Isolated left ventricular noncompaction cardiomyopathy (ILVNC) is a rare genetically heterogeneous condition characterized by hypertrabeculation and sponge-like appearance of the left ventricular myocardium (Fig. 1). ILVNC can be congenital in nature or acquired later in adult life. In addition, sporadic occurrence and familial transmission have been described.1-3
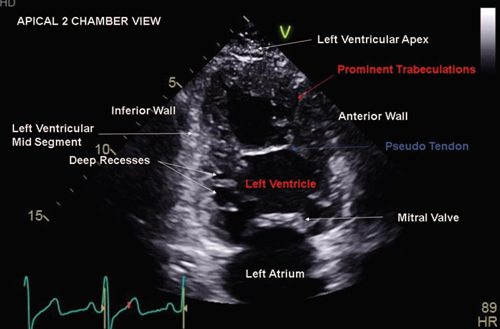
Source: Authors.
Figure 1 Apical 2 chamber view displaying hypertrabeculation in left ventricular non compaction cardiomyopathy.
In the early intrauterine period, the myocardium exists as a loose meshwork. By the 18th week of life, coronary vasculature is established and the loose myocardial meshwork compacts. This process is responsible for the relatively smooth appearance of the normal left ventricular wall (Fig. 2). The embryogenic hypothesis suggests that arrest of this process causes ILVNC (see Video, Supplemental Digital Content, http://links.lww.com/RCA/A852). The non embryogenic hypothesis proposes that chronic changes in left ventricular loading conditions leads to hypertrabeculation.1,2
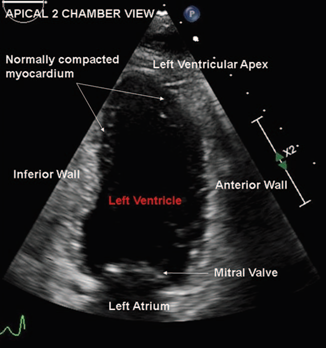
Source: Authors.
Figure 2 Apical 2 chamber view displaying scarcely trabeculated normal left ventricular myocardial walls.
Although children and adults present similarly with heart failure, arrhythmias, thromboembolic phenomenon, or sudden cardiac death, patients with the acquired form of ILVNC may be largely asymptomatic as children. Currently, the true prevalence of ILVNC is unknown. Males are affected more than females.1,2
Definitive diagnosis of this condition relies on cardiac resonance imaging. Echocardiographic diagnosis requires that the ratio of left ventricular non compacted to compacted myocardium at end-systole in the parasternal short axis view exceeds 2 (Fig. 3).3,4
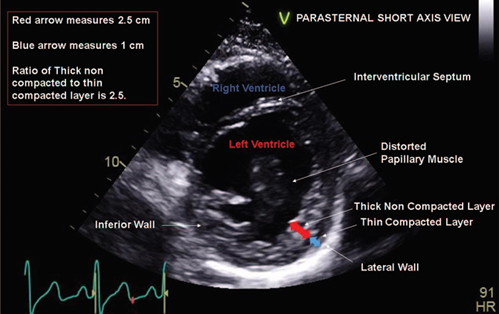
Source: Authors.
Figure 3 Measuring and calculating ratio of thick non compacted to thin compacted myocardium in the parasternal short axis view.
Women with ILVNC are at a high risk of developing decompensated heart failure during pregnancy. Cardiovascular changes in pregnancy including tachycardia, intravascular volume expansion, and anemia exacerbate heart failure. Vaginal delivery with early institution of epidural analgesia is preferred in stable patients. Refractory heart failure with hemodynamic instability necessitates cesarean delivery under general anesthesia. Cesarean delivery is preferably conducted in cardiac surgical operating rooms lest extracorporeal life support is needed for refractory hypotension. Pre induction arterial line and central venous cannulation is prudent. Inotropic and vasopressor support may be necessary at or soon after induction.5,6
Ethical responsibilities
Protection of people and animals. No experiments on people or animals were done.
Confidentiality of the data. All protocols at our institute were followed and patient or hospital identifiers have been removed from all images.
Right to privacy and informed consent. As patient and hospital identifiers have been removed, no informed consent was solicited for this production.











 text in
text in 


