Introduction
This reflection article is addressed to anesthetists who are occasionally faced with pediatric patients in their surgical work and who have to deal with the anxiety and stress resulting from the fear of failing to secure the airway. This fear is real considering that the main complications in pediatrics originate in airway management and failure to follow simple recommendations that may avoid adverse outcomes. These recommendations are highlighted, using a narrative review and the expertise of the authors.
The article describes the importance of adequate airway management in pediatrics; relevant differences with respect to adults; details of the new classification of the pediatric airway proposed since 2012; and important points of the different algorithms available for airway management. Aspects that are sources of failure during airway management are pointed out, and final conclu sions are presented. The general anesthetist is expected to be able to answer the question of whether the pediatric airway is as difficult as they say, identify children at high risk, and select the safest management strategies.
Importance of the adequate management of the pediatric airway
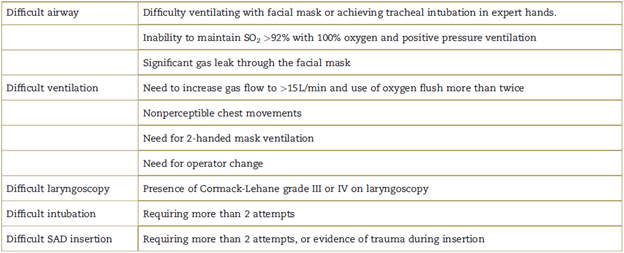
Difficult airway incidence varies depending on the training of the staff assessed, and may be as low as 0.05% among expert anesthetists or as high as 11% in prehospital care. The incidence of pediatric difficult airway lies between these extremes for general practitioners, pediatricians, and intensive care physicians. 1,2 The smaller the child the greater the possibility of a difficult airway. The definition of the "difficult airway" varies according to the scientific society reviewed3-5 (Table 1).
Failed management of the pediatric airway has fatal consequences because hypoxemia sets in very quickly, the child becomes bradycardic in response, and goes into cardiac arrest in a matter of seconds, with the resulting brain injury or death. These events occur much faster than in adults, and, in children, this situation is compounded by "years of healthy life" and the "fragile developing brain," which worsen the clinical, social, and legal outcomes.
The definitions of "difficult ventilation," "difficult laryngoscopy," "difficult intubation," and "difficult supra-glottic airway device (SAD)" are all different (Table 1). 3-5 Each definition is beyond the scope of this article which focuses on the "normal" child and not on predicted difficult airway.
Differences of the pediatric airway: what is important to know?
The most important anatomic differences between the pediatric and the adult airway, and their impact on management are the following:
The larger head and occiput in relation to the body: the large, more anterior, and superior omega-shaped epiglottis requires different alignment for each of the 3 axes for intubation. 6
When children are born, they are nasal breathers by force due mainly to the large size of the tongue in relation to the mouth. However, infants and toddlers may have hypertrophied tonsils and adenoid tissue, creating an obstruction to nasal breathing. Consequently, children may have a different way of breathing at different ages. 7
Tracheal length and diameter predispose to easier selectivity of the tracheal tube during intubation and obstruction thereof due to secretions. 8
In the rib cage, ribs lie more horizontal, and the rib cage is more compliant due to its cartilaginous composition, while the lung parenchyma is stiffer and less compliant.
Diaphragmatic muscle fibers allow faster motion, but are more prone to fatigue, predisposing the child to ventilation failure sooner than in the adult.
Initial descriptions of the pediatric airway anatomy made 50 years ago by Eckenhoff in 1951 and later by Bayeux, showed that the larynx was tapered and its narrowest portion was the cricoid ring. 9 Over the past decade, different studies have shown that the larynx in children is cylindrical, somewhat elliptical, with a larger anteroposterior diameter, and its narrowest portion being the at the site of the vocal cords and the cricoid cartilage, similar to adults. 10-12 Perhaps, the flaw with the initial information occurred because it was based on cadaver models with an unmodifiable cricoid ring and vocal cords were by soft tissue prone to dilation.
The physiological differences between children and adolescents are summarized as less tolerance to apnea, rapid oxygen O2) desaturation, and carbon dioxide (CO2) retention, leading to catastrophic bradycardia and cardiac arrest, if not addressed properly. 13 They include the following:
Lower functional residual capacity (FRC): FRC is deter mined by respiratory reserve volume and residual volume, and is the only site for O2 storage in an emergency. Given that it is proportionally smaller than total lung capacity, the child is at a disadvantage when it comes to fighting apnea with a very limited O2 reserve.
Increased cellular consumption of O2: Neonates in particular have 2 to 3 times higher metabolic activity, and oxygen depletion occurs quickly in case of absent O2 supply.
Increased CO2 production: Increased cell metabolic rate leads to higher CO2 production, and, in cases of ventilation failure, respiratory acidosis sets in very quickly.
Greater closing capacity: The volume of air remaining in the alveoli to prevent their collapse is called closing volume or capacity. In adults, this volume is propor tionally smaller and is consistent with a value consid ered part of the FRC. In neonates and infants, this volume is greater, closer to tidal volume, meaning that small airways collapse with a minimum reduction in tidal volume, atelectasis forms, and oxygenation and ventilation problems are made worse.
In short, anatomic and physiological differences in the child mean that lack of training and adequate management of the airway may result in more severe hypoxemia, bradycardia, and faster cardiac arrest than in the adult.
How is the airway classified in pediatrics?
Pediatric patients include ages ranging from extreme prematurity to 18 years, making it impossible to apply routine anthropometric measurements as is the case in adults. 13 The Mallampati classification is valid in children over 5 years of age. 14 Consequently, airway in a child requires a different assessment based on the following considerations.
Background history
Prior history of difficulty managing the airway is a major determining factor of a difficult airway. It is important to enquire specifically about such a history and also about any interventions on the airway, including mechanical ventilation, tracheostomy, tracheomalacia, stridor, and so on. Age is key, considering that all children under 1 year of age, particularly neonates, present conditions predisposing to difficult airway management.
Anatomic examination
The morphology of the lower third of the face and the presence of head and neck masses or asymmetries are predictors of a difficult airway. Examples include the Pierre Robin sequence, Goldenhar syndrome, Treacher-Collins syndrome, Pfeiffer's syndrome, hygromas, and tumors. Other predictors of difficulty are a mouth opening of less than 3 child fingers across, the inability of the mandible to project beyond the maxilla, and low-set ears which are associated with abnormalities in the development of the first branchial arch responsible also for the development of the upper airway. 13,15
Physiologic examination
Airway inflammatory or infectious variables (rhinitis, bronchitis, bronchiolitis, pneumonia, pharyngitis, etc), and also bronchial hyper-responsiveness and a history of obstructive sleep apnea must be considered in children, because these conditions may give rise to severe obstruction within seconds, due to laryngospasm or broncho-spasm, impairing airway management. 13,15
Based on this assessment, the pediatric airway is classified as follows16:
Normal: No prior history or anatomic or physiological abnormalities suggestive of a difficult airway.
Suspicious: No prior history or anatomic abnormalities, but presence of physiological alterations.
Anticipated difficult airway: Prior history of difficult airway and/or evident anatomic abnormalities.
This classification allows adequate preparation and level of care. Children with anticipated difficult airway must receive care in centers specializing in pediatric anesthesia. Children with a normal airway may receive care from general anesthetists trained to respond to an unexpected difficult airway. Children with a suspicious airway may receive care from general anesthetists with the support from other available anesthetist with experi ence in pediatrics and with all devices, medications, and necessary protocols readily available in the theatre in case of an acute airway obstruction. 17,18
How do we approach the airway in pediatric patients?
The different anesthesia societies have their own algo rithms for approaching the airway in elective and urgent cases, and for anticipated or unexpected difficult airways. Algorithms are also available for difficult ventilation, difficult intubation, and for the worst case scenario, namely, no ventilation and no intubation. In Colombia it is customary to adapt the algorithms of the American Society of Anaesthesia, updated in 2013. 3 In 2012, Doctors Engelhardt and Weissen from the United Kingdom published a special guideline for pediatrics. 17,19,20 They emphasize that each algorithm has its own subtle differ ences and highlight the need for each local anesthesia group to adapt the most appropriate algorithm in accordance with their own resources.
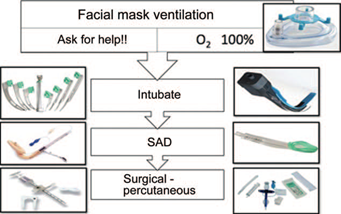
The cornerstone in pediatric airway management includes adequate ventilation with facial mask, asking for help as soon as possible, and elevating the fraction of inspired oxygen (FiO2) to 100%. The next step is tracheal intubation or SAD insertion to secure the airway or even access tracheal intubation through the SAD. Finally, if ventilation and intubation are not possible with any of these options, percutaneous or open surgical approaches through the neck must be considered. In cases of elective surgery, induction may be reversed and the procedure may be rescheduled for a later date when ideal conditions are ensured. When there are problems with airway management, as long as there are no anatomic predictors of a difficult airway, there is the option of increasing the depth of anesthesia or even administer a muscle relaxant to secure the airway more easily. In between these steps of ventilation, intubation, SAD, and surgical access, there are intermediate steps such as flexible fiberoptic bronchoscopy, rigid bronchoscopy, guidewires, tube exchangers, and cannulas that can be adapted in each service (Fig. 1).
What devices are available in pediatrics?
One decade ago, many of the devices available for adult airway management did not exist in pediatrics, particu larly for neonates and infants; nowadays, many of them have become available, including basic or first-line devices, intermediate devices, intubation and advanced devices, and devices for approach through the neck. 21
First-line devices are the "cornerstone" of airway management in pediatrics. The facial mask, when ade quate in size, must cover nose and mouth, and must be fitted tightly making a "seal" over the child's face, using the letter "C" maneuver with the first and second fingers, and the letter "E" with the remaining fingers on the horizontal ramus of the mandible, slightly extending the head. This ventilation may be enhanced with the oropharyngeal or nasopharyngeal cannula in case of oral obstruction. Every child who can be ventilated has little chance of developing complications. The few cases of difficult ventilation may usually be addressed by improving technique and mask fit. Tissue laxity in children allows to improve ventilation with adequate positioning and continuous airway pressure (CPAP), using the air column to "splint" the airway and ensure patency. 21
Intermediate devices include the traditional laryngo scope with different straight or curved types of blades. The straight blade offers a slight advantage in infants because the epiglottis, due to its shape and location, must be "engaged and elevated." There are different types of videolaryngoscopes available in pediatrics; they have shown to improve the view of the glottis and success with tracheal intubation when laryngoscopy is classified as Cormack-Lehane types III and IV. Intubation with the videolaryngoscope is more time-consuming than with the conventional laryngoscope, and it is worth highlighting that, in pediatrics, that apnea time matters. 22-24
Another option for intubation is the use of the fiberoptic bronchoscope. The flexible one is the gold standard for approaching the anticipated difficult airway because it allows both oral and also nasal intubation or SAD intubation. The rigid scope is the device of choice when the difficulty is related to infraglottic issues such as airway compression by a foreign body or a mass, because ventilation and oxygenation are possible during the procedure through the wide working channel and connections.
Supraglottic airway devices include first-generation devices that allow only ventilation and oxygenation, as is the case with the classical laryngeal mask, and second-generation devices featuring a gastric suction channel, preformed curve, and bite protection. They allow tracheal intubation and the performance of fiberoptic bronchosco py because of their diameter, shape, and fittings. Second-generation SADs are easier to fit, fail less, and are the most advisable. 25 A discussion about the advantages and0 disadvantages of each of these devices is beyond the scope of this paper.
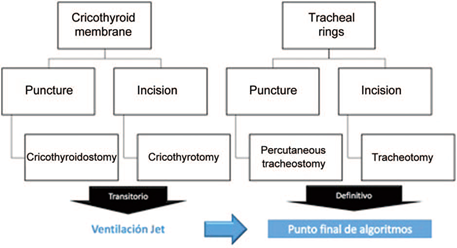
Using the advanced devices, the airway is approached trough the neck, especially in cases of no ventilation or intubation when everything else has failed, an extremely rare situation in pediatrics which can be reversed by improving the ventilation and intubation technique. These are percutaneous approaches that may be performed on the cricothyroid membrane or the tracheal rings, entering either by puncture or incision (Fig. 2). Approaches through the cricothyroid membrane are transient while waiting for a percutaneous or open tracheostomy through the tracheal rings as a definitive approach in the case of a difficult airway. 26-28
Recommendations for reducing airway failures
During preparation
Take time to assess and classify the airway. Consider the environment in which the airway will be approached, determining the physical condition of the child, functional class, surgical risk, and the urgency of the procedure. Then, prepare the equipment and drugs you will be using. Determine your plan for approaching the airway and alternative options: plan A, B, and C. Explain to the attending staff what the airway approach plans are and when they will be asked to intervene.
During preoxygenation
Preoxygenate for at least 3 minutes at 100% to obtain 6 to 8 vital capacities, enough to provide O2 saturation of FRC. Use sedation to ensure that the process will flow smoothly in the uncooperative child, without losing the ventilation pattern.
If you need more than 1 attempt at intubation, preoxygenate again at least during 1 minute. Also, when arterial O2 saturation (SaO2) is less than 90%, the real SaO2 will be lower because the SaO2 tracing has an approximate 40-second delay.
Consider apneic oxygenation when facial mask ventila tion with positive pressure is contraindicated. It consists of using a nasal cannula together with the facial mask, with a flow ranging between 2 and 6L/min depending on the age of the child.
Optimize the facial seal when using mask ventilation and secure airway patency by means of manual CPAP. Placement of an interscapular roll in children under 2 years of age, or an occiput support in older children, facilitates ventilation and tracheal intubation because it helps improve alignment along the 3 axes of the airway: oral, pharyngeal, and tracheal.
When faced with difficult ventilation and oxygenation in the absence of an anticipated difficult airway, consider increasing the depth of anesthesia and giving muscle relaxants to facilitate the maneuvers.
During laryngoscopy
Optimize intubation conditions from the start, because the first attempt is the best. Allow sufficient drug latency because manipulating the pediatric airway without ade quate depth of anesthesia increases the incidence of gagging, cough, laryngospasm, glottic edema, and failed tracheal intubation. The ideal time lapse for securing the airway once ventilation-oxygenation is stopped is 20 seconds in neonates and 30seconds in all other children.
Prefer the straight blade for laryngoscopy in infants because engaging and elevating the epiglottis is the easier approach to the airway in this age group.
Recognize the difficulty of managing the airway promptly and ask the person with more expertise for help; provide 100% oxygen and trigger alternative treat ment plans. Limit laryngoscopy attempts to 3 and proceed to alternative plans. Repeated laryngoscopy attempts must be performed with variations of the technique, that is, change of blade or positioning, to look for a different result. View the passage of the tracheal tube through the glottis; this way, the videolaryngoscope allows the person performing the intubation and also the assistant to see what is happening, and, in case of failure, the second anesthetist may adjust the technique accordingly, in creasing the possibility of success.
Identify esophageal intubation early on, when passage of the tube through the glottis cannot be viewed directly and 10 seconds elapse without obtaining the adequate capnography tracing. Any delay in recognizing this event limits response time and a fast solution to failed intubation.
Training
It is wrong to assume that daily practice is a source of sufficient training for crisis situations. Anesthetists must be trained for situations that might never arise, attending simulation workshops with their work team, using their own resources to become familiar with their operation, and developing local management algorithms for critical situations. 29
Conclusions
Intubation in children under 1 year of age is more difficult, whereas older children are easier to approach using the appropriate maneuvers. Fortunately, it is easy to ventilate and oxygenate children with a facial mask, which is the cornerstone of management when difficulties approaching the airway arise, as long as adequate facial seal and a patent airway are achieved with manual CPAP. The pediatric airway is easy to classify and difficult cases may be readily anticipated with an active enquiry into the prior history, anatomic abnormalities, and physiological alterations. Several devices are available for approaching the airway. It is advisable to have a pediatric airway cart equipped with all the necessary items, develop local airway management algorithms, and train the surgical team by means of simulation workshops so that they can become familiar with their own resources.











 text in
text in