Introduction
Catheter placement in the internal jugular and subclavian veins under ultrasound (US) guidance was first described in 1975, and the initial attempts at the use of Doppler for percutaneous angiographic guides were made in 1973.1
Today, the primary aim of US-guided catheter placement is to impact the incidence of complications, increase success rates on first attempt, and increase accuracy, thus becoming a standard in clinical practice.
The traditional landmark technique for central venous catheter placement (local anatomy and palpation of arteries close to veins) does not allow to identify anatomic variants at insertion sites. Moreover, venous thrombosis may occur, particularly in cancer and critical patients, making it impossible to place a central venous catheter. 2,3 Technical breakthroughs and improvements in image quality-US-guided access-allow to identify vessel location, optimal puncture site, and anatomic variants. To a large extent, this helps to avoid venous thrombosis, among other complications. 1 However, the level of benefit varies depending on the skill, training, and learning curve of the operator, as well as the anatomical site. 3 consequently, the type of patient, the interventional team, and the US machine can be considered the cornerstones of US-guided vascular interventions. 1
In general, central venous catheterization may be required for hemodynamic monitoring, delivery of vaso-active drugs and hyperosmolar fluids, and volumetric resuscitation; and in oncologic and hematological patients for blood sampling and preparation of peripheral stem cells, and for the administration of blood products, chemotherapy, or other medications. 4 Therefore, the advantages of US in critically ill patients, 5 ventilated patients, 6 or in situations requiring parenteral nutrition or hemodialysis, 7 are clear today and result in positive outcomes. 8
The aim of this review is to provide a detailed description of the most relevant literature on the impor tance of US guidance for central venous catheterization, as well as on its impact on the safety of the procedure.
Materials and methods
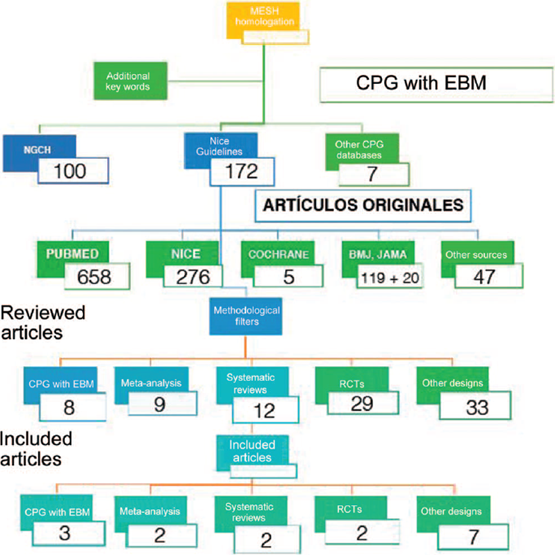
Narrative review of the medical literature related to US-guided central venous catheterization. Various databases were queried, including the National Guideline Clearing house, New Zealand Guidelines, Australian Guidelines, Oxford Journals, Medline, National Institute for Clinical Excellence (NICE), Cochrane, BMJ, JAMA, Science Direct, and OVID. The MeSH terms and key words used for the search map were evidence-based clinical practice guide lines, central venous catheterization indications, US guidance, vascular access, central venous catheter, con ventional landmark guidance.
After applying the selected filters, 91 articles were reviewed, and the final sources were 16 publications with the best level of evidence, because of their designs as clinical practice guidelines, systematic reviews, and meta-analyses.
Results and discussion
Figure 1 shows the results according to the search criteria established for the review.
The only central venous catheter approach with sufficient evidence for recommending its use under US guidance routinely is the internal jugular vein, but it does not mean that this approach should prevail in situations in which the subclavian vein approach for central venous catheterization is indicated. 3,9
This is important as the subclavian approach is better in terms of the percentages of infection, bacteremia, and anatomic variants. 10 However, according to the variables already mentioned, the internal jugular vein and the right femoral approaches provide a more direct route to central veins, facilitating catheter placement without the need for control chest radiographs. 11
Once the need for a central venous access is identified, the next step is to define the approach. The approach that should be considered in the first instance because of its association with a lower percentage of infection is the subclavian vein. If access cannot be achieved through that approach, the next step is to move toward the internal jugular vein, associated with a higher possibility of infection. 12
The internal jugular vein approach has advantages that prompt its selection, including the lower incidence of complications in adjacent structures13; a lower risk of mechanical complications compared with the subclavian approach2; and finally, ease for catheter placement without the need for control chest radiograph. 14
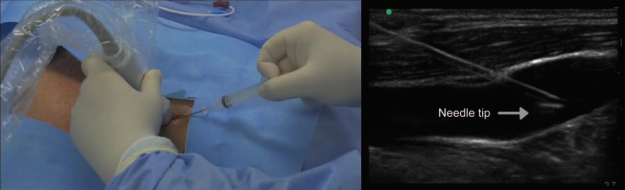
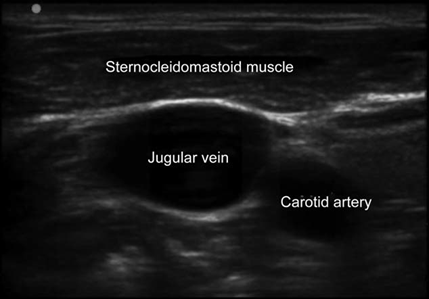
Technological sophistication of US machines varies significant, although the most basic models are good for vascular accesses. US modes for identifying and localizing vessels for catheterization are B mode (bidimensional) and Doppler for flow analysis (arterial or venous). Selecting the appropriate linear high-frequency (5-12MHz) probe is critical for obtaining high-quality images; high-frequency provides better resolution of the tissues lying close to the skin surface, which is ideal for vessel visualization10 (Fig. 2).
Source: Authors.
Figure 2 Ultrasound window showing the relationship between the jugular vein and its neighboring structures.
The structures covered by the US beam underneath the left side of the probe marker (indicated by a light or notch on the side of the probe) always come up on the screen from left to right. Therefore, probes have markings that help with correct orientation. Moving the probe to the left or to the right while watching the image should help confirm the adequate orientation. 15
Transverse and/or longitudinal planes can be used for localization of the selected vein and catheter placement. 16 The transverse position (short axis) is useful for accessing vessels near the skin surface such as the internal jugular vein. 17,18 For deeper vessels, as is the case with the common femoral vein, a combined approach may be used, starting with the transverse position to identify the vessel, followed by rotation to the longitudinal view, initial needle advancement, and cannulation completion. 19
Additional steps are required when using US for central venous access such as the use of the stockinette and the sterile conductor gel. 20
Generally, the patient is placed at 10 and 20 degrees of Trendelenburg to reduce the risk of embolism and promote vein dilation for jugular access; the head is rotated to the opposite side of the puncture, bilateral anatomic recognition of the vascular structures is per formed in a medial-to-lateral direction, making sure there is no thrombosis, and the best site for puncture in the neck or subclavian vessels is identified. Once the puncture site is selected, the area is prepared with asepsis and antisepsis with chlorhexidine for 60 second, sterile drapes are placed, catheters are purged with saline solution, and the probe is covered with the sterile stockinette. 19,20
An illustrative academic video of the techniques was prepared to provide a graphic description of US-guided in plane and oblique longitudinal internal jugular access and US-guided in-plane longitudinal subclavian vascular access (Fig. 3) (Watch the video here: http://links.lww.com/RCA/A57).
In addition, having an US machine allows us to run several checks to ensure the safety of the procedure, such as an US scan of the pleura and the lung to determine the presence of pleural sliding and rule out pneumothorax, providing higher positive predictive and negative predictive values than chest X-ray14,21,22; look for free fluid to rule out haemothorax23; and finally, determine the correct placement of the catheter in the right atrium, with an apical subxiphoid window and bolus in the distal catheter line with 10cm of saline solution24 (Fig. 4).
When the traditional landmark approach is used, complications range between 0.3% and 18.8%, due to multiple variables such as patient population, insertion site, time used, and number of attempts. 25-27
Both Randolph et al4 in a 1996 meta-analysis as well as Rabindranath et al7 in a systematic review and meta-analysis conducted in 2011 show that the use of US for central venous catheterization through the internal jugular vein and subclavian vein in adults is associated with a significantly lower failure rate when compared with the traditional "blind" approach, and also with a reduction in the rate of complications, a shorter approach time and a lower number of attempts at successful access.
Figures for US and the approach to the internal jugular vein are strong. A meta-analysis by Hind et al28 conducted by the British NICE29 found a reduction of the relative risk of complications, failed attempts, and failed first attempt of 57%, 86%, and 41%, respectively. Therefore, the risks of inadvertent arterial puncture and local hematoma, among others, are lower with the use of US for the placement of a central venous catheter in the internal jugular vein.
However, it is important to recognize the adverse events that my occur with US-guided catheterization, including incorrect placement, arterial puncture, local hematoma, air embolism, or nerve injuries. 14,30
Pneumothorax and/or hemothorax are rare events; the majority of cases are recognized by US at the time of the intervention. 31,32 Thrombosis, arteriovenous fistula, and pseudoaneurysms are potential long-term complications and may be readily identified by US. 14,21
In the study by Kaye et al33 (n = 325 patients taken to cardiovascular surgery), the rate of complications follow ing the placement of a central venous catheter (including carotid puncture and pneumothorax) was significantly greater in the group in which no US was used as compared with the group in which US was used.
When US was used as a guide for the central venous catheter, Cavanna et al34 reported symptomatic deep vein thrombosis in the upper limbs in 2.4% of cases and catheter-related infections in 9.96% of the catheters inserted. Catheter removal due to complications was required only in 2.9% of the cases, and there were no reports of nerve injury, major bleeding, or pneumothorax.
Even with the help of US, puncture of the posterior vascular wall may still occur as a complication of venous catheterization. 35,36 The factors that influence the risk of posterior wall penetration include the approach technique, in particular short axis versus long axis, speed of needle insertion, distance between needle entry and the transducer, and insertion angle. 37
In their systematic review, Brass et al mention, regarding internal jugular, subclavian, and femoral vein accesses, complications of nearly 13.5% with the conventional technique, compared with 4% for US-guided catheterization of the internal jugular vein3,9; additionally, the success rate is greater with US, with shorter access time and a lower number of attempts. 1,38
Regarding the subclavian and femoral veins, although some data favor US for these approaches, meta-analyses have not found statistically significant differences when compared with the landmark-guided technique. 18,39-41
In experienced hands, the rate of failure for the landmark technique in the subclavian vein ranges between 9% and 13%.17 Standard approaches have been assessed (supraclavicular, infraclavicular, and, more recently, the axillary approach), but the results are inconclusive. 42-44
Based on these findings, whenever there are difficulties establishing a central vascular access in an adult patient, the suggestion is to use US to help guide the access, provided the operator is experienced. 45-50
Dietrich et al1 mention the following recommendations to help avoid risks and complications:
Optimize the target image in B mode.
Adjust patient position (Trendelenburg) and the position of the examiner and the US machine in relation to the puncture site (comfort for the interventional operator).
Position the head appropriately for localizing the target vein laterally, instead of anterior to the artery.
Get training in viewing skills using adequate practice models such as phantoms, and also in normal patient conditions, and emergency situations.
In hypovolemia, administer intravenous fluid before the puncture.
Obtain training that is certified or has a steep learning curve in simulators or in real life with an instructor to attain international success standards and reduce complications.
Conclusion
US must be used routinely for establishing a central venous access. Current evidence supports this recommendation for the internal jugular vein, but not so for the other approaches; however, in cases of difficult or failed catheterization using conventional methods, US must be used for any of the approaches described as a tool to ensure success. 1,2
Practitioners must be adequately trained in the use of the US machine and must have experience using a high resolution device. Time and practice are needed to become fully competent in these techniques and processes must be reviewed and audited to improve confidence and skill in vascular access, and compliance with standards must be appraised.
In the near future, as a result of the growing use of US for central venous catheterization, new research, brands, and more echogenic catheter materials will become available in the market. The need for these new materials is clearly implicit, considering that they will have a direct impact on the location of the catheter tip, helping reduce the percentage of complications and eliminating the need for verification by means of postpuncture chest radio graphs or fluoroscopy, among other advantages.











 text in
text in