Introduction
Arthroscopy is an ambulatory, minimally invasive, and useful technique for managing most pathological and trauma lesions of the knee.1-3 Through 2 or 3 ports or incisions, the injured tissue is repaired. This procedure may be conducted under general, regional, or local anesthesia.4
Postoperative pain control is a crucial clinical factor for the recovery of the patient, since pain limits adequate rehabilitation and resuming of daily activities,5,6 with subsequent social and economic impact, not just for the patient, but also for the healthcare system.7
There are different techniques for regional anesthesia, based on the site of administration of the local anesthetic (LA) agents, and 2 of these are: sciatic-femoral peripheral nerve block (SFNB) and spinal anesthesia (SA) administered with bupivacaine as the only LA. These techniques have been used in daily practice of anesthesiology and orthopedics for the last decades, specially due to the lower incidence of complications, greater convenience, and usefulness.8
SA is considered to be safe, though not risk-free.9 One of its advantages is easier administration and patient comfort; however, some disadvantages have been described, such as puncture site pain, post-puncture headache, urinary retention, and a high level of nerve block that compromises the heart rate (HR). This technique requires longer patient isolation time and delays the start of the surgical procedure.10
The sciatic-femoral nerve block technique requires the localization of the site of needle insertion using anatomical landmarks, and neurostimulation or ultrasound-guided support,11,12 as indicated in some studies.13 The SFNB is effective for controlling postoperative pain,14 and some of its advantages include lesser hemodynamic changes, and preserved intestinal and bladder function, with a lower risk of neuro-infectious complications.15 Some of the disadvantages described are the time required for administration, and the need of technologies to guide the placement of the LA agent, the development of hematomas, and potential HR alterations.16,17
There is currently a controversy around the selection of the anesthetic technique for knee arthroscopy,18,19 in search of effectiveness, safety, patient satisfaction, and practitioner comfort. However, in clinical practice there is a preference for bupivacaine as the LA of choice for these techniques,20 but over the last few decades, the combination between LAs and the peripheral nerve block technique has emerged, in the quest for postoperative management that favors early rehabilitation21 and less adverse events such as bladder globus and postoperative joint pain that requires rescue analgesia.
Due to the rapid administration and therefore, shorter time to start surgery, some anesthesiologists prefer SA with bupivacaine22, which is a long-lasting LA agent that provides up to 6hours range for the surgical procedure. No instances of decreased levels of hemoglobin in blood have been described and allergic reactions are minor, as compared against other LA agents. However, the presence of other adverse events and limitations such as anatomical alterations of the lumbosacral spine, mostly in elderly patients, increases the use of peripheral nerve blocks20 that have anatomical landmarks for ease of administration and better postoperative pain control.
In view of the clinical practice heterogeneity, the authors conducted this systematic review (SR) with a view to establishing the effectiveness and the safety during the postoperative period of adult patients undergoing arthroscopic knee surgery, using exclusive spinal analgesia with bupivacaine, as compared with sciatic-femoral nerve block.
Method
Eligibility criteria
The Randomized Clinical Trials (RTC) considered included adult population having undergone knee arthroscopy using SA or sciatic-femoral nerve block as the comparator, excluding any trials using an anesthetic agent other than bupivacaine in SA and nerve block other than sciatic-femoral nerve block, simultaneously.
The primary outcomes evaluated were effectiveness, safety of anesthesia, and patient satisfaction.
Search methods to identify the trials
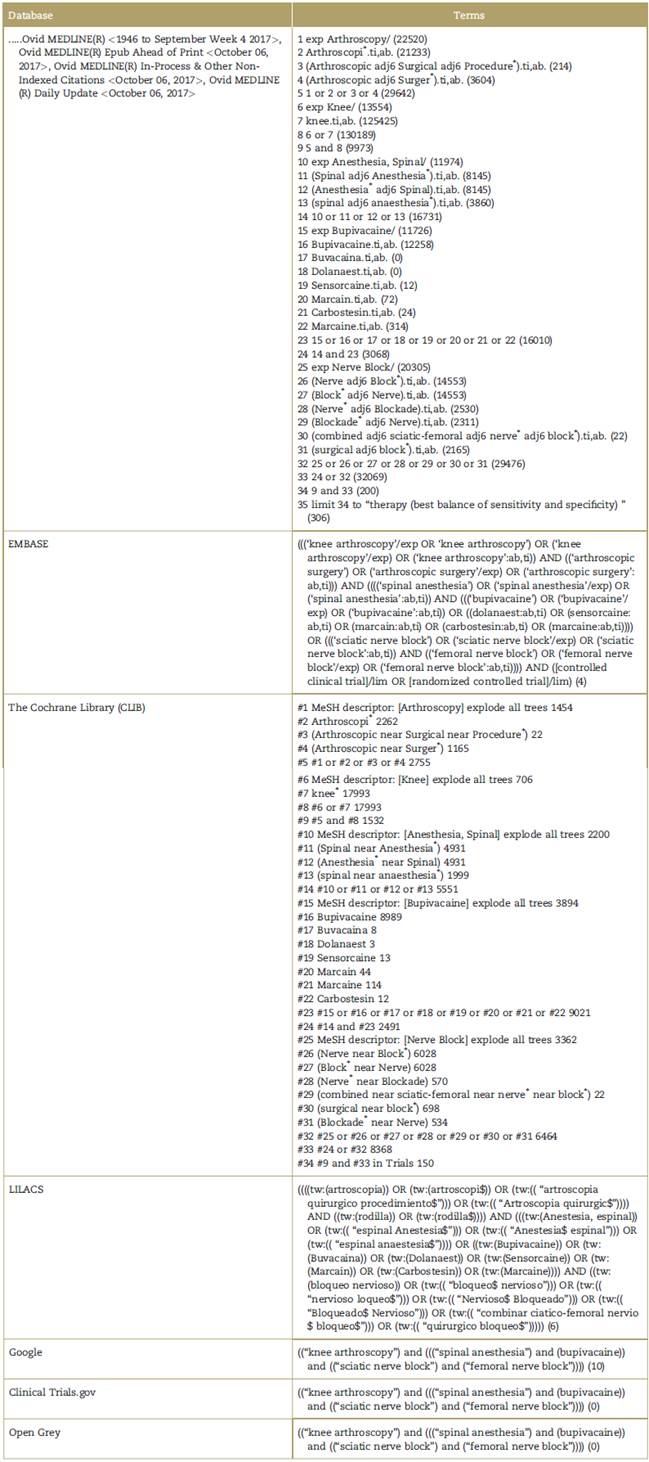
The keywords selected to design a search strategy using synonyms, indexed terms, truncation and proximity operators, were: "spinal anesthesia", "bupivacaine", "nerve block", and "knee arthroscopy". The search was conducted in the following databases: Ovid, Cochrane, Embase, Lilacs, Open Grey, ClinicalTrials.gov, and academic Google, in English, Spanish, and Portuguese, with no date restrictions. The snowball technique was also used. See Annex 1.
Data selection and data mining
Two authors (FACO, AAMO) independently selected the trials following the Cochrane methodology for SRs. The first step is the review and selection of titles and abstracts; the second step is the selection of potential articles for reading of the full text, and a final step of review and selection of the articles based on compliance with all the inclusion criteria. The authors settled their discrepancies consulting a third and a fourth reviewer (IP and GR).
One of the inclusion criteria considered for this SR was the selection of RCTs since the expectation was to avoid trials with design limitations that could bias the estimates of the impact of the intervention. Similarly, RCTs provide better-quality evidence in studies comparing techniques, due to less bias in the design and in the procedures.
Data mining was independently conducted by the authors (FACO, AAMO), using an extraction matrix that included variables such as: name of the first author, year of the intervention, type of surgery, number of patients, age of patients, sample size by group and sub-group, LA agent used, time of total analgesia, length of time of the procedure, adverse events, time of the first spontaneous micturition (minutes), need for rescue analgesia, length of the recovery for discharge (minutes) and patient satisfaction, as information related to effectiveness, safety, and satisfaction.
Evaluation of risk of bias in the trials included
The evaluation of the methodological quality of the trials was done with the Risk of Bias Assessment Tool proposed by the Cochrane collaboration for randomized trials, adapted from Higgins et al.23
This tool was used to assess the following biases: selection, performance, detection, abandonment, report, etc., with a view to making a comprehensive qualified judgment such as: low, unclear, or high. Both authors (FACO, AAMO) independently evaluated each domain and a shared a joint was reached on the risk of bias for each trial.
Treatment effect and analysis measures
Based on the selected outcomes, 5 statistical parameters were chosen for evaluation: total anesthesia time, rescue analgesia, HR, time to first micturition (TFM), and acceptance of the anesthetic technique.
Statistical analyses such as meta-analyses are not applicable for the selected trials, which is considered a limitation for this review. For the evaluation of biases, the Review Manager (RevMan) [Programa informático]. Versión 5.3. Copenhague: The Nordic Cochrane Center, The Cochrane Collaboration, 2014 was used.24
Heterogeneity may not be assessed through statistical tests due to the inability to group the numerical data for outcomes, since these are estimated differently in each trial. If the golden rule criterion is used for I2 value, this may be low because it is <40%.25 For this reason, a narrative study was conducted to consider the clinical and methodological heterogeneity among the trials.
Likewise, the publication bias could not be statistically identified because the review included only 3 articles25 with a small sample size.
Results
Trial identification
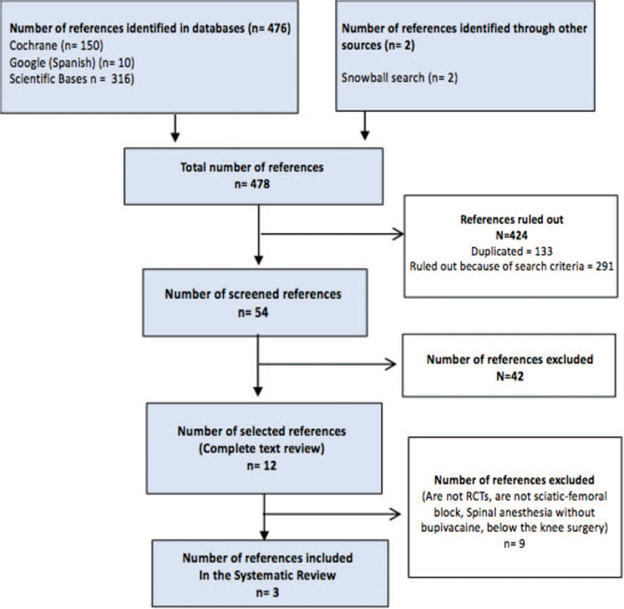
A total of 478 references were analyzed, of which 12 were reviewed as full text, and 3 that complied with the eligibility criteria were selected; the 9 trials not included were ruled out because the SA was administered with a LA agent other than bupivacaine and the lower limb blockade was not consistent with knee arthroscopy (Fig. 1). Of the trials selected, 2 were conducted in Italy16,26 and 1 in Colombia.27
Characteristics ofthe trials
The population in the 3 RCTs corresponds to 100% of patients undergoing elective knee arthroscopy, which makes the populations comparable. However, the use of the various tools for monitoring of the times in each of the trials limits the comparison of the results.
The total population was 132 patients, with a distribution of 50% for each anesthetic technique. Table 1 depicts the characteristics of the trials included.
Table 1 Characteristics of the trials included.
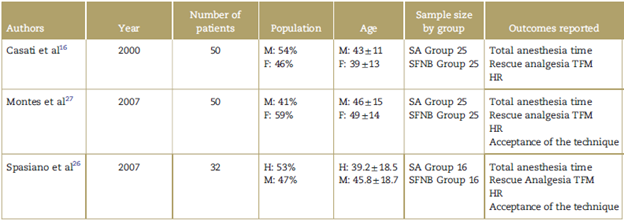
F=female, HR=heart rate, M=male, SA=spinal anesthesia, SFNB = sciatic-femoral nerve block, TFM=time to first micturition.
Source: Authors.
In the SA groups, the studies used the single injection technique for the administration of LA at low doses of bupivacaine.28 According to the literature, low doses range between 5 and 8 mg.29 For the SFNB groups, the studies report a technique using electro-stimulation to identify the peripheral nerves, with variations in the procedure for administering the LA agent. Table 2 illustrates the characteristics of both techniques.
Table 2 Characteristics of the anesthetic technique.

SA=spinal anesthesia, SFNB=sciatic-femoral nerve block.
Source: Authors.
The results reported correspond to the sample of 131 patients because of a technical anesthetic failure in the SFNB in the Montes et al27 trial; the patient required general anesthesia and therefore was excluded from the analysis.
Effectiveness of anesthesia
The effectiveness was evaluated in terms of quality of anesthesia during the postoperative period of the 3 trials from the time of the anesthetic injection until patient discharge. This assessment included both the sensory and motor blockade, using various techniques and scales.
The 3 trials evaluated the sensitivity block before the start of surgery using the prick test, with total loss of sensation for both anesthetic techniques. The trial by Spasiano et al26 used a numerical frequency scale (NFS) during the application of the tourniquet, to complement the sensitivity blockade evaluation.
The motor blockade was evaluated using the Bromage scale with a score of 3 as the optimum value for Casati et al16 and Montes et al,27 while Spasiano et al26 used an orthopedic evaluation of freedom of knee movement during SA, with 94%rated as excellent, 6% as sufficient. With regards to SFNB, 81% rated excellent and 19% rated as sufficient.
Quality of anesthesia. The 3 trials evaluate the quality of anesthesia for the 2 techniques with different tools. The sufficiency of anesthesia over the postoperative period is rated as inadequate in the presence of pain and need for rescue analgesia, and adequate when no additional analgesia was required.
In the trial by Casati et al,16 sufficiency of anesthesia was evaluated every 30 minutes using the modified Bromage scale during the postsurgical period until discharge, with 84% of the patients in the SA group being adequate and 92% in the SFNB group. Furthermore, Montes et al27, evaluated the sufficiency of anesthesia during the postsurgical period in the OR until hospital discharge at 15-minute intervals; the presence of pain was evaluated using the visual analog scale (VAS), with 88% of the patients reporting adequate results in the SA group and 92% in the SFNB group. Spasiano et al26 evaluated the sufficiency of anesthesia during the postsurgical period using the NFS with 94% of the patients rated as adequate in both groups; in addition, 13 patients (41%) still maintained the effect after 2hours, 3 patients (9%) after 4hours, and the effect resolved in all patients after 6 hours.
Use of rescue analgesia. Postoperative pain was monitored using various instruments and at different points in time in each trial. Casati et al,16 continued monitoring through a telephone survey 24hours later and 1 week after the intervention during the postoperative control visit for both groups, reporting that 12% (3 patients) required rescue analgesia in the SA group and 8% (2 patients) in the SFNB group.
The trial by Montes et al27 used the VAS for inpatient monitoring every 15 minutes and then continued daily home monitoring at 6,12,18 and 24 hours for both types of anesthesia, reporting that 16% (4 patients) in the SA group required additional analgesia, while none of the patients in the SFNB group required additional analgesia.
Spasiano et al26 used the NFS in both anesthetic techniques 2, 4, and 6 hours during the postoperative period, reporting that 1 patient (6.2%) required rescue analgesia after 4hours in the SA group and 1 patient (6.2%) after 5.1 hours in the SFNB group.
Safety ofanesthesia and adverse events (AE)
Time to first micturition. The time to the first spontaneous micturition was observed in each group, although Montes et al27 indicates that he does not consider this variable in the results.
According to Casati et al,16 the TFM report is 231±93 minutes for SA and 145 ± 36 for SFNB. On the other hand, the trial by Spasiano et al26 reports a TFM of 269 ± 66 for SA for SFNB. The TFM results in these 2 trials show a difference in favor of SFNB.
In addition, Casatti et al report 12% (3 patients) in the SA group who experienced urinary retention and required a urinary catheter. There were no reports of urinary retention and urinary catheter in the SFNB group.
Changes in heart rate (HR) and other hemodynamic parameters. The 3 trials conducted a routine HR control with non-invasive techniques and other hemodynamic parameters. The study by Casati et al16 emphasized vital signs monitoring and patient awareness during the postoperative period and reported 3 patients (12%) with bradycardia in the SA group and no reports in the SFNB group. The study by Montes et al27, reported ECG conventional monitoring, HR and blood pressure during the procedure, with measurements every 15 minutes during the postsurgical time, with no patient alterations reported.
The study by Spasiano et al26 monitored 4 parameters: systolic blood pressure, diastolic blood pressure, mean arterial pressure, and HR, which were measured at 5 time points (t: 0 minute, t: 5 minutes, t: 10 minutes; t: 15 minutes, t: 30min). Changes in blood pressure were minimal and the HR was lower in the SA group, as compared against the SFNB group.
Patient satisfaction
Acceptance of the anesthetic technique. Two of the 3 trials included this outcome for the 2 anesthetic techniques. The study by Casati et al16 did not.
The studies by Montes et al27 and Spasiano et al,26 evaluated satisfaction using a dichotomous survey, asking whether the patients would undergo a new procedure with the same anesthetic technique. In both trials, 100% of the patients responded positively. The study by Spasiano et al26 also used an ordinal scale in 3 categories to have patients assess the anesthetic technique with the following results: 93% excellent for SA and 87% for SFNB; 6% good for SA and 6% for SFNB; and 0% sufficient for SA and 6% for SFNB.
The consolidated results are illustrated in Table 3.
Table 3 Consolidated results during the postoperative period.
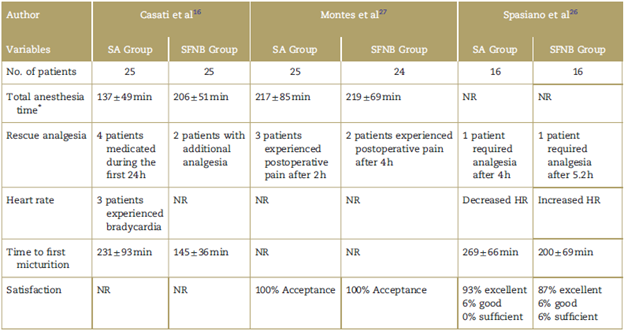
HR=heart rate, NR=Not reported, SA=spinal anesthesia, SFNB = sciatic-femoral nerve block.
*The total anesthesia time reported in the studies corresponds to the sum from the time of anesthesia preparation, surgical preparation, duration of surgery, time in the recovery room, until effective discharge, in minutes.
Source: Authors.
Risk ofbias assessment ofincluded studies
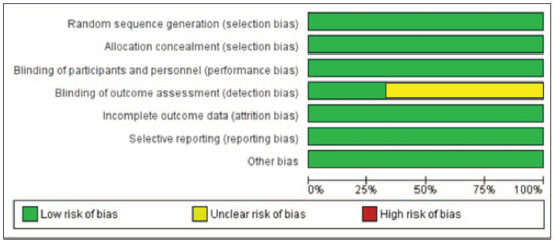
Figure 2 shows the quality evaluation of the studies identified over the search process.
The conclusion is that the trials included in the SR have a low risk of bias for the domains of random sequence, performance, detection, attrition, reporting, and other biases due to explicit non-compliance with the processes and procedures. A clarification must be made regarding the study by Montes et al,27 where 1 patient had to be operated under general anesthesia because of block failure in the SFNB group and was excluded from the analysis by the author.27
Two of the studies show an indeterminate risk of bias for the detection domain. The study by Montes et al27 identified a research assistant doing post-operative monitoring of all patients, but does not specify blinding; and Spasiano et al26 describes the follow-up and recording process without indicating the observer's conditions. Moreover, the study by Casati et al16 assesses the bias of reporting the use of a blind observer for monitoring during the postoperative period until discharge as low risk.
Discussion
The SA technique has been the most widely used technique in knee arthroscopy and the literature reports that it provides a complete sensory and motor blockade of the lower extremity when using low single doses.30 The 3 studies for the SA groups achieved sensory and motor block in all patients with no reports of intraoperative rescue analgesia using a single dose of 0.5% bupivacaine (7, 7.5, and 8mg).
Bupivacaine as a LA agent has been widely studied31 and used in regional anesthesia techniques, with a half-life of 3.5 hours of complete sensory and motor blockade.26 The block times achieved in the 3 studies for the SA group are consistent with the literature,32 but do not allow for an association between the dose and the block, because the results reflect contradictory anesthesia times.
The study by Casati et al16 used the highest dose of hyperbaric bupivacaine (8 mg) which is associated with a higher risk of transient neurological symptoms, more adverse event reports such as cardiovascular dysfunction and urinary retention with urinary catheter, and these results are consistent with the reports of previous research studies,33 but the findings are not significant because of the sample size used. According to Montes et al27 and to other researchers, the preoperative times with SA are shorter and no differences are reported in the total OR time and hospital discharge. However, 12% of the patients required rescue analgesia after 2 hours. The study by Spasiano et al26 used lower doses of bupivacaine (7 mg) with lower requirement of rescue analgesia and no significant adverse effects.
The effectiveness of the SFNB as described in the literature34 is mostly based on the successful unilateral motor and sensory blockade and on the postoperative anesthesia time with a lower risk of hemodynamic changes, preserving the intestinal and bladder function.30,35 The SFNB technique uses multiple procedures that are described in the various approaches,36 demanding knowledge and experience in the technique for a successful outcome.37,38 Greater patient safety and stability is also reported during the perioperative period, reducing the adverse effects and the need for postoperative analgesia.39
In the study by Casati et al16 the postoperative analgesia times were longer and the TFM was shorter, as compared with SA; 2 patients required rescue analgesia associated with hip pain subsequent to limb manipulation during the procedure. The study by Montes et al27 compared the level of analgesia effect during the postoperative period (6 hours) and found a superior effect in the SFNB group, with no significant differences in other outcomes. In this study, there was a technical failure on the SFNB that required the use of general anesthesia, which evidences the need to strengthen the anesthetic technique-patient relationship. Spasiano et al26 showed that it is possible to achieve a successful SFNB with low LA concentrations using shorter administration times, that are associated with minimal hemodynamic changes and significant cardiovascular stability. The changes described in HR correspond to mild increases in the SFNB group and decrease in the SA group. The SFNB group experienced longer postoperative analgesia and shorter spontaneous micturition times, as compared to the SA group. One patient from each group required rescue analgesia, but the administration for the SFNB patient was 80 minutes later as compared to the patient in the SA group.
When comparing the outcome of rescue analgesia between the 2 groups, there is a significant difference in favor of SFNB with 3% of the patients requiring rescue therapy, versus 12% in the SA group.
In the 3 trials, the postoperative analgesia times favor the SFNB group, with 1 additional benefit associated with the preservation of organic functions that contribute to patient discharge, as expected for ambulatory surgery.
The 3 studies show evidence of higher patient safety with SFNB, associated with less cardiovascular and neurological function risk, and less urinary retention. Other adverse effects described may be due to LA-related complications and the route of administration of the agent.40
Patient satisfaction was evaluated using different tools in each trial, with no differences found in favor of 1 or other technique.
The 3 trials are relatively homogeneous with regards to the SA technique, but the results differ in the safety evaluation and this may be explained based on the dose of LA used by Casati et al16,8mg versus 7.5and 7mgin Montes et al27 and Spasiano et al,26 respectively. There are differences in the injection technique and the drug used for SFNB, but the results reported are very similar with regard to the quality of the block and the safety of the patient, though there were some differences in the way the outcomes were assessed; for instance, when evaluating the quality of the postoperative analgesia, the trials used VAS, modified Bromage scale, and NFS.
This SR failed to statistically assess the potential existence of publication bias; however, it is presumed to be low on account of the comprehensive search of the studies and the reference to additional sources.
With the results obtained for the continuous numerical variable of TFM, it is possible to argue in favor of the SFNB technique since it does not interfere with voiding. Unfortunately, the trials do not report separately the anesthesia times, limiting the analysis of this SR which focuses on postoperative time.
Finally, the potential occurrence of bias risk in the trials is overall low, which does not compromise the validity of the trials.
Conclusion
There are not enough studies to definitely compare the 2 anesthetic techniques based on the outcomes proposed for this SR. In terms of the effectiveness of anesthesia, both the SFNB and SA deliver highly satisfactory postoperative analgesia times; and in terms of safety, there is a lower risk of adverse events and earlier recovery with SFNB. However, the studies do not allow for conclusive statements.
SA is more widely accepted among the professional anesthesiologists because of ease and quick administration, while SFNB requires technological support, training, and skills for a successful result. Considering that knee arthroscopy is an ambulatory procedure, further research is needed to determine which technique should be used for each particular case.
Ethical responsibility
This is a secondary study and hence it is not governed by the ethical standards for research on human beings. Nevertheless, from the ethical point of view, this systematic review pulls together current concepts about residual and postoperative analgesia control in knee arthroscopy, keeping in mind the benefit for the patients undergoing this procedure in our daily practice.
The privacy of the patients included in the randomized clinical trials used for this review, the authors, their rights and outcomes shared shall be respected.











 text in
text in