Introduction
The purpose of focused critical care echocardiography (FCCE)1,2 performed by expert cardiologists, as compared with conventional echocardiography, is early identification of hemodynamic changes in order to help with diagnostic, clinical, and therapeutic decision-making.3,4 This crucial information has been documented over the past 15 years by means of multiple studies in adults and children.1,3-6 According to the recommendations from the American Society of Echocardiography (ASE), quantitative measurements in FCCE are not necessary7 and their usefulness for research within the intensive care setting has not been demonstrated to date.
In Colombia, there are no formal training programs in FCCE addressed to pediatricians working in pediatric intensive care units (PICU) or pediatric intensivists, just as there are no studies documenting their performance. The objective of this study was to assess a 26-hour theory and practice FCCE training program addressed to pediatricians and pediatric intensivists working in a PICU. Moreover, it sought to achieve and document skills acquisition by correlating the performance of the trainees with that of the pediatric cardiologist acting as the gold standard, not only in terms of basic level image acquisition but also the ability to obtain some quantitative measurements that can be used in the clinical and research settings of pediatric critical care.
Methodology
Population
Practical training sessions were carried out in patients under 18 years of age admitted to the ICU of Hospital Cardiovascular del Niño de Cundinamarca (Children's Cardiovascular Hospital of Cundinamarca [Soacha, Colombia]), except in children with cardiac malformations or who were hemodynamically unstable. Healthy children of hospital employees were also included. Five pediatricians and 6 pediatric intensivists participated under the guidance of a pediatric cardiologist.
The parents of all the children subjected to echocardiography gave their informed consent. The study was approved by the institutional ethics and research committee of Hospital Cardiovascular del Niño de Cundinamarca as stated in Minutes No. 024 of December 23, 2017.
Training model and curricular content
Phase 1. Opening: Reading bibliographic material on basic echocardiography, FCCE and guidelines4,8-10 was provided 15 days before the start of the course. In addition, trainees received a document prepared by the authors of the training program containing principles of cardiovascular ultrasound, common imaging formats, basic echocardiographic planes (parasternal, apical, subcostal, and suprasternal), and a table with basic echocardiography measurements focused on critical care with their equation and windows. Five hours of self-learning were required.
Phase 2. Theoretical-practical course conducted by a pediatric intensive care cardiologist in 2 classroom sessions, as follows:
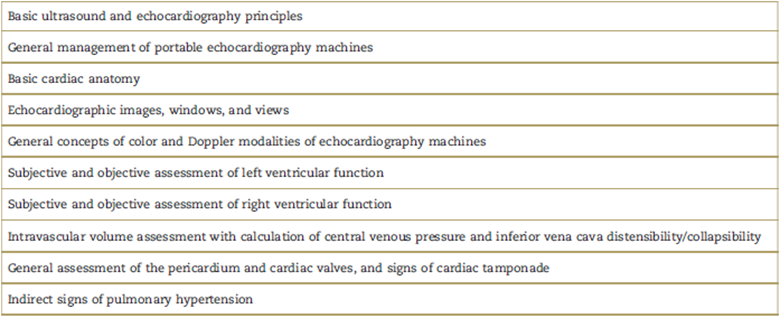
Six hours of theory (Table 1), based on the recommendations of the echocardiography and critical care societies.7,11,12
Six hours of practice under the supervision of a pediatric cardiologist expert in echocardiography, using 3 portable machines: Siemens Acuson CV70 (United States of America, © Copyright 2018 Let Medical Systems, Corp. Store), GE Vivid 7 Ultrasound System (General Electric, Healthcare), and Phillips Sonos 5500 (Philips Electronics North America Corporation). The trainees completed a total of 3 FCCEs and the session ended with the expert pediatric cardiologist performing a complete echocardiogram (Table 2).
Table 2 Practical training program.
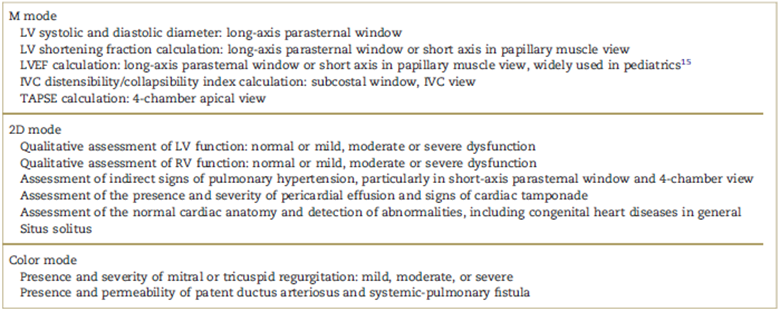
IVC=inferior vena cava, LV=left ventricle, LVEF=left ventricular ejection fraction, RV=right ventricle, TAPSE=tricuspid annular plane systolic excursion.
Source: Authors.
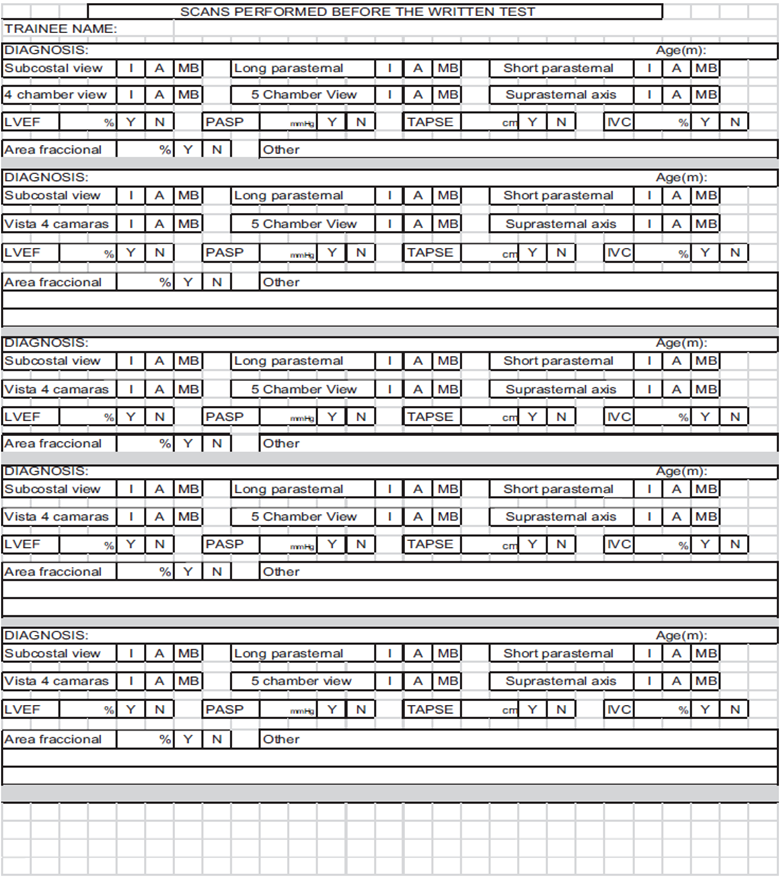
Phase 3. Performance of at least 20 echocardiography scans by the trainees (unsupervised) in patients admitted to the PICU; this number has been established in prior studies.13,14 At the end of this phase, trainees had to submit a log of practice echocardiograms which they received at the start of the training program (Annex 1). Scans could be repeated in the same patient at different points in time. A total of 4 weeks were devoted to this phase of the program.
Phase 4. The trainees went through a final practical examination under the supervision and evaluation of an expert pediatric cardiologist. Eligibility criteria for the final examination were completion of the 3 phases previously described, comprising the training syllabus. For this test, the trainees had to perform a complete FCCE with the 4 main echocardiographic windows, including the following measurements: inferred central venous pressure (CVP) based on inferior vena cava (IVC) diameter and its variability; IVC distensibility or collapsibility index (dIVC), taking into consideration whether the patient was on ventilation or not; tricuspid annular plane systolic excursion (TAPSE); and left ventricular ejection fraction (LVEF) on M mode, which is the most widely used in clinical practice, especially in pediatric patients15 (Table 3).
Table 3 Description of echocardiography variable measurements: CVP, TAPSE, dIVC, LVEF in M mode.
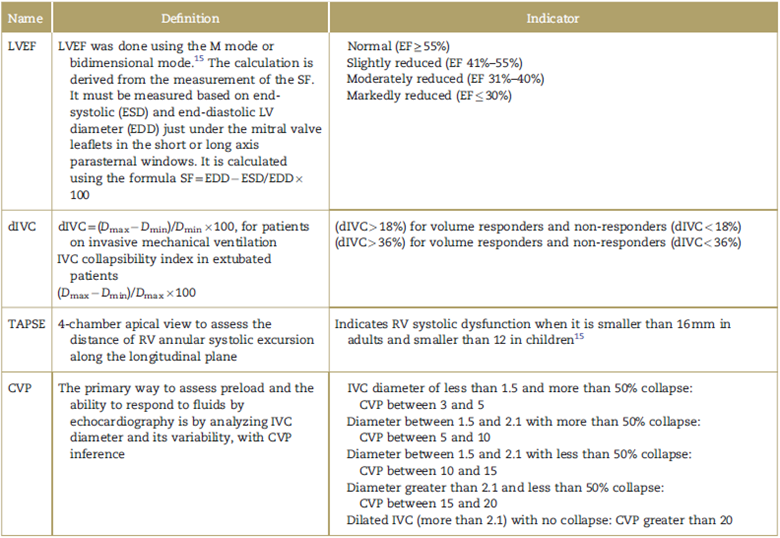
CVP=central venous pressure, dIVC distensibility index inferior vena cava, Dmax=maximum diameter, Dmin=minimum diameter, EDD=end-diastolic LV diameter, EF=ejection fraction, ESD=end systolic LV diameter, LV=left ventricle, LVEF=left ventricular ejection fraction, RV=right ventricle, SF= shortening fraction, TAPSE =tricuspid annular plane systolic excursion.
Source: Authors.
The scale developed by Gaudet et al14 was used for assessing the quality of the acquired images. The scale consists of 2 parts:
For the first part, each FCCE window is assessed against a checklist of the main structures that needed to be visualized and scored from 0 (failure to acquire the image or inadequate image or inadequate image for assessment) to 2 (optimum quality image). At the end of the checklist, the quality of the echocardiographic window is assessed in terms of gain, depth, and image centering.
For the second part, the diagnostic quality of the images is assessed in terms of the ability to review LV size and systolic function, right ventricular (RV) size and systolic function, intravascular volume, and presence of pericardial effusion. Each item allows a score of 0 for inadequate images for diagnostic assessment, 1 for borderline quality images, and 2 for adequate images for diagnostic assessment.14 On the Gaudet et al image acquisition assessment scale, trainee performance is calculated dividing the score obtained for each item over the maximum score possible, and expressed as a percentage.
In each of the patients in whom the trainees did their final practical examination, the expert pediatric cardiologist conducted a complete echocardiogram and measured the required qualitative variables, 15 minutes before the trainee. The quantitative measurements calculated by the trainees were compared to those of the expert pediatric cardiologist and the correlation was expressed as a percentage. Values above 80% were considered as a good level of correlation.
Data collection
Data regarding trainee characteristics were collected in an Excel spreadsheet (Microsoft Corporation, Redmond, WA). These included age, gender, level of education, prior training in echocardiography, number of echocardiograms performed before the practical examination, degree of satisfaction with the course following their FCCE training in terms of usefulness and applicability for their professional practice. The latter item was rated as "not useful", "somewhat useful", or "very useful".
Echocardiographic variables14 were entered as follows: score and performance in long-axis parasternal window (minimum 0 points, maximum 12 points); short-axis parasternal window (minimum 0 points, maximum 18 points); score and performance in apical 4-chamber window (minimum 0 points, maximum 10 points); score and performance in long-axis subcostal window (minimum 0 points, maximum 8 points); score and performance in subcostal echocardiographic window for inferior vena cava (minimum 0 points, maximum 8 points); score and image quality diagnostic yield (minimum 0 points, maximum 12 points); score and total performance on the Gaudet et al diagnostic image acquisition assessment scale (minimum 0 points, maximum 68 points); percentage of total performance on the Gaudet image assessment scale (minimum 0%, maximum, 100%). Performance was expressed as a percentage of trainee score χ 100/maxi-mum score.
The correlation between measurements by the trainee versus the pediatric cardiologist was recorded as follows: TAPSE; LVEF; CVP calculation inferred on the basis of caval diameter and its variation during the respiratory cycle; dIVC (minimum 0%, maximum 100%).
Statistical analysis
The Shapiro-Wilk normality test was performed, observing a symmetrical distribution of the data. Descriptive statistics were applied using proportion estimations and relative frequencies for categorical variables; and central trend measurements were used for continuous variables. The Student t test was used to compare continuous variables for independent samples. The following were used as predictive variables: having prior knowledge of echocardiography, level of education, and number of training echocardiograms performed before the final practical examination. The control variables selected were the scores obtained for each echocardiographic window (long-axis and short-axis parasternal window, apical 4-chamber window, and long-axis and IVC subcostal windows) and the correlation percentage obtained for each echocardiographic measurement in relation to the expert pediatric cardiologist (inferred CVP, dIVC, TAPSE, and LVEF). The Stata 8.0 (Stata Corporation, College Station, TX) and SPSS Statistics 23 software packages were used for all the analyses.
Results
A total of 11 trainees participated in the FCCE training, 5 (45.5%) pediatricians and 6 (54.5%) pediatric intensivists. Mean age was 39 years, with a range between 28 and 50. Of the study population, 45.5% or the total number of pediatric intensivists that went through the training, had prior knowledge of echocardiography (general knowledge and performance of pediatric echocardiograms) (Table 4).
Table 4 Characteristics of the participants in the training program.
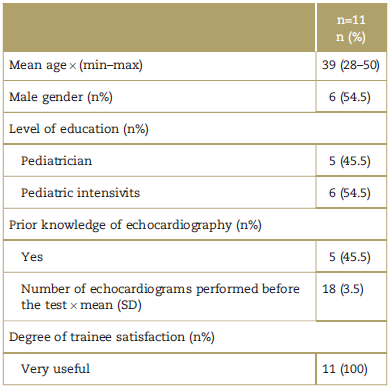
max=maximum, min=minimum, SD=standard deviation.
Source: Authors.
The course lasted 26 hours. During the training process, FCCEs were performed in a total of 198 PICU inpatients, with a mean of 18 echocardiographic scans per trainee. Not all students were able to perform all 20 echocardio-grams, because of the limited time period. Upon completion of the program, 100% of the participants rated it as very useful for their professional practice (Table 4). Overall, the training program resulted in high performance on the Gaudet et al image assessment scale, with a mean of 94.5%, and also a high average level of correlation for the measurements performed: 77.25% in relation to the expert pediatric cardiologist (Table 5).
Table 5 Trainee scores and performances in echocardiography image acquisitions.
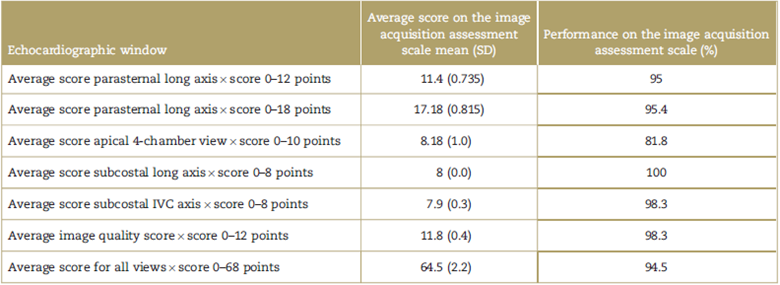
IVC=inferior vena cava, SD=standard deviation.
Source: Authors.
The echocardiographic windows for which the trainees obtained the best average score were the subcostal long-axis view and the subcostal window for the IVC, with performances of 100% and 98.3% on the scale, respectively. The window with the best average score and performance (81.8%) was the apical 4-chamber view (Table 5).
The echocardiographic measurement with the highest average correlation between the trainees and the expert pediatric cardiologist, and a good correlation (higher than 80%) was inferred CVP (100% of the trainees), followed by dIVC (81.8% of the trainees), TAPSE (72.7% of the trainees) and LVEF (54.5% of the trainees) (Table 6).
Table 6 Correlation for each echocardiography measurement between the trainees and the pediatric cardiologist.
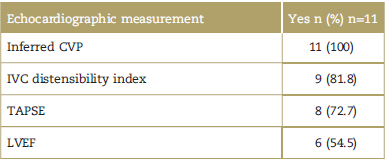
Note: Positive correlation defined as a correlation level higher than 80% for each echocardiographic measurement as compared to the intensive care pediatric cardiologist. %=percentage, CVP=central venous pressure, IVC= inferior vena cava, LVEF=left ventricular ejection fraction, n=number, TAPSE = tricuspid annular plane systolic excursion.
Source: Authors.
When continuous variables were compared using the Student t test, significant differences were found only between having prior knowledge of echocardiography and obtaining a higher score for the apical 4-chamber view (mean, 9.0; standard deviation [SD], 1.02 P = 0.021). This prior knowledge was associated also with improved correlation with the pediatric cardiologist for LVEF measurement (mean, 92.2; SD, 6.3; P=0.036). It was also found that a greater number of training echocardiograms (before taking the practical examination at the end of the course, with a mean of 18 echocardiograms per trainee) was associated with a higher score for the sum of all the views (mean, 65.3; SD, 1.9; P=0.038). Likewise, it was sufficient for obtaining some measurements for the assessment of intravascular volume and cardiac function, with more than an 80% correlation with the expert pediatric cardiologist (Table 5).
Discussion
In general terms, the 26-hour FCCE training program resulted in a very good average performance on the Gaudet et al14 image assessment scale, and very high correlation level for the various measurements with the expert pediatric cardiologist.
Studies published in recent years, including a few in pediatrics like the one by Gaspar et al,15 have documented that an average of 16 to 30 echocardiograms in training programs may be sufficient to achieve adequate and optimal FCCE performance.7,13,15,16 However, in this level proposed by the ASE, which is equivalent to the basic level of the American College of Chest Physicians/La Societé de Reanimation de Langue Française,7 the only goal is to train in the acquisition of echocardiographic images and qualitative assessment of cardiac function7; but a few studies,15,17,18 this included, have found that this number of echocardiograms has also been sufficient for obtaining some measurements to asses intravascular volume and cardiac function with a correlation level greater than 70% with the cardiologist and/or expert echocardiographer.
The observation is of great value for clinical and research work in intensive care. Hence, the proposal of expanding the objectives of the basic level of the American College of Chest Physicians/La Societé de Reanimation de Langue Française or of ASE level I, to include the calculation of these echocardiographic measurements. This will help optimize and obtain more objective answers and diagnoses with the bedside use of FCCE.
For people with prior experience, these types of programs may provide more expertise and help maintain their level of competency. In contrast, this study documented that 9 hours of real-time practice for pediatricians and pediatric intensivists doing FCCE resulted in a very good level of basic FCCE training and acquisition of some measurements for global cardiac function assessment.
The best performance was obtained with the subcostal long-axis window (98.75%), while the window with performances under 80% (81.8%) was the apical 4-chamber view (Table 5). It may be concluded that subcostal and parasternal views are the easiest to obtain and that the learning curve for acquiring an adequate 4-chamber view requires additional training and, consequently, a greater number of practical echocardiograms and longer training than used in this study (18 scans and 26 hours, respectively). The apical view has been recognized by the ASE as one of the most difficult echocardiographic windows to acquire, even for cardiologists in training.7
The echocardiographic measurements for which trainees achieved a correlation of more than 80% with the pediatric cardiologist, considered the easiest to learn, were inferred CVP, dIVC and TAPSE. The most difficult to learn, requiring more training was LVEF. The above shows that FCCE learning curve and skill improve with a greater number of echocardiographic scans and that more experience is required to improve performance in the 4-chamber view and the level of correlation for LVEF with the expert pediatric cardiologist.
RV dysfunction and failure has been recognized and studied more and more in the critical care setting; it is found to be an important morbidity and mortality factor in critically ill patients, affected not only by cardiovascular conditions but by the most frequent conditions seen in the ICU: acute respiratory distress syndrome, sepsis, and pulmonary embolism.18,19
The gold standard for measuring RV function in view of the complex geometry is nuclear magnetic resonance imaging, which is hardly of any use in the critical care setting, even less so if bedside real-time monitoring of the RV is required for target-guided therapy designed to optimize and improve RV function.20
TAPSE, together with RV fractional area change appeared to have validated these characteristics in recent years.20,21 The ASE7,8 considers that TAPSE may be obtained easily and is a measurement of longitudinal RV function. Although it only measures longitudinal function, it has been shown to have good correlation with techniques that assess global systolic RV function and must be part of the systematic assessment of the right cavities.8
The study explored, for the first time, the possibility of training for TAPSE measurement as part of the basic level FCCE curriculum, in order to assess the RV in the critical care setting. In average, it was the second best correlated measurement with the expert cardiologist, and the third for which a larger number of trainees achieved a level of correlation above 80% (8 out of 11 trainees). These findings suggest that TAPSE may be introduced as part of FCCE training as a useful and power tool for the quantitative assessment of RV systolic function.
Strengths
The study explored, for the first time, the possibility of teaching TAPSE measurement as part of the basic level FCCE curriculum to assess RV function in the critical care setting. This study is the first in Colombia to establish the learning curve during the entire training of pediatricians and pediatric intensivists. It shows that they are capable of performing FCCE in critically ill children and emphasizes that every time there are doubts about anatomic or functional abnormalities, the case must always be discussed and reassessed by a pediatric cardiologist.
Limitations
One of the main limitations was the small number of participants which did not allow a different type of analysis. The majority of trainees work in a PICU, with cardiovascular emphasis, and although they did not have prior knowledge in echocardiography, they have been exposed to it.
Conclusion
The training program was useful to achieve the basic FCCE level, with optimum performance in the acquisition of the main windows and some echocardiographic measurements to assess volemia, response to fluids and LV and RV function, following a 26-hour course and the performance of 18 echocardiographic scans during the practical component of the program.
An important contribution was the finding that, as part of the basic FCCE level of training, a very good level of correlation may be achieved for TAPSE, thus resulting in a more objective measurement of RV function and bedside monitoring of the RV. This type of training is the initial exploration of pediatric FCCE in Colombia for point-of-care academic, clinical and research purposes.
Ethical responsibilities
Human and animal protection. The authors declare that no experiments were conducted in humans or animals for this research.
Data confidentiality. The authors declare having followed the protocols of their institution regarding patient data disclosure.
Right to privacy and informed consent. The authors declare that not patient data appear in this article.











 text in
text in