Introduction
The laryngeal mask airway (LMA) is one of the most used devices for airway management. It is easy to insert, safe, and efficient.1 It was created by Archie Brain in 1983 as an alternative to a facial mask and orotracheal tube, especially in cases where it is difficult to maintain the airway or when a less invasive and less traumatic option is needed.1,2 In order to improve this device's safety, ProSealTM LMA (The Laryngeal Mask Company Ltd., Le Rocher, Victoria, Mahé, Seychelles. United Kingdom) was developed in the year 2000. As an additional feature, it has a drainage channel for suctioning esophagogastric secretions, decreasing distension, regurgitation, and risk of aspiration.3 Besides that, it offers a better seal at the laryngopharyngeal level, since the cuff is more distensible, compared to a Classic LMA, it expands better over these structures and facilitates oropharyngeal leakage pressures when it reaches 25 to 30 cmH2O during controlled mechanical ventilation, being this value greater than in other supraglottic devices.2-5 In this way it increases the possibility of success in patients with compliance disorders or pulmonary obstruction.6,7
There are different types of LMA devices each with different designs and manufactured material, each created for specific conditions and uses in the patient. Widely available are Classic LMA, i-gel (Intersurgical Ltd., Crane House, Wokingham, Berkshire, United Kingdom), Fastrach, ProSealTM, Supreme, and Unique, among other trademarks. As ProSealTM is the basis for further developed types of LMA, it is recognized by some as the "gold standard" and considered to be the point of comparison for emerging supraglottic devices.5,7,8 Despite multiple clinical trials and meta-analyzes available comparing the effectiveness of different designs, results are diverse and difficult to reproduce, leading to insufficient evidence to a clear decision on what type to prefer over the others.5-7,9-12
Complications in airway management are the most feared events in anesthesia due to their high morbidity and mortality opportunities for the patient.13-20 Many reviews have been aimed at creating difficult airway algorithms, to foresee these situations and establish the most appropriate management of a patient's airway.16,19-22 Existing guidelines recommend using the LMA as rescue in failed laryngoscopy or if an unexpectedly difficult airway is found.16,19,23,24 However, difficult ventilation and failure have also been described with these devices, situations that alter patient's oxygenation and threaten life.5,20,25,26
Ventilatory failure has been evaluated for Classic and Unique LMA reporting incidence from 0.2% to 4.7%.9,17,18,25,26 The rate variation depends on the definition for LMA failure considered by the studies, population characteristics and type of device used. In general terms being male, over 45 years of age, obese, with poor dentition, thyromental distance less than 6cm and limited neck movements are associated factors for LMA ventilatory failure. Other studied factors exist such as: Mallampati score, history of pulmonary pathology, and practitioner experience without showing significant relationship so far.17,18,20,25
In searches of international and national literature there is no evidence found of similar studies specific for ProSealTM LMA, one of the most used devices in reference centers of the country, such as Fundación Valle del Lili. The aim of this research was to determine the incidence of failure with this ProSealTM LMA and to identify related clinical conditions.
Methods
An observational analytic study of a group of adult patients undergoing anesthetic procedures for urgent or elective surgery using ProSealTM LMA for airway management in which the presence or absence of failure was evaluated.
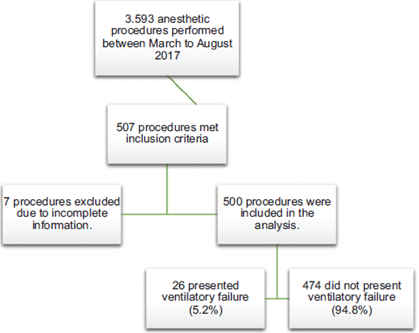
A total of 3.593 anesthetic procedures were performed at Fundación Valle del Lili from March to August 2017. Patients with incomplete information about the type of device used for airway management, pregnant women, full stomach or usage of a LMA different from ProSealTM were excluded.
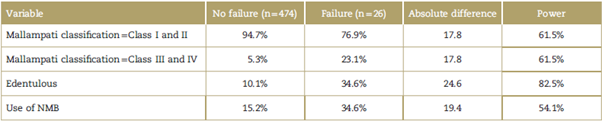
A total of 500 procedures from 489 different patients met the inclusion criteria, discriminated as follows: 27 with ventilatory failure and 474 without the event (Fig. 1). A difference in the exposure proportion between groups (no failure and failure) with a 95% confidence interval (CI) was used to calculate the power of the study with this sample size. Table 1 show the power of the study calculated for each variable for differences in the exposure proportion between groups over 17.8%. A difference in the exposure proportion less than 17.8% had a power between 7% and 33.4%.
Source: Authors.
Figure 1 Research flowchart of patients having anesthetic and surgical procedures between March and August 2017.
Demographics, clinical history, difficult airway predictors, intraoperative management and LMA failure were included. At the beginning of the day Case Report Forms (CRFs) were distributed in every operating room. In case of using ProSeal™ LMA, they were filled by the attending anesthesiologist, resident of anesthesiology or medical student, not associated investigators of this research. At the end of the day CRFs were collected by authors who then entered the information into electronic database available at the institutional digital platform. The attending anesthesiologist decided the airway management solution for every patient as they did during their daily clinical practice. When ProSealTM LMA was used the size was chosen, usually, depending on patient's weight according to manufacturer's recommendations (LM instruments S.A., Bogotá, Colombia). Cuff insufflate volume was chosen by the anesthesiologist without exceeding manufacturer's recommended volumes or up to 60cmH2O measured with manometer.27
To define LMA failure, definitions by different authors were considered and are shown in Table 2. Therefore, it was decided to include the main characteristics of found descriptions: need to exchange to another device, time and dysfunctionality. LMA failure for this research was then defined as the presence of gas leakage that does not allow reaching the programmed volume or ventilatory pressure from the start of ventilation until 5 minutes after its implantation, requiring change in LMA size or insertion of an orotracheal tube.
Table 2 LMA failure definitions available in the literature.
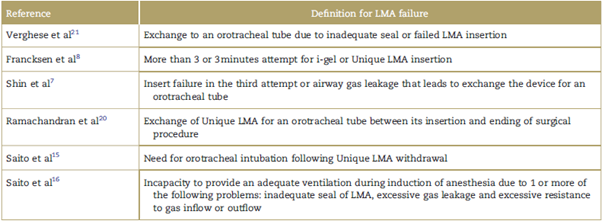
LMA=laryngeal mask airway.
Source: Authors.
This research follows international laws for biomedical investigation for the World Health Organization entrusted in Helsinki Declaration, and it is regulated by Resolution No. 8430 of 1993 by Colombian Health Ministry. According to established risk categories, research was considered without risk given its documental character where authors did not assign biologic, psychologic or social exposures to patients different from the ones required for their surgical procedures. This research has Institutional Review Board approval in Fundación Valle del Lili with internal certificate no. 06 of March 22, 2017, therefore, the ethics committee decided to exempt informed consent.
Statistical analysis
Statistical analysis was performed using statistical software STATA 12.1 (StataCorp. 2011, Stata Statistical Software: Release 12; StataCorp LP, College Station, TX). Incidence of ventilatory failure with ProSealTM LMA was calculated taking the number of failures over the total of anesthetic procedures included in the research period.
Continuous variables were expressed as mean and standard deviation or median and interquartile range (IQR), according to assumption of normal distribution. Categorical variables were presented as proportions and the comparison between them was made with Fisher's exact test or Chi2 depending on procedure's distribution for each category, considering a statistical significance as a P value <0.05. Results were shown in frequency tables.
For multivariate analysis skewed logistic regression was used to estimate adjusted odd ratios (ORs). This method is useful when there are extreme probabilities, that is, when for the outcome variable a greater proportion is presented in one of the categories. Under this scenario, the use of a classic logistic regression is not adequate, since it assumes that the probability of failure is 50%,28 which does not occur in this research because the probability was 5.2%.
This regression includes variables with a P value <0.15 in the bivariate analysis. The variables were selected using the backward method and for each model the Akaike information criterion (AIC) and the Bayesian information criterion (BIC) were calculated in order to evaluate the goodness-of-fit. The model with the lowest AIC or BIC value was chosen in the selection of variables.
Results
A total of 500 procedures were included (Fig. 1). Median age was 51 years (IQR 37.0-65.0 years) and 26 for body mass index (IQR 23.6-28.4). The majority were women (62.2%) and LMA size most frequently used was 4 (68.2%) (Table 3).
Table 3 Population clinical characteristics.
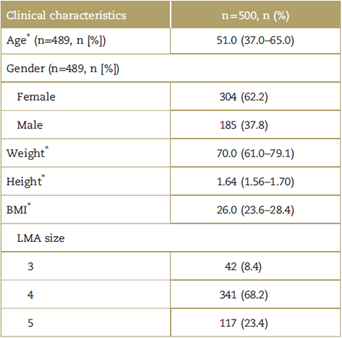
BMI=body mass index, LMA=laryngeal mask airway.
* Median (IQR).
Source: Authors.
Incidence of ventilatory failure with ProSealTM LMA was 5.2% (26 out of 500 procedures). Age (P = <0.001), Mallampati Classification (P = 0.002), reduced neck movements (P 0.025:, edentulous (P = 0.001), use of neuromuscular blockers (NMB) (P = 0.024) and inadequate anesthetic depth, and/ or laryngospasm (P = 0.001) were statistically significant related factors among the group that presented ventilatory failure (Table 4). Failure was more frequent in patients older than 75 years, while those who did not present failure occurred in greater proportion under 60 years. Patients without failure had Mallampati Classification I more frequently, and those with failure had Classification III and IV. It is more frequent that patients with ventilatory failure be edentulous, with reduced neck movements, intraoperative use of NMB and present inadequate anesthetic depth, and/or laryngospasm.
Table 4 Related clinical conditions with ProSealTM LMA ventilatory failure.
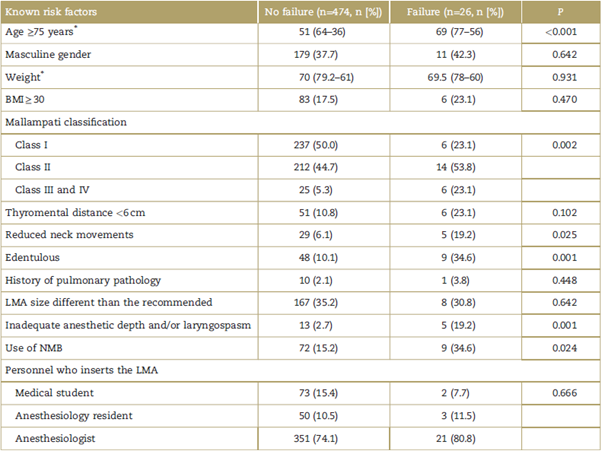
BMI=body mass index, IQR=interquartile range, LMA=laryngeal mask airway, NMB=neuromuscular blockers.
*Median (IQR).
Source: Authors.
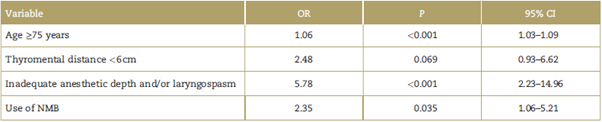
Later with the Skewed logistic regression more parsimonious model it was found that the age (OR = 1.06,95% CI 1.03-1.09, P <0.001), thyromental distance less than 6 cm (OR=2.48, 95% CI 0.93-6.62, P = 0.069), inadequate anesthetic depth and/or (OR = 5.78, 95% CI 2.23-14.96, P < 0.001) and intraoperative use of NMB (OR=2.35, 95% CI 1.06-5.21, P =0.035) were associated factors for LMA ventilation failure. Results of this model are presented in Table 5.
Discussion
Ventilatory failure with ProSeal™ LMA in patients seen in Fundación Valle del Lili was 5.2%, being higher than reported for Classic and Unique LMA.9,17,18,25,26 Ramachandran et al25 described a 1.1% incidence of failure with Unique LMA in more than 15,000 anesthetic procedures and Saito et al17,18 reported 0.2% with different types of LMA. However, the incidence estimated with this research remains being low compared with the estimated for the overall of patients in which any type of LMA is being used.
We identified that patients older than 75 years, edentulous, with Mallampati Classification III or more, reduced neck movements, short thyromental distance, use of NMB and inadequate anesthetic depth, and/or laryngospasm had a greater opportunity to develop ventilatory failure with ProSealTM LMA. It is proposed to evaluate the presence of these clinical characteristics, in order for the professional be prepared with other airway devices and improves patient's conditions to achieve a successful airway management.
This research identified that the older the population was, the proportion of patients with ventilatory failure increases. Result consistent with authors like Ramachandran et al25 and Saito et al17 who identified the age as risk factor for failure, specifically being older than 45 years.18 This relation can be explained by the structural changes in this population's upper airways, which is more elliptical and less firm compared to younger people.29
To secure the airway correctly, the anatomy of patients should allow an alignment of the oropharynx and fixation of the LMA to the hypopharynx. That may be limited if the patient has a short thyromental distance and poor neck mobility, both reported as risk factors for LMA failure in the literature.17,18,20,25 In this research at first bivariate analysis they were proven significant, and even though the thyromental distance less than 6cm entered the logistic regression model, they both failed to demonstrate statistical significance at the end. In a clinical setting they are usually considered important together to achieve an adequate positioning of the patient and it is very difficult to distinguish which could be more determinant for an easier insertion of the device.17,18
Although an adequate anesthetic depth is considered essential for a successful LMA insertion,1 in the literature reviewed an insufficient anesthetic depth and/or presence of laryngospasm have not been considered an isolated factor associated with failure of supraglottic devices.17,18,25 We identified that having an inadequate anesthetic depth and/or presence of laryngospasm represents a 5 times greater opportunity to develop ventilatory failure. This finding could be due to the possibility that the patient bites the device, moving it and not permitting an adequate seal. In addition, it could generate laryngospasm, which avoids airflow to the lungs, altering oxygenation, and finally leading to device failure.
It is well known the need of NMB for insertion and functioning of the orotracheal tube, but their role for LMA use remains controversial. Recent clinical trials have shown no differences in terms of seal pressures, surgical conditions, and pharyngolaryngeal discomfort with ProSealTM LMA when NMB are used or not, but with longer recovery times when they are used.30,31 We identified a statistical significant relation between ventilatory failure and intraoperative use of NMB, where the opportunity of developing failure is 2 times greater when they are used. This intriguing finding favors the latest tendency in the literature that NMB are not necessary for LMA positioning,17,30,31 even though in the clinical setting we can evidence improving anesthetic conditions for LMA insertion with their use. This can be explained by changes in upper airway structure when patients are anesthetized and paralyzed compared with conscious patients, evidenced through radiological examinations by Sivarajan and Joy.32 These structures move backwards with head extension leading to oropharynx narrowing and possibly making the LMA insertion harder.
We identified no statistically significant relation between being edentulous and LMA ventilatory failure, even though a higher proportion of failure was seen with this condition. This is congruent with some reported research in which having lesser dental pieces was associated with this device failure,20,25,33 and may be due to increased laxity in pharynx tissues, which prevents an adequate fixation of the device, facilitating its displacement and allowing air leakage as an insufficient seal is obtained, generating greater difficulty for airway management.23,25,33-35
For explaining the differences between genders, many research has described the increased resistance of a male's upper airway compared to a female's, leading to a narrow lumen and airway obstruction.20,25,34 This condition could predispose male patients to failure with a supraglottic device explaining the significant relation observed in recent investigations,17,25 however for this research failed to prove significance.
History of pulmonary pathology was considered if the patient had chronic obstructive pulmonary disease, asthma, or obstructive sleep apnea syndrome. Decrease in lung compliance and increase airflow resistance through the lungs are pathophysiological changes described in these conditions that can generate high airway pressures with subsequent possibility for oropharyngeal leakage and leading to failure.20,25,34 Nevertheless, it was not possible to demonstrate a statistically significant relation.
Despite the fact that the experience of the person managing the airway has been considered as a risk factor for the failure of orotraquel intubation,20 this variable was included in the analysis, without statistical relation among the staff that inserted the device, including students of medicine, residents and anesthesiologists. Result compatible with the exposed by Ramachandra et al.25
Results of this research contribute to medical literature with the identification of related clinical conditions to ventilatory failure with ProSealTM LMA in patients seen in a high-complexity hospital in Cali, Colombia, where in addition to other known factors, we obtained a statistical significant relation between an inadequate anesthetic depth and/or presence of laryngospasm with this device ventilatory failure, being described for the first time in these investigations. It is proposed that in case of identifying any associated factor for failure, the anesthesiologist should be prepared with other devices such as orotracheal tubes, video-laryngoscope or fiberscope, in order to effectively manage failure and avoid its complications like hypoxemia, brain injury and even death.
The main limitation was the amount of patients that presented the event, even though a multivariate analysis with skewed logistic regression was carried out.
Ethical responsibilities
This research follows international laws for biomedical investigation for the World Health Organization (WHO) entrusted in Helsinki Declaration, and it is regulated by Resolution No. 8430 of 1993 by Colombian Health Ministry. According to established risk categories, research was considered without risk given its documental character where authors did not assign biologic, psychologic or social exposures to patients different from the ones required for their surgical procedures, therefore, the ethics committee decided to exempt informed consent. This research has Institutional Review Board approval in Fundación Valle del Lili with internal certificate no. 06 of March 22, 2017.











 text in
text in