to predict edema and edema progression, and it has the advantage of being easily accessible to patients, with the possibility of doing serial studies, providing immediate findings and are not time consuming. 50
In patients with a history or suspicion of airway burn or inhalation injury, with a normal laryngeal examination or mild involvement, the recommendation is to do a serial evaluation every 2 hours or sooner, in the presence of clinical decline14 and suggest the need for close observa tion, oxygen supplementation, and keeping the head up. Any findings of severe involvement or progressive edema are an indication for immediate intubation. 14,45 Refer to Figs. 1 and 2.
Conclusion
The inflammatory process generated during an airway burn or inhalation injury causes edema and a potential risk of losing the airway patency. There must be a high suspicion index and a low intubation threshold versus the risk of airway obstruction. The classical signs and symptoms, such as hoarseness, carbon sputum, facial burn, and signed vibrissae, are all sensitive but not specific predictors to indicate progress to obstruction. Clearly, there is no indication for prophylactic intubation, but there must be a clear indication, keeping in mind all the added risks of intubation. If an airway burn or inhalation injury is suspected, the recommendation is to complement the clinical evaluation with an oropharyngeal examination, sequentially, with fibrobronchoscopy, or laryngoscopy (direct or indirect) and then, in the future, with a tracheal ultrasound to identify the airway edema and its evolution, to make a clinical decision on the indication to intubate or not, based on the findings of obstruction.











 texto em
texto em