Introduction
Several studies have determined the role of lactate elevation and its clearance as predictors of mortality and stay in the intensive care unit (ICU) in cases of sepsis, cardiopulmonary resuscitation, severe burns. Blood lactate levels above 2 mmol/L are proposed as an early and reliable marker of tissue hypoperfusion and, therefore, their measurement would be useful in critically ill patients at risk of developing shock due to any etiology.1-4 It has also been postulated that clearance of lactate levels during resuscitation is a prognostic marker that indicates the patient's response to treatment. Persistently elevated lactate seems to be associated with mortality and prolonged hospital stay in trauma patients.5-7
The objective of this study was to prospectively determine the association of the initial lactate value with mortality, and its clearance after 6 and 24hours, in a group of trauma patients.
Materials and methods
Subanalysis of a prospective cohort collected from March 2014 to October 2016 at the Hospital Universitario San Vicente Fundación-HUSVF-(Medellín, Colombia). This is a high complexity university hospital with 672 beds, 173 beds of intensive and intermediate care and 11,905 annual trauma consultations. The study was approved by the bioethics committee of the Institute of Medical Research of the Faculty of Medicine-Universidad de Antioquia through act No. 008 of May 17, 2012 and the committee of ethics of the HUSVF research through act No. 15-2013 of December 13, 2013. The informed consent was obtained in writing by each patient or his representative. The study was conducted in accordance with the ethical principles for medical research in human beings (Declaration of Helsinki of the World Medical Association). It was financed by the Science, Technology and Innovation Institute-Colciencias-(code 111556933334) and the Universidad de Antioquia.
Patients over 18 years old with multiple trauma defined as the involvement of 2 or more areas (head, face, extremities, thorax, abdomen, or soft tissues), were included. Burn patients should have confirmed second degree with 20% of the compromised body area, or third degree burns with 10% of the body area involved. In addition, the collection of information corresponding to vital signs and physical findings of the patients had to be carried out by the trained personnel of the project within the first 6 hours of admission to the hospital. Referred patients or hospitalized in another institution for more than 24 hours before admission, discharge or remission in the first 24hours of admission, diseases that prevent the standardized taking of clinical parameters (amputation, burns, extensive skin diseases in upper limbs), Raynaud's phenomenon or peripheral arterial disease, denial of the patient/family member/attending physician, screening after 6hours of admission to the institution, previous participation in the study and non-resuscitation orders were excluded.
Standardized measurements were made by nurses belonging to the study, for the following signs upon admission, 6 and 24 hours after the beginning of emergency treatment: capillary refill time, heart rate (HR), systolic pressure, diastolic pressure, pulse pressure, mean arterial pressure, shock rate, respiratory rate, and temperature. Simultaneously with the clinical evaluation, blood samples were taken for lactate measurement in the same periods of time, and the scores were calculated: Charlson Index-which estimates 10-year survival according to comorbidities-Acute Physiology and Chronic Health Evaluation II (APACHE II); the sequential organ failure assessment (SOFA); and Revised Trauma Score (RTS).8-10
Lactate serum was determined with the Lactic Acid assay ARCHITECT c Systems and AEROSET System (Reference 9D89-20; Abbott Laboratories, Chicago, IL). The detection limit is 0.05mg/dL and its inaccuracy is ±6.3% of the variation coefficient. Results were converted from mg/dL to mmol/L following the following equation, according to the manufacturer's instructions: mmol/L= mg/dL χ k (where k: 0.111). The outcome evaluated was inhospital mortality up to day 28.
Statistical methods
To estimate the association between the outcome of hospital mortality and the initial values of lactate and its clearance, several univariate, and multivariable logistic regression models were adjusted. Finally, a multivariate logistic regression model adjusted by trauma mechanism, RTS score, Sequential Organ Failure Assessment (SOFA), APACHE II, shock rate, lactate on admission, clearance of 10% lactate between admission and 6hours (1=second) was performed. Lactate value equal to or greater than 90% of the first, 0 = second lactate value less than 90% of the first, 50% lactate clearance between admittance and 24 hours (1 = third lactate value equal or higher 50% of the first, 0 = third lactate value less than 50% of the first).
The missing data for APACHE II and SOFA, approximately 5%, were assumed to be normal. Lactate variables at admission, 6 and 24hours had a shortage of 15,19, and 24 observations, respectively, for which a multiple imputation technique was performed with 100 iterations taking into account the variables of age, sex, RTS score, Charlson index, SOFA score, APACHE II score and type of trauma, so as to guarantee the best estimator close to the true parameter of the variables.
Results
During the recruitment period, 494 trauma patients were evaluated, of which 251 met the inclusion criteria (Fig. 1).
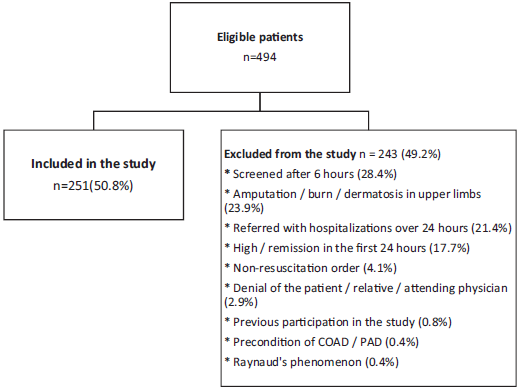
Source: Authors.
Figure 1 Study population. COAD = chronic occlusive arterial disease, PAD = peripheral arterial disease.
The median age was 33 years (interquartile range (IQR)= 26-47), being higher in patients who died (44 years, IQR = 29-51); 90% were men (n=226). The median Charlson index was 0 (IQR=0-0), SOFA was 2 (IQR = 1-6), being almost 3 times higher in the deceased (7, IRQ = 5-9) and APACHE II of 8 (IQR=4-14), being twice the value in deceased patients (16, IQR = 13-21). In the first 24hours they received 4060 cm3 of intravenous fluids (IQR = 3000-6500). Patients who died received more than 2000 additional cm3. 25.1% of the cohort (n=63) required the use of vasopressors and in 41.3% (n=26) of them a combination of 2 medications was used, 31.9% of the patients were transfused with a higher percentage in patients who died 53.9%. 50% of the patients were transfused with 4 units of blood products, in general venous saturation was 96% without differences between the groups, with a greater percentage in patients who died. 45.4% (n=114) of the participants required admission to intensive care. The median stay in the ICU and hospital stay was 5 days (IQR=2-10) and 7 days (IQR=3-16), respectively. Mortality was 15.5% (n=39). 58.2% (146) of the included patients presented penetrating injuries, 12 (30.8%) of them died and 41.8% (105) patients presented closed trauma, the mortality in this group was 69.2% (Table 1).
Table 1 Clinical characteristics and clinical course.
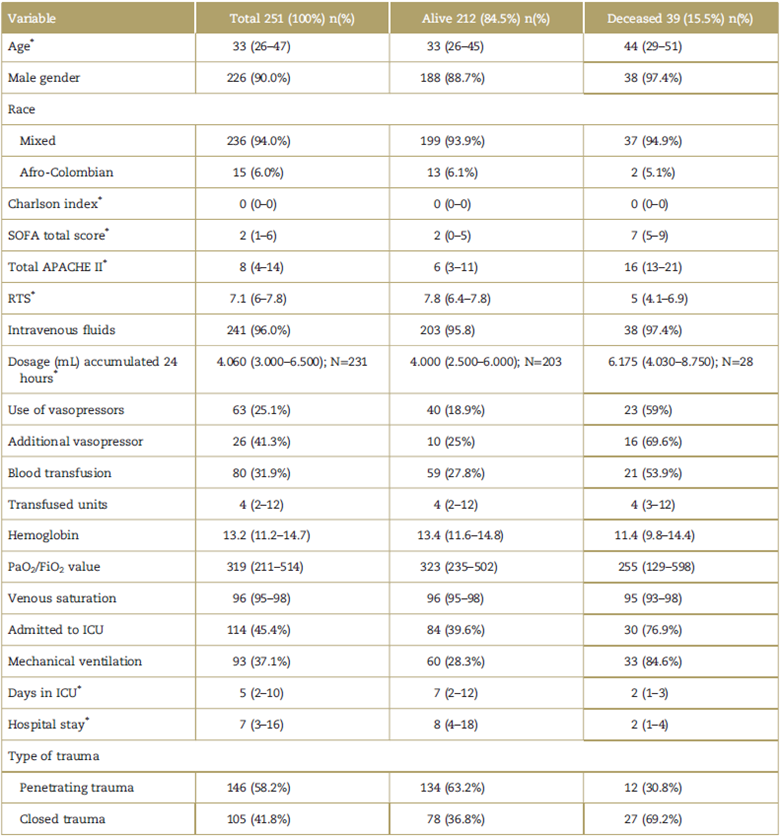
APACHE II=Acute Physiology and Chronic Health Evaluation II, ICU=intensive care unit, RTS=Revised Trauma Score, SOFA=Sequential Organ Failure Assessment.
*Median (interquartile range).
Source: Authors.
Traumatized patients who died had higher capillary refill values 2.9 seconds, (IQR = 2-3.7) versus 2.1 in those who survived (IQR = 1.8-2.9), as well as lactate values on admission 4.6 mmol (IQR=2.9-6.9) versus 3.7 in those who survived (IQR = 2.5-5.3), the same sequence is maintained for the measurements taken at 6 and 24 hours, as shown in Table 2.
Table 2 Clinical variables at 0 hour and vital status at discharge.
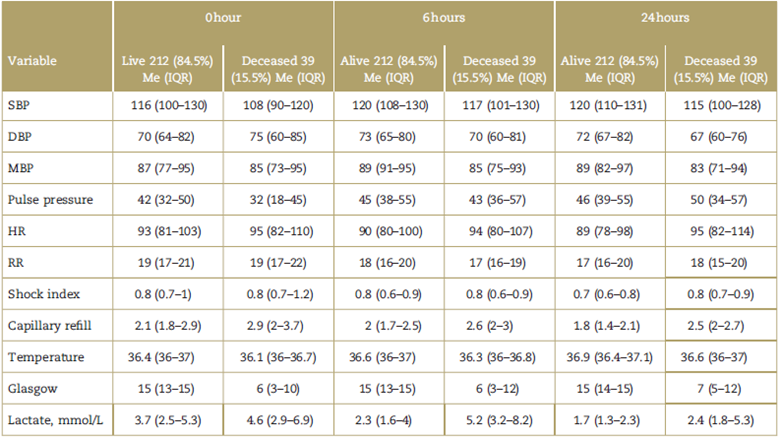
Me (IQR)=Median (interquartile range). HR=heart rate, RR=respiratory rate, MBP=mean blood pressure, DBP=diastolic blood pressure, SBP=systolic blood pressure.
Source: Authors.
Table 3 describes the lactate change, capillary refill, and shock index between the 0 to 6 and 0 to 24hours. The patients who died cleared less lactate (delta -0.4, IQR = -20.8, vs 0.8, IQR = -0.2-2.1 among survivors), did not improve capillary refill (delta -0.09, IQR = -0.2-0.3, vs 0.2 IQR=-0.1-0.5 among survivors), nor the shock index (delta 0.01, IQR=-0.06-0.14 vs 0.03, IQR=-0.05-0.17).
Table 3 Differences between living and deceased with respect to changes in lactate, capillary refill, and shock index.
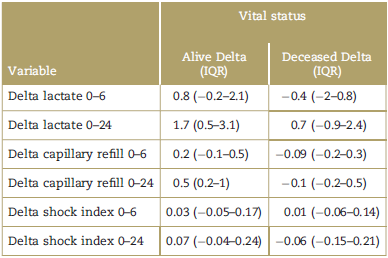
Delta was calculated by subtracting the second or third measurement from the first measurement.
IQR=Interquartilic range
Source: Authors.
In the univariate analysis, lactate at admission, non-depuration of 10% and 50%, trauma mechanism, RTS, SOFA, and APACHE II scores were associated with mortality. When performing the multivariate analysis, only the association with non-clearance of lactate of 50% (0-24 hours) and SOFA score was maintained (Table 4).
Table 4 Univariate and multivariate analysis for mortality with respect to the first measurement of the variables.
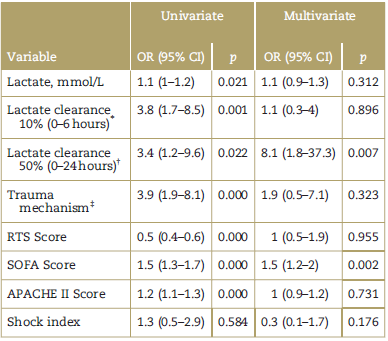
APACHE II=Acute Physiology and Chronic Health Evaluation II, CI = confidence interval, OR=odds ratio, RTS = Revised Trauma Score, SOFA= Sequential Organ Failure Assessment.
*Clearance of 10% between the initial lactate and that of 6hours; 1. No clearance of 10% between the initial lactate and that of 6hours.
† 50% clearance between the initial and 24-hour lactate; 1. No 50% clearance between the initial lactate and the 24-hour lactate.
‡ Penetrating; 1. Closed.
Source: Authors.
Taking into account that the lactate variables at admission, 6 and 24hours presented some missing data, an analysis was made with the imputed data finding that the adjusted model the lactate at admission, non-clearance of lactate of 50% (0-24hours), the trauma mechanism, and the SOFA score were independent factors associated with mortality (Table 5).
Table 5 Univariate and multivariate analysis for mortality with respect to the first measurement of the variables (imputed lactate).
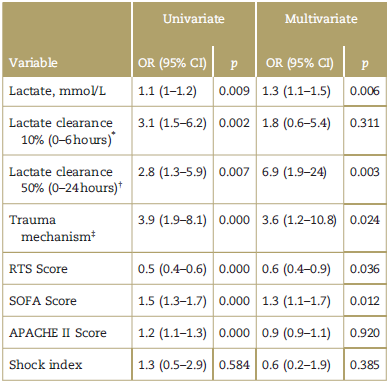
APACHE II=Acute Physiology and Chronic Health Evaluation II, RTS= Revised Trauma Score, SOFA=Sequential Organ Failure Assessment.
*Clearance of 10% between the initial lactate and that of 6 hours; 1. No Clearance of 10% between the initial lactate and that of 6hours.
† 50% Clearance between the initial and 24-hour lactate; 1. No 50% clearance between the initial lactate and the 24-hour lactate.
‡ Penetrating; 1. Closed.
Source: Authors.
Discussion
Shock is defined as a state of cellular and tissue hypoxia due to an imbalance between delivery and oxygen consumption or inadequate utilization,11 when the oxygen supply falls below a critical threshold, and it is not possible to satisfy the needs of the cells. This imbalance results in a cellular hypoxia, the energy metabolism becomes totally dependent on anaerobic glycolysis. Anaerobic glycolysis sharply increases the production of cellular lactate, which diffuses in the blood during prolonged ischemia of the cells. Therefore, high concentration of circulating lactate often indicates inadequate tissue oxygenation due to lack of supply and/or oxygen consumption.
Multiple trauma patients present alterations in systolic blood pressure and HR and a variable degree of tissue hypoperfusion, increased anaerobic metabolism, and metabolic acidosis; even in the presence of compensated shock.
This study corresponds to an evaluation of the prognostic significance of lactate in patients with trauma in a HUSVF cohort of Medellin over a period of 31 months.
The lactate measured at admission was evaluated as a biomarker of tissue hypoxia in trauma and its clearance during the first 24hours of hospitalization.
In the subgroup of infection of this same cohort, Londoño et al12 failed to demonstrate a correlation between the clinical findings of hypoperfusion demonstrated at physical examination and lactate values; and found lactate value at admission as an independent prognostic marker for mortality, indicating the importance of knowing the lactate value to guide resuscitation goals.
In a study published in this same journal13 in a prospective cohort of 196 patients diagnosed with hemorrhagic shock, lactate was measured at admission and 6 hours in addition to other clinical variables. When lactate serum clearance was less than 20% at 6hours, was found to be a risk factor for mortality. In our study, we found that the initial lactate value can discriminate by itself, the severity of the patients, being an independent prognostic marker for mortality (Odds ratio (OR) = 1.1, 95% confidence interval (CI): 1-1.2) and non-clearance of at least 10% at 6 hours has an OR of 3.8 (95% CI: 1.7-8.5) for risk of death, variables that can provide additional prognostic information in this type of patients.
Several studies have evaluated the prognostic value of lactate and its clearance in multiple trauma patients: Brown et al14 measured plasma lactate value in 1168 patients transported by helicopter to a level I trauma center and found that the median lactate was higher in patients who died compared with survivors 3.8 versus 2.3 (P < 0.05), in our study the median was higher 4.6 versus 3.7, but it is consistent with what was found by these authors.
It has been postulated that the use of alcohol and vasoactive substances induce metabolic acidosis which decreases the value of lactate and Base Excess measurements to predict mortality in trauma patients. Dunne et al15 prospectively evaluated a cohort of 15,179 patients and confirmed that the lactate and Excess base values are independent predictors of mortality in trauma patients and the consumption of alcohol and vasoactive substances do not modify their predictive capacity for death, ICU stay and hospital stay.
Ouellet et al16 retrospectively analyzed a cohort of 449 closed trauma patients and found that those who died had a greater median value of lactate than survivors (3.5 vs 2.2 P <0.05). In our study of the 105 patients with closed trauma, we also found a higher median in the deceased patients compared that of survivors (4 vs 3.8).
We found that the initial value of lactate levels provides important prognostic information superior to clinical signs in a broad spectrum of trauma patients. The information from previous reports that the lactate value at admission is strongly related to mortality in traumatized patients is confirmed in this group. In the univariate analysis, the association of the trauma mechanism, lower RTS score, higher values of SOFA, and APACHE with mortality were also found.
Recently, a systematic review was published that sought to determine the value of the measurement of lactate levels taken on admission to emergency services in trauma patients, recruiting 44,154 patients from 28 studies. This review showed an association of high lactate values on admission with the risk of dying and probably with other outcomes such as hospitalization time, ICU time, use of vasopressors, transfused blood units, and organ failure.17
Some studies have also evaluated the prognostic value of lactate clearance in traumatized patients. Odom et al7 evaluated the lactate values at admission and their clearance after adjusting severity scales in a group of trauma patients. Lactate was divided into 3 groups as follows: normal (less than 2.5 mmol/L, between 2.5 and 3.9 mmol/L, and 4 or more mmol/L). Clearance at 6 hours was also subdivided in groups, as follows: 60% or more, 30% to 59%, and less than 30% In this study, patients with high lactate at admission were found to have higher mortality. Adjusted by age and Injury Severity Score, the initial lactate level was a predictor of mortality, being significantly higher in patients with lactate higher than 4 mmol/ L. Clearance was also subdivided into groups. Patients whose lactate cleared by 60% or more of its initial level, had lower mortality than those with 30% or less7 In our study, we found that the 50% non-clearance between the initial lactate and the 24-hour lactate increased the risk of dying by 2.8 times more than in those who achieved this clearance (95% CI: 1.3-5.9), and when adjusted for variables such as trauma mechanism, RTS score, SOFA score, APACHE II score, and shock the risk is even higher (OR 6.9, 95% CI: 1.9-24).
Another study with 586 traumatized patients, 84% with closed trauma and 16% with penetrating trauma, found that higher lactate levels at admission correlated with higher mortality. The patients whose lactate cleared less than 20% of their initial lactate value in the first 2hours, had a worse result.6
We also found that among patients with high initial lactate and clearance measured at 6 and 24hours, closed trauma, SOFA, APACHE II, RTS scores are prognostic factors for mortality in trauma patients. In the multi-variate analysis, independent prognostic factors associated with mortality were the lactate values at admission, 50% non-clearance at 24hours, the trauma mechanism and SOFA score. Oliveros-Rodríguez et al,18 in an observational study in 233 trauma patients admitted to the ICU between 2010 and 2014, found a greater capacity to discriminate lactate when it remains elevated over 2.35mmol/L at 24hours with an OR of 1.65 (95% CI: 1.27-2.13).
Gonzalez et al conducted a systematic literature review to evaluate lactate clearance as a prognostic factor in penetrating trauma, selected 6 papers that included 350 patients, found a heterogeneity in the populations included in the studies and in the therapeutic interventions and that the value of lactate clearance in trauma patients is not standardized. The conclusion of the review was that persistently elevated lactate seems to increase mortality and hospital stay in this population.19
There are some methodological considerations about this work. Although the spectrum of patients recruited is broad, the selection was done through convenience sampling and the group does not necessarily represent patients with more severe lesions or in a higher state of hypovolemic shock which limits the applicability of the findings. Another limitation, given the sample size, was the inability to establish subgroups according to the trauma mechanism. Finally, some conditions that could affect the clearance of lactate such as liver or kidney involvement were not considered.
In conclusion, we demonstrate in a prospective cohort of trauma patients that high lactate values at admission are associated with a higher probability of dying, and that in those who enter with high lactate values, clearance is an independent predictor of death.
Ethical responsibilities
Protection of people and animals: The authors declare that no experiments have been carried out on humans or animals for this research.
Data confidentiality: The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent: The authors declare that patient data does not appear in this article.











 text in
text in 


