Introduction
One of the most important goals on admission of a patient to the intensive care unit (ICU) is to ensure survival. However, it is crucial to preserve the best possible quality of life (QOL) in relation to the state of health of the patient.1-3 For survivors of the ICU, disease and limitations do not end in the hospital; length of stay and procedures do not only increase the mortality rate, but they also affect health-related QOL (HRQOL).4,5 Given the broad definition of QOL and the fact that quality-of-life concepts are not very tangible, this study refers to HRQOL, which developed as a subtype of "QOL", in order to restrict the spectrum of health-affected conditions, where 4 roles are assessed: physical, social, psychological/emotional, and cognitive.6 The Acute Physiology and Chronic Health Evaluation (APACHE) II score was taken into account to determine the severity of patients in the ICU.7 There is no literature in Colombia pertaining to the consequences of a stay in the ICU, creating a gap in medical knowledge. Therefore, the objective of this study was to assess QOL and mortality in patients over 50 years of age after discharge from an ICU.
Multiple standardized questionnaires are available for objective measurement of HRQOL, including EQ-5D-3L, which measures 5 parameters: mobility, self-care, pain/ discomfort, usual activities, and anxiety and depression. It also includes a final item that assesses subjective patient perception of QOL using an analogue scale. A total score is calculated based on the 5 dimensions and the analog scale, where a value of 1 is interpreted as the best possible QOL, and 0 as the worst.8 EQ5D was preferred over the SF36 and HAQ scores, considering that several studies have shown that it is easier to administer and interpret and the response rates are better.9,10 In addition, this tool has been validated to be applied over the phone to facilitate data collection. EuroQol was contacted to request permission for using the questionnaire in the Colombian population applying the same reference values used in Spain for estimating the final result.
Methodology
Analysis of a cross-sectional observational study in patients discharged from the ICU of the Manuel Uribe Ángel Hospital between January 2014 and December 2016. The study was approved by the ethics committee of the Hospital, as stated in Minutes No. 01 of March 9, 2017, and by CES University as stated in Minutes 108 of June 6, 2017. The verbal informed consent process was done with all patients between June 1, 2017, and July 31, 2017, and it consisted of reading a form that explained the purpose of the calls and asking them for their consent to analyze their data and their answers. The study was conducted in 100% of the population that met the inclusion criteria: being older than 50 years of age with a length of stay in the ICU of 48 hours or more and a complete clinical record (documentation of the etiology, the APACHE II score, gender, and the contact telephone number).11 Patients with more than 1 known admission to the ICU of the Manuel Uribe Ángel Hospital and those who died were excluded. The latter were taken into consideration only for demographic and mortality characteristics, considering that they could not be surveyed for QOL.
The Manuel Uribe Ángel Hospital has a 14-bed polyvalent unit with advanced technology and staff specialized in the management of critically ill patients. This ICU is licensed to provide specialized services to patients with various conditions managed by internal medicine, oncology, cardiovascular disease, pulmonology, neurology, neurosurgery, high-complexity surgery, among others. The main diagnoses are acute ventilatory failure associated with pulmonary or systemic infection, decompensated chronic obstructive pulmonary disease or other causes, septic shock, and sepsis, postoperative care following major surgery such as cardiovascular, neuro-surgery, thoracic surgery, oncologic surgery.
The demographic characteristics of all the patients were taken from the clinical record. Afterwards, during the period between June and August 2017, all the patients were contacted by telephone. The calls were made by 5 researchers using the same format: an explanation of the reason for the call, the objective of the study and the hospital involved, verbal informed consent process for the telephone survey and, finally, the administration of the EQ-5D-3L questionnaire. In cases of patients who had died, only the date of death was asked and documented for postdischarge mortality estimation.
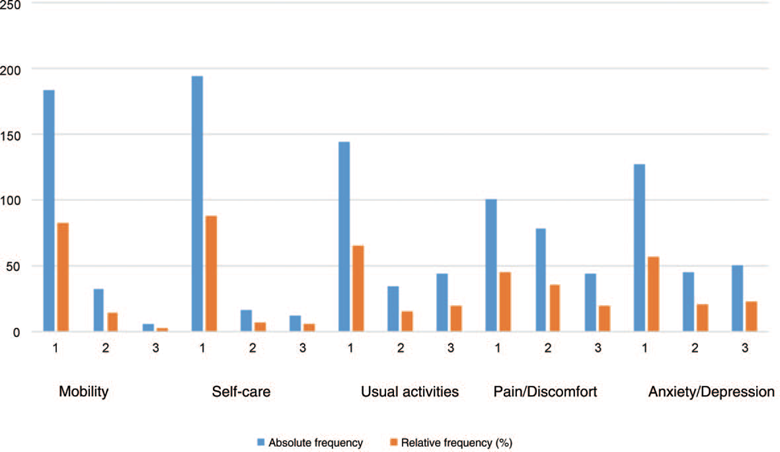
Table 1 Comparison between responders and non-responders of the EQ-5D-3L questionnaire.
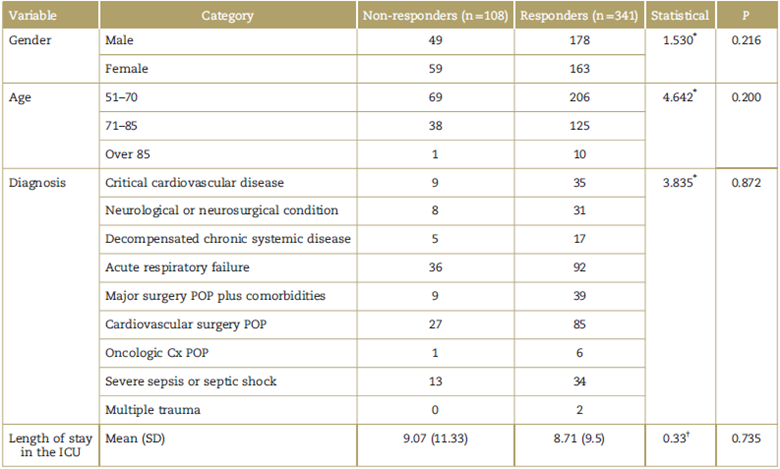
ICU=intensive care unit, POP=postoperative period, SD=standard deviation.
*Pearson χ2.
† Student t.
Source: Authors.
Data analysis
Data were entered in a Microsoft Office Excel 2010 database and they were processed using the SPSS version 21 software package (Statistical Package for the Social Sciences, manufactured by International Business Machines Corporation). A demographic analysis of the data was conducted and mortality following ICU stay was identified. A univariate and bivariate analysis was performed for each variable, using the Chi-square test for qualitative variables, Student's t test for quantitative variables with parametric distribution, and the Mann-Whitney U test for variables with non-parametric distribution.
In order to ensure that the population that was not contacted and the population that responded the questionnaire were similar, a comparison was made between mean lengths of stay in an ICU using Student's t test. Regarding demographic characteristics (gender, reason for admission, and age ranges), similarity was compared using the Pearson Chi-square test. The results in Table 1 show that there are no statistically significant differences in any of the characteristics assessed.
Results
Overall, 449 clinical records of patients who met the inclusion criteria were evaluated. It was not possible to contact 24.92% of these patients for different reasons, such as change of residence and wrong phone number. The statistical analysis of demographic characteristics, reasons for admission to the ICU and length of stay was done for the entire population that met the inclusion criteria (including those patients who could not be contacted and those who died later). Mortality was calculated taking into consideration 341 patients who were contacted; this number includes the patients who died after having spent time in an ICU and those who had not died yet at the time of the call and were able to answer the EQ-5D-3L survey (Fig. 1).
Regarding demographic characteristics (Table 2), 50.6% of patients (227) were females, mean age was 68.3 years (±9.62 years), mean length of stay in the ICU was 8.8 days (± 9.63 days), 68.4% (307) had an APACHE II score between 10 and 24; 28.5% (128) of the patients had acute respiratory failure as initial etiology, this being the most prevalent diagnosis at the time of admission.
Table 2 Demographic characteristics of patients admitted to the intensive care unit.
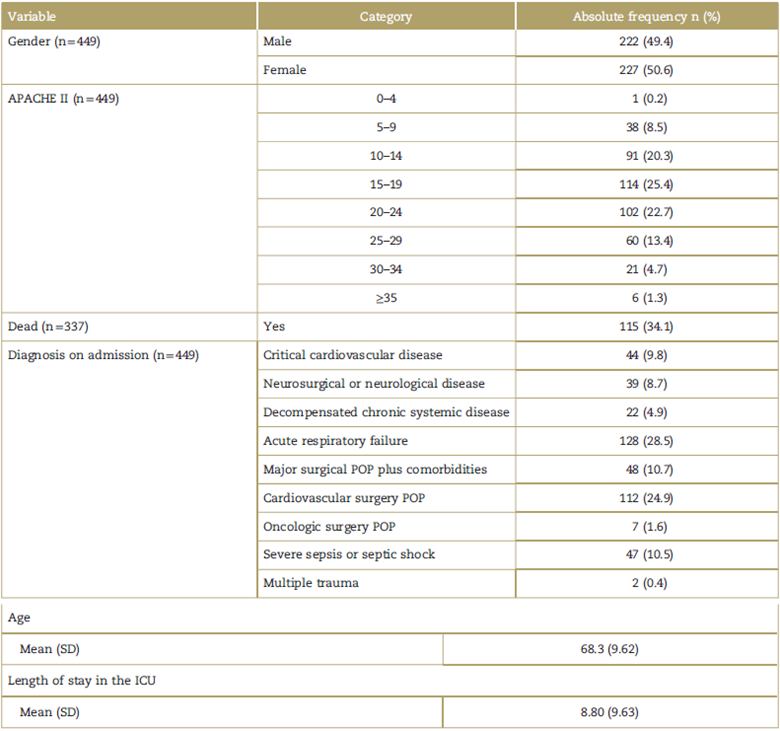
APACHE=acute physiology and chronic health evaluation, POP=postoperative period, SD=standard deviation. Source: Authors.
Regarding mortality, it was reported for 33.72% of the patients (115) out of the total who were contacted (341); of them, 25.21% (29) died within the first 30 days of discharge from the ICU; 36.52% (42) died between month 1 and month 6; 17.39% (20) died between month 6 and month 12; and 20.87% (24) died after the first year of discharge from the ICU. Given the high mortality, it was only possible to give the quality-of-life survey to the 222 remaining patients (49.44% of the original sample).
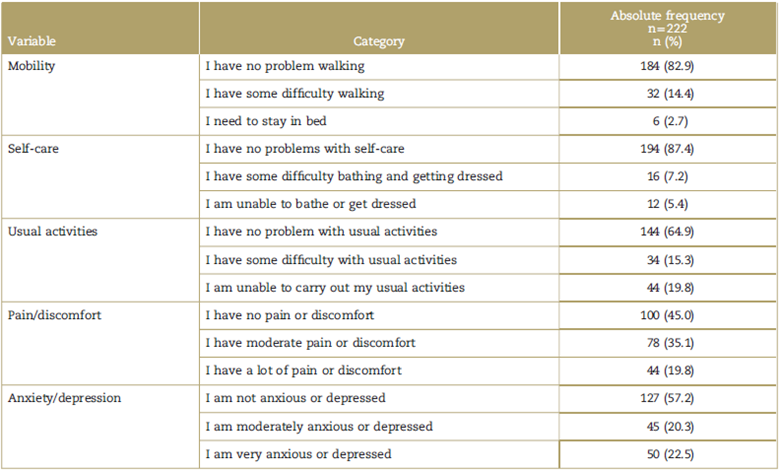
Regarding the EQ-5D-3L results (Table 3), the total mean for HRQOL was 0.68 for patients under 80 years of age, pain/ discomfort being the most affected domain with a mean score of 1.74 over 3, followed by 1.65 for anxiety/depression, and finally 1.49 for usual activities.
Table 3 Differentiation of health-related quality-of-life parameters analyzed using the EQ-5D-3L, by age range.
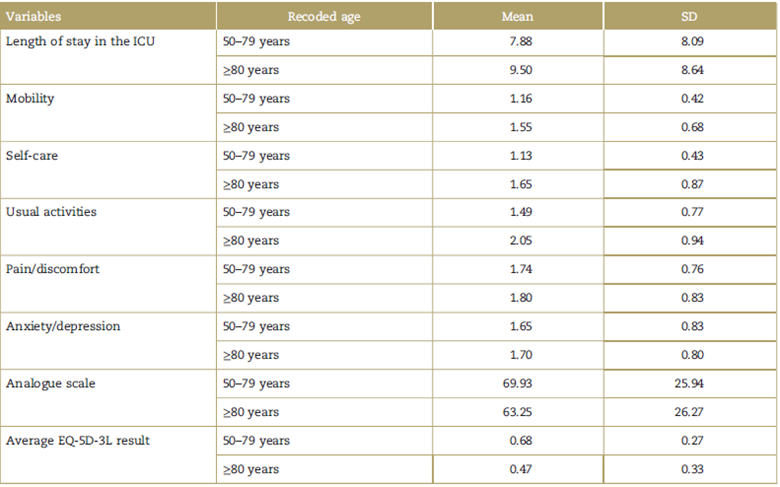
EQ-5D-3L parameters=mobility, self-care, usual activities, pain/discomfort and anxiety/depression. SD=standard deviation. Source: Authors.
In terms of the analog scale, the total average was 69.05%, 100% being the best QOL perceived by the patients. There was no evidence of a relationship between the analogue scale and gender (P = 0.720). For the group of patients over 80 the average result on the EQ-5D-3L was 0.47, the most affected domain being usual activities, with a mean score of 2.05 over 3, followed by pain/discomfort at 1.80. Regarding the analogue scale, the mean for this age group was 63.25%. In addition, a mean length of stay of 9.50 days was found.
According to the results on Table 4, for the pain/ discomfort domain, 54.9% of patients scored this item as moderately or severely affected. Regarding the anxiety/ depression domain, 42.8% of the patients gave a score of moderately or very anxious/depressed.
As shown on Table 5, the patients who had at least 1 non-affected domain on the EQ-5D-3L (score of 1), had a higher average on the visual analogue scale (P = 0.000 in all dimensions). A relationship was found between the length of stay in the ICU and the score for the self-care and usual activities dimensions, considering that longer stays in the ICU were associated with a score of 3 given by the patients to those items (P = 0.024 and 0.003, respectively). Moreover, a relationship was found between days in the ICU and the APACHE score (P = 0.020), showing that patients with APACHE > 35, had a longer stay.
Table 5 a. Associations between diagnosis on admission to the ICU, length of stay, EQ-5D-3L dimensions and analogue scale. b. APACHE, Lenght of stay in Critical Care and Age.
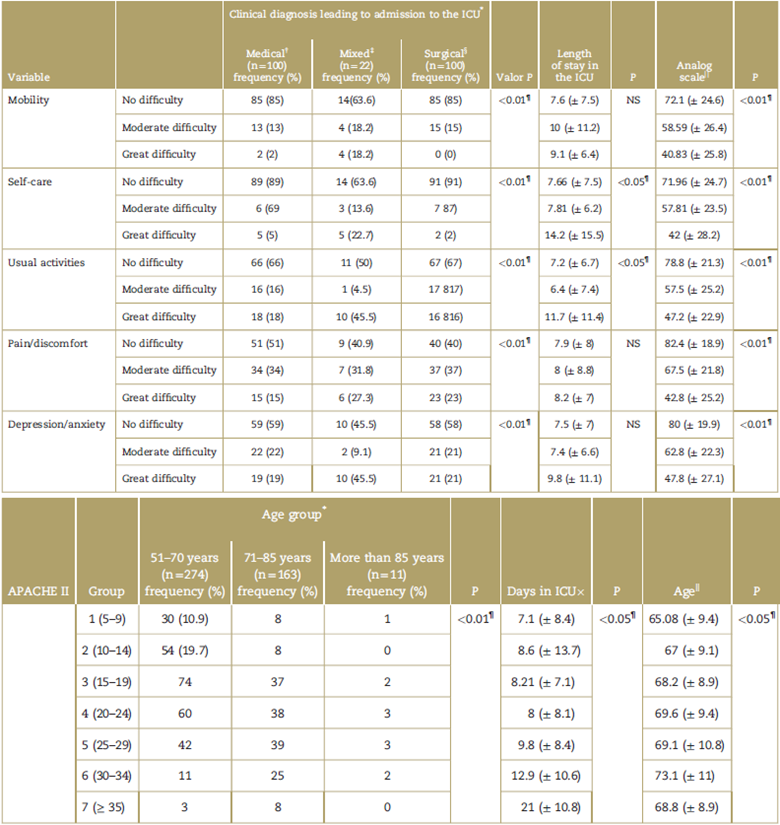
APACHE = acute physiology and chronic health evaluation, ICU=intensive care unit, NS=not significant, POP=postoperative period.
*Pearson χ2.
† Medical diagnosis included the following conditions: critical cardiovascular disease, decompensated chronic systemic disease, acute respiratory failure, severe sepsis or septic shock, multiple trauma.
‡Mixed diagnosis included the following conditions: neurological or neurosurgical disease.
§ Surgical diagnosis included the following procedures: POP Major surgery plus comorbidities, POP cardiovascular surgery, POP oncologic surgery
ll ANOVA, analysis of variance.
¶ P<0.05.
In addition, an association was found between APACHE score and age (P=0.027), the mean age for patients with APACHE ≥ 35 being 68.8 (± 8.9).
According to the data, there was an association (P = 0.013) between the etiology on admission and the mobility domain, the neurological or neurosurgical condition being the most commonly associated with a severe effect (score of 3). Likewise, a significant difference (P = 0.040) was found between the diagnosis and the self-care group, the most frequent diagnosis for patients with a no-effect or moderate effect score being postoperative stay after cardiovascular surgery (35.1% and 25%, respectively), and neurological or neurosurgical disease being the most common diagnosis in patients who scored this item as severe effect (41.7%).
Discussion
When compared to the general population, patients discharged from the ICU have a lower QOL and increased mortality during the first year, according to other researchers like Brinkman et al3 and Rydingsward et al12. Likewise, this study showed how there are determining factors for patient outcome, including early initiation of physical therapy, occupational therapy, patient age and functional status of the patient while in the ICU.
This study shows evidence that 1/3 of the patients die few months after leaving the hospital despite the treatment provided. Roch et al13 studied mortality in patients over 80 years of age following discharge from the ICU and found that the rate for the first year was 72% and the rate at 2 years was 79%. This might be related to the disease and the lack of patient conditioning, and it may be influenced by factors such as care after discharge and timely medical assessment, among other things.14
In a study conducted in the Netherlands with 91,203 patients, 1-year mortality was 12.5% after admission to an ICU. The study looked at patient subgroups according to the reason for hospital admission (elective surgery, urgent surgery, medical [non-surgical]), and based on the reason for admission to the ICU (cardiac surgery, subarachnoid hemorrhage, acute renal failure, community-acquired severe pneumonia, cancer and trauma).3 A similar study with 740 patients found 28% annual mortality based on variables analyzed retrospectively, namely, gender, age at the time of admission to the ICU, body mass index, APACHE, length of stay in the ICU, length of hospital stay, duration (in hours) of mechanical ventilation, type of admission (elective surgery, emergent surgery, or medical causes), presence of comorbidities, continuous venovenous hemofiltration, sepsis within the first 24hours of admission, and readmission to the ICU after initial treatment.15 A study in England found that 56% of patients admitted to intensive care died within the first year after discharge. All eligible patients had to have received at least 48 hours of grade 3 dependent care (critical care due to multi-system organ failure).4 When comparing these results with our study, it was found that 81.5% of the deaths happened in the first year after discharge, which is higher than the studies conducted in European countries. It is worth highlighting that the populations of 2 of the 3 studies mentioned above are similar to the population of this study.
Authors like Pintado et al found that 1-year mortality in patients with prolonged lengths of stay (>14 days) in an ICU was higher than in patients with a shorter length of stay (68.2% vs 41.2%). Moreover, they found a relationship between prolonged length of stay and severity of the condition on admission; this could explain the mortality figures found in our study, considering that more seriously ill patients had longer stays.16
In terms of HRQOL, total average on the EQ-5D-3L was 0.65. This result might be explained by multiple variables such as length of stay in the ICU, patient age, comorbidities, socioeconomic condition, among others.17 Bearing in mind the severity of the conditions that require admission to the ICU, a low total average on the analogue scale would be expected, given that patients are generally left with notorious limitations for daily life.18
Regarding patients over 80 years of age, HRQOL is lower compared with the general group (0.4793 vs 0.65, respectively). It is striking that the most affected category in these patients is usual activities (2.05 over 3). In addition, differences are found between the 2 groups on the analogue scale (60.23% vs 68.9%, respectively).
Patient severity index on admission to the ICU was measured using the APACHE II score. Our study found that patients with a high APACHE (≥35) had longer stays in the unit (P = 0.020), a finding that has been shown in several studies.19-21 Likewise, mean age in these patients was 68.8 (± 8.9). The study by Khouli et al22 found that mortality predictors following stay in an ICU included high APACHE II score. Given the severity of the patients treated in this intensive care center, in-hospital/out-of-hospital mortality is high. In general, mean APACHE score at the time of admission was higher than in other centers with a non-polyvalent ICU. Moreover, patients in this hospital come from a low socioeconomic bracket, which means that the baseline health status is usually lower than for patients in other private centers.18
This study shows that the most affected dimensions on the EQ-5D-3L were pain/discomfort and anxiety/depression. These results were lower than those reported by Griffiths et al, (2013) who showed that 73% and 70% of the patients had severe pain at 6 months and 12 months after discharge, respectively. In addition, the same study also found that 46% and 44% of the patients had anxiety/ depression after 6 and 12 months, respectively.4
In their study, Griffiths et al (2013) found that 25% of patients were unable to perform usual activities on their own during the first 6 months, and 22% continued to have limitations in this dimension after 12 months. In our study, 9.8% of the patients were designated as "unable to perform usual activities".
In addition, a study in which the EQ5D tool was used together with the visual analogue scale to assess happiness found that the performance of this tool is good and cost-effective to assess healthcare-related QOL but not so for assessing happiness in these patients.23
Conclusion
Mortality following discharge from the ICU was 33.72%, with a higher proportion between 1 and 6 months.
In terms of HRQOL, the average for the general group was 0.65, showing that these patients are affected to a real degree. It is worth highlighting that the average was lower for patients over 80 years of age.
The most affected categories in the general group were pain/discomfort followed by anxiety/depression, whereas in the group of patients over 80 years of age, the most affected dimensions were usual activities followed by pain/ discomfort.
These values ought to be taken into consideration at the time of discharge in order to offer an assessment of the emotional condition together with effective pain therapy aimed at reducing the impact of the effect of these dimensions on perceived HRQOL.
In terms of the analog scale, the average of the general group and the group over 80 years of age was 67.8% and 63.25%, respectively, and the results were worse for patients with higher APACHE II scores and longer stays.
Considering that no study of this type done in Colombia was found as a result of the search conducted in the literature by the researchers, this is the first step in the exploration of the outcome of these patients in this country.
Additional prospective studies comparing QOL before and after discharge from the ICU are needed in order to have a more adequate determination of the general health condition of these patients and the impact of this kind of hospitalization on their QOL.
Future clinical trials to assess the value of adequate early physical, nutritional, and rehabilitation therapy during the stay and discharge of the ICU could have a positive impact on mortality and QOL outcomes in these patients.
Ethical responsibility
The protocol was approved by the ethics committee of Universidad CES in the category of "lower than minimum risk research" pursuant to Resolution No. 8430 of 1993 of the Colombian Ministry of Health, ensuring data confidentiality in accordance with the principle of the Declaration of Helsinki. The study was approved by the ethics committee of Hospital Manuel Uribe Ángel Acta (Minutes No. 01 of March 09, 2017), and by Universidad CES (Minutes No. 108 of June 6, 2017). The informed consent process was carried out by telephone to avoid unnecessary patient travel and additional costs.
Human and animal protection: The authors declare that no experiments were conducted in humans or animals for this research.
Data confidentiality: The authors declare having followed the protocols of their institution regarding disclosure of patient information.
Right to privacy and informed consent: The authors obtained the informed consent of the patients and/or subjects reported in this article. This document is kept by the corresponding author.











 text in
text in