Introduction
Awake craniotomy can be defined as an intracranial surgical procedure where the patient is deliberately awake for a portion of the surgery, usually for mapping and resection of the lesion. It has a long history that pre-dates general anesthesia (GA) as there are many examples of paintings and descriptions of such procedures, especially trephination, dating back over a thousand years. During the last several decades, this procedure has become increasingly popular with wider indications prompted by accumulating evidence that patients receiving awake craniotomy have better outcomes in many aspects. The improvements in anesthetic agents and techniques, especially shorter and more dependable durations of actions, have also made a great contribution. Some aspects of awake craniotomy, including indications and contraindications, benefits, anesthetic techniques, challenges, and potential future directions are discussed. Minimally invasive procedures done through a burr hole, for example, placement of deep brain electrodes for Parkinson's Disease, are also technically awake cranioto mies, but they are not discussed in this review. 1,2
Indications
Awake craniotomy is used for any intra-axial mass lesion residing adjacent to or in eloquent brain based on pre-operative imaging, including motor, and language cortex, and also cortex responsible for other functions, for example, frontal lobe-executive functions. The lesions are primarily gliomas, cortical, and subcortical, both high and low-grade, as the survival rate is related to the extent of resection. 3 Intraoperative stimulation mapping in an awake patient can also be used in (1) refractory epilepsy, as extratemporal seizure foci are often close to eloquent brain areas4; (2) vascular lesions (e.g., arteriovenous malformation) near eloquent areas. 5
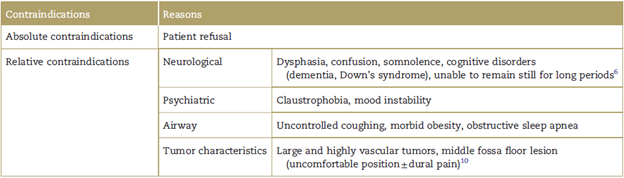
Contraindications
Absolute and relative contraindications are shown in Table 1. There are also some debated contraindications, such as serious medical conditions (congestive heart failure, when ejection fraction <10%),6 3rd trimester pregnancy with looming neurological crisis, 7 and patient's age (the reported age range is 9-90 years old). 8 Awake brain tumor surgery can be performed safely by experienced teams with low complication rates. This is regardless of tumor site, size, and pathology; body mass index; smoking status; American Society of Anesthesiology classification; seizure duration and frequency; emotional or psychiatric history. 9
Benefits
The goal of awake craniotomy is to maximize tumor resection while preserving neurological function. This is achieved by stimulation mapping intraoperatively in an awake patient. With language and sensorimotor mapping functional aspects of the brain can be more accurately delineated so that patients can have more extensive tumor resection, reduced need for postoperative intensive care monitoring and less cost, 11,12 fewer neurological deficits (7% vs 23%), shorter hospital stay (1.7 vs 9 days), 13 longer survival. In addition, after awake craniotomy, patients need less intraoperative vasopressor, have less pain and less narcotic usage, and reduced postoperative nausea and vomiting. Although this procedure can be stressful with up to 30% of the patients having considerable pain and 10% to 14% experiencing significant anxiety, patient acceptance and postoperative satisfaction are high. 14 Posttraumatic stress disorder does not seem to occur. 15 As awake craniotomy with light-moderate sedation doesn't require mechanical ventilation, it avoids physiological disturbance associated with GA. A detailed discussion of the potential disadvantages of GA has recently been reviewed. 16 The data suggest awake craniotomy could improve access to neurosurgical care in poorer countries. 17
Anesthetic techniques
Awake craniotomy requires skill, experience, and the commitment of the entire OR team.
Pre-operative patient interview by all team members is essential in building trust and engagement. A common cause of failure is poor patient communication intra-operatively. Surgeons, anesthesiologist, and nurse provide patients with reassurance and empathy, mitigating their anxiety. Patients should be informed of constant intraoperative face-to-face interactions, and other details includ ing positioning, insertion of an indwelling urinary catheter, craniotomy noise, and mapping-related tasks. Preoperative assessment of language function needs to be done.
Pre-medication
Pre-medication should be personalized according to the patient’s condition and needs. In general, some medications should be avoided or used cautiously, such as midazolam, atropine, and scopolamine, as they can impair neurocognitive function and lead to confusion or delirium. However, a small dose of midazolam (1-2-mg intravenous [IV]) is beneficial in highly anxious younger patients with normal pre-operative neurologic function. Patients having seizure mapping should not receive any medications that suppress epileptiform activity, for example, midazolam, anti-convulsants. There is no consensus on the need to administer anti-convulsants in patients with no prior seizures.
Monitoring
Standard monitoring including electrocardiogram, oximetry, non-invasive and intra-arterial blood pressure, end tidal carbon dioxide, respiratory rate, and urine output is used. Monitors should be placed on the same side as brain lesion to avoid interfering with contralateral sensorimotor monitoring. Processed electroencephalogram (e.g., BIS [Medtronic Inc, Houston, TX, USA], SedLine [Masimo Corporation, Irvine, CA, USA]) monitoring may help shortening the patient awakening time. (18
Positioning
Patients usually are lateral or semi-lateral, turned 90 degrees in reference to the anesthesia workstation and facing the anesthesia team to allow face-to-face interaction and airway management. The head is usually secured in a head frame.
Anesthetics
Currently, several techniques are used in clinical practice, mainly divided into 2 groups: (1) Asleep-awake-asleep. The patient will have GA with laryngeal mask airway/endotra-cheal tube (LMA/ETT) for the craniotomy and closure but awakened and extubated for mapping and resection. (2) Awake-awake-awake. The patient will be awake with sedation (light, moderate, or deep) with spontaneous ventilation for the craniotomy and closure. With both approaches, no medications are usually administered during the mapping phase. The choice of technique must take into account team preference, tumor location, neurological status, body size, age, motivation, and medical comorbidity in addition to the patient's physical condition.
Choice of medications varies interinstitutionally and among individual teams. To achieve smooth transi tions and facilitate intraoperative mapping, anesthetics need to have rapid onset and offset, titratability, and minimal lingering effects. The most commonly used agents are propofol, fentanyl, remifentanil, and dexme-detomidine (DEX), sevoflurane is also used in some institutes. DEX has the unique advantage in that it causes only slight respiratory depression but provides some sedation and analgesia and can be used in combination with other agents or as a sole sedative. 19 Unlike propofol and midazolam, it does not augment neurologic dysfunction. 20
Pre-awake phase
Local anesthesia, either local infiltration and/or scalp blockade, provides effective pain control for both awake craniotomy and GA, and reduces usage of IV opioids. Commonly scalp nerve blockade and local infiltration along the incision line are used with a combination of lidocaine, longer acting agent (bupivacaine or ropivacaine), and epinephrine. Usually there is no pain when dura is manipulated; however, irritations of nerves innervating dura in close proximity to meningeal vessels can cause pain. This is usually managed with infiltration of local anesthetic (LA) along the meningeal vessels.
Commonly used anesthetic regimens for awake craniotomy
Light-moderate sedation: Low-dose propofol (20-50 mg/ kg/minute or 0.5-2.0 mg/mL) and remifentanil (0.01-0.06 mg/kg/minute or 0.2-1.5 ng/mL) infusions should be titrated to make the patient drowsy but arousable, without airway obstruction. DEX 0.3 to 0.5 mg/kg/hour can be used when propofol and remifentanil are not satisfactory or hypoventilation and airway obstruction require propofol and/or remifentanil to be reduced or stopped. Some patients become very disinhibited with propofol and DEX should be added or completely replace the propofol.
Deep sedation: The aim is to maintain spontaneous ventilation but with the use of an airway device for airway patency, for example, nasal trumpet(s) or LMA.
Challenges encountered with sedation are shown in Table 2.
Anesthetic regimens for GA. Intravenous infusions (propofol 50-100mg/kg/minute or 1.5-4.0mg/mL; remifentanil 0.1-0.2mg/kg/minute or 2-4ng/mL), or the use of inhalational agents (sevoflurane or desflurane <0.5 minimum alveolar concentration [MAC]) along with remifentanil 0.1 to 0.2 mg/ kg/minute or 2 to 4 ng/mL, can effect a rapid and smooth transition from asleep to awake. Endotracheal intubation, either orally or nasally, has been used in the past. However, the transition from asleep to awake can be very challenging because of coughing and agitation. Currently, a more popular choice is an LMA, which produces less stimulation and a smoother transition. 23
Awake phase. The goal is to transition smoothly and rapidly without agitation, confusion, or drowsiness from sedation or anesthesia to an awake patient. The patient needs to be engaged, cooperative, pain-free, and comfort able for mapping and tumor resection. All agents are stopped, although it is sometimes useful to keep a very low dose of remifentanil (0.01-0.05 mg/kg/minute or 0.2-1 ng/mL) running or administering small doses of fentanyl for analgesia. Pain should be managed with supplemental LA and possibly IV acetaminophen. Non-pharmacological intraoperative management should be used to reduce fear and anxiety.24 Empathy, hand-holding, reassurance, on going encouragement, coaching, and conversation are all useful and important. A sponge soaked with ice-cold water can be used to wet the patient's lips and mouth for comfort. The patient can be allowed to move limbs and hips at appropriate times. An air blanket is used to provide either warm or cool air to maintain a comfortable temperature.
Physiological test
Motor and sensory pathways. Awake surgery provides accurate mapping of both superficial and deep pathways of the limbs, face, and mouth. Mapping can elicit or inhibit movements. Responses of orofacial musculature, laryngeal activity, and vocalizations can be recorded as tingling or movement, for example, withdrawal of protruded tongue, or speech arrest. 25 Similarly, tingling, twitching, or movement in the limbs may be elicited, most commonly arms and hand. The anesthesiologist should observe the patient carefully and report every movement to the surgeon, and the patient should also be instructed to report any abnormal movement or sensation. The stimulation mapping allows not only delineation of the cortical areas but also allows the surgeon to stimulate and monitor subcortical tracts.
Language. Speech areas cannot be safely localized on the basis of anatomical landmarks. To assess speech, the Visual Object Naming Test is frequently used. The Boston Naming Test consists of 60 drawings of common objects graded in difficulty, for example, window, car, dog, guitar. In addition, language functions can be studied with greater refinement and complexity. 26 Bilingual patients need to be tested in both languages as the anatomical areas may not entirely overlap.
Visual. Intraoperative brain mapping of cortical visual cortex with subcortical mapping of visual tracts may be useful to minimize risk of permanent hemianopia in tumors located in the parieto-occipital area. Identification of optic radiations by direct subcortical electrostimulation is a dependable method to reduce permanent injury in surgery for gliomas involving visual pathways. 27 Methods to identify other functions such as memory and counting are of interest and being developed. 28
Challenges during the awake phase. Common challenges include hypertension, seizures, somnolence, agitation, oxygen desaturation, tight brain, and shivering. 29
Hypertension: This is most commonly secondary to pain, agitation, and anxiety. However, other causes should also be sought such as hypoxia, hypercapnia, and DEX associated. Treatment should focus on managing the cause. Labetalol or esmolol may sometimes be necessary.
Seizures: Seizure incidence is 3% to 16% and happens during cortical and subcortical stimulation mapping. The incidence is less if the surgeon avoids stimulating an area twice in rapid succession. Continuous monitoring of electrocorticography for spikes or sharp waves within 5 seconds after each stimulation allows early detection. Patients with a history of seizure and younger patients especially with tumors of the frontal lobe are more prone to seizures. 19 Intraoperative seizures have a higher incidence of transient motor deterioration and longer hospitals stay. 30,31 First-line treatment of stimulation-evoked seizures is irrigation of the cortex with cold crystalloid solution, and this can be repeated as often as necessary. Intravenous propofol, in small (30-50 mg) repeated doses, is effective, but one must be cautious so as not to produce medication-induced coma resulting in airway compromise. IV fosphenytoin, valproate, lorazepam, or a barbiturate may rarely be needed acutely. Most resolve without adverse outcomes. Cardiac arrest and apnea may occur. Urgent intubation and conversion to GA is necessary for prolonged seizures >5 min.
Emergence agitation and delirium may occur if the pre-awake phase is with GA or deep sedation. Contributing factors include older age; pain; disorientation; inappropriate use of naloxone, flumazenil, neostigmine, and atropine; oxygen desaturation; hypercapnia; urethral stimulation; and bladder distention. It can be very difficult to manage, and there is no consensus on the best approach. An approach is to reinduce anesthesia with a propofol bolus (30-50mg), then administer a DEX bolus 0.1 to 0.2mg/kg before the 2nd wake-up attempt. Low-dose remifentanil infusion 0.01 to 0.05 m g/kg/minute or 0.2 to 1 ng/mL, droperidol or haloperidol before reawaking and physostigmine bolus 0.5 to 1.0 mg are all suggested strategies.
Somnolence: This usually reflects residual anesthetic effects or from anti-convulsants. The best strategy is prevention by early termination of DEX and propofol, and the avoidance of large doses of midazolam or longer acting opioids.
Nausea and vomiting: These are most commonly associated with opioids; other common associated factors are age, gender, and anxiety. The incidence is much lower with the common use of propofol. Management includes empathy, ondansetron, and small dose of propofol (20-30mg). (6) Hypothermia and shivering: These should be pre vented by the use of blankets, warm air devices, and appropriate room temperature. Tramadol 50 mg or 25 to 30-mg meperidine may be effective.
Postawake. Similar to the pre-awake phase, one can also choose awake, spontaneous ventilation under light or deep sedation, or GA with airway control. Sedation often suffices. The patient usually requires lower rates of sedative infusions during the postawake phase than during the pre-awake phase as patients are often fatigued, and there is a lower level of painful stimuli during skull closure.
Postoperative care. The patient should initially be cared for in a high dependency unit or ICU familiar with neurosur-gical patients. Pain management can be achieved by small doses of opioids intravenously including with patient controlled analgesia, oral opioids combined with acet-aminophen. 32
Future research
High-quality randomized clinical trials relevant to the role of anesthesia in the outcome after awake brain tumor resection is lacking. Outcome-oriented studies comparing GA versus MAC and the impact of specific anesthetic agents on brain tumor outcomes (tumor recurrence and progression, survival rate) are needed. Despite many studies comparing short-term outcomes with different anesthetics and analgesics, there is a need for large randomized controlled clinical trials that examine long-term outcomes including tumor recurrence, survival, and quality of life. 33-35
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics commit-tee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.











 texto em
texto em