Introduction
Nausea and vomiting are a frequent complication during the postoperative period. The incidence of nausea and vomiting without preventive pharmacological management ranges between 20% and 40%, but may rise to 70% among the population with risk factors for this condition.1 The consequences of experiencing postoperative nausea and vomiting (PONV) are multiple and clearly impact both the patient and the healthcare institutions. Some of these consequences are suture dehiscence, esophageal laceration, hydro electrolytic imbalance, patient dissatisfaction, higher healthcare-associated costs, and delayed hospital discharge.2-4
The risk factors associated with the development of PONV have been linked to the patient's clinical condition, the anesthetic procedure, and the type of surgery. The patient's characteristics identified include: female gender, non-smoker, a history of PONV, and a history of motion sickness. In terms of the anesthetic procedure, these include the use halogenated agents, the use of opioids during the intra and post-operative period, the use of nitrous oxide, duration of anesthesia (the risk increases by 60% per every 30 additional minutes) and the state of hydration of the patient, since the lack of fluids promotes PONV.5 Finally, the type of surgery has also been associated with the development of PONV: laparoscopic procedure, laparotomy, strabismus, plastic surgery, maxillofacial, ophthalmological, neurological, urological, and gynecological.1,6,7
Similarly, protective factors for the development of PONV have been identified, including favoring the use of continuous infusion of propofol, minimizing the doses of neostigmine, patient's own preparation before the procedure (acupuncture, music therapy, acupression, transcutaneous electrical nerve stimulation)8,9 and adequate pharmacological intraoperative prophylaxis with significant antiemetic power.10
However, the scientific evidence regarding the factors associated with the development of PONV notwithstanding the use of pharmacological prophylaxis is scarce. Consequently, this research project identified the demographic and clinical factors of patients, as well as the perioperative variables associated with the development of PONV following antiemetic prophylaxis.
Materials and methods
Context
The study was conducted at Fundación Valle del Lili (FVL), in a University Hospital specialized in high complexity patients in the Southwestern region of Colombia. Our institution currently uses the "Fundación Valle del Lili's protocol for the prevention and treatment of postoperative nausea and vomiting", based on a consensus guideline for the postoperative management of nausea and vomiting of the Society of Ambulatory Anesthesia.11 This protocol uses a risk scale adapted pursuant to the recommendations of that consensus, and establishes the medications for adequate antiemetic prophylaxis in each patient. The medications used in the institution are ondansetron, dexamethasone, haloperidol, and continuous propofol infusion and midazolam.
Type of study
A case-control study was conducted based on an institutional record of adult patients admitted to the postanesthesia care unit (PACU) following surgery under general anesthesia, between April and June 2017. The following were the exclusion criteria: anesthetic procedures in obstetric patients (including cesarean sections or postnatal procedures within less than 6 weeks), suspicion of, or proven increased intracranial pressure, patients with pre-operative intestinal transit disease (gastroparesis, esophageal stenosis, gastric, or intestinal obstruction), patients that were receiving dopaminergic, serotoninergic, or histaminergic drugs routinely and received at least 1 dose during the week before the procedure; patients that received chemotherapy during the last 15 days, users of preoperative nasogastric tube, and patients that were admitted to the intensive care unit during the 24hours of the post-anesthesia period.
Cases comprised patients with nausea or vomiting within the first 6 postoperative hours, despite having received antiemetic prophylaxis. Moreover, the patients that received antiemetic drugs and did not develop any of these symptoms during the follow-up period, were considered controls. Every patient received at least 1 antiemetic agent.
During the study period, a total of 1114 patients were admitted to the PACU. The case: control ratio was 1:4. All patients that developed PONV during this period of time were considered as cases and a random sample was selected from the group of patients that met the criteria for controls, in order to analyze a number of controls that met the pre-established 1:4 ratio. The power of the study to identify a 50% of females among the cases and an odds ratio (OR) = 2 for gender was 77.5%.
Data collection and processing
The source of information was the electronic medical record; specifically, the pre-anesthesia, anesthesia, and postoperative recovery room follow-up records were reviewed. The data of interest were entered into the software BD Clinic (Fundación Valle del Lili, Cali, Colombia). The protocol for this study was approved by the Ethics and Biomedical Research Committee of the FVL (protocol 970). According to the standard of the Colombian Ministry of Health, responsible for regulating research in the health sector, this study is a risk-free research project, and therefore a request was submitted to waive the informed consent.
Statistical analysis
Central tendency measurements were used to describe the patients' characteristics (mean or median) and dispersion (standard deviation or interquartile range) for the continuous variables, according to the normal distribution verified with the Shapiro-Wilk test. The qualitative variables were presented as relative and absolute frequency distributions.
The comparison of quantitative variables between cases and controls was done with t Student when the variable followed a normal distribution; otherwise, the MannWhitney U test was used. For the qualitative variables, the X2 statistical test or the exact Fisher's test was used, based on the expected frequency in the categories. The level of significance was set a 5%.
In terms of the identification of potential factors associated with the occurrence of PONV following anti-emetic prophylaxis, a bivariate analysis was conducted estimating the crude OR with its confidence intervals. Then a logistic regression was conducted to identify the variables associated with PONV, following the analysis based on other independent variables; adjusted ORs were obtained. This last analysis included the factors with a P value <0.2 in the bivariate analysis.
Results
A total of 80 patients who experienced PONV and 332 patients who experienced no symptoms following prophylaxis were included, for a total of 412 patients. All patients were comparable in terms of age, personal history, use of fentanyl, remifentanil, and halogenated anesthetic agents. In addition, there were no differences among the various methods to secure the airway. Table 1 lists the general characteristics of the sample, stratified by group.
Table 1 Demographic, clinical, and perioperative patient characteristics.
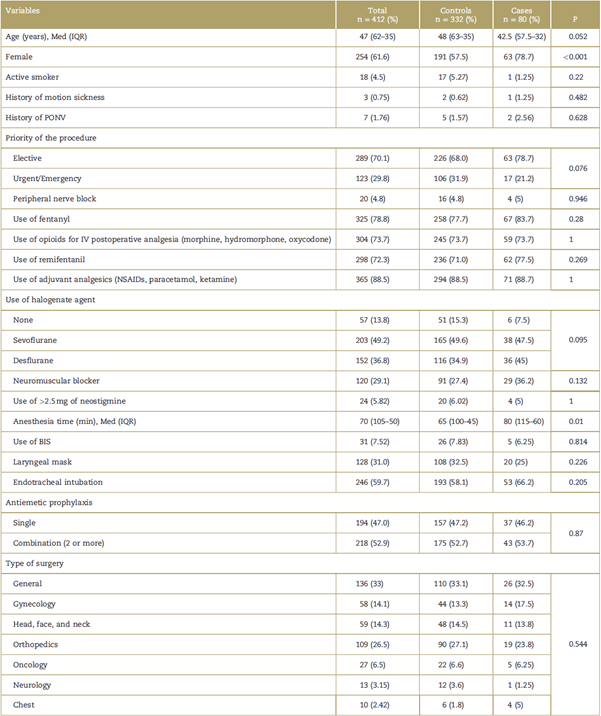
BIS=bispectral index, IQR=interquartile range, IV=intravenous, Med = median, NSAID=non-steroidal anti-inflammatory drug, PONV=postoperative nausea and vomiting.
Source: Authors.
In contrast, statistically significant differences were found with regard to gender and duration of anesthesia between the groups. The percentage of women was higher in the PONV group (63 [78.8%] vs absence of PONV 191 [57.5%]; P<0.001); similarly, the duration of anesthesia was higher among the cases (80 [115-60]) vs the controls (65 [100-45]; P = 0.01).
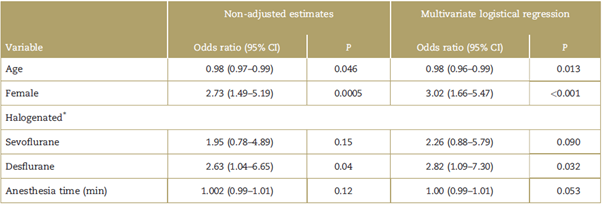
The most parsimonious logistical regression model found that the factors associated with PONV following prophylaxis were age (OR = 0.98, 95% confidence interval [CI] 0.96-0.99; P = 0.013), female gender (OR=3.02, 95% CI 1.66-5.47; P < 0.001) and the use of desflurane during the surgical procedure (OR=2.82, 95% CI 1.09-7.30; P<0.032). The Hosmer-Lemeshow test estimated a P value of 0.88, and indicated that the logistics model is adjusted to the data. This regression model allows for an acceptable discrimination between patients with and without PONV after prophylaxis (Area under the curve - Receiver operating characteristic = 67%, 95% CI: 61.4%-73.7%). The results of the multivariate logistical regression are show on Table 2.
Discussion
Nausea and vomiting are frequent postoperative complications that may trigger unfavorable clinical conditions, in addition to patient dissatisfaction and higher healthcare costs. In this retrospective case-control study, we identified the factors associated with the occurrence of PONV, despite pharmacological antiemetic prophylaxis.
In the study, females had 3-fold odds of developing PONV as compared to males, which is consistent with the risk factors classically described in the literature.12,13 In 2018, Yi et al conducted a study aimed at identifying the relationship between incidence and risk factors for PONV in patients with intravenous patient controlled analgesia (IV-PCA); information on 6773 individuals was collected and as part of the analgesia protocol, all patients received antiemetic prophylaxis with 5-HT3 receptor antagonists. The authors reported for females an OR of 2.9 (95% CI 2.39-3.52, P ≤0.001).14 The explanation for female susceptibility to this complication has yet to be fully understood; however, it is well known that there is a sensitization of the chemoreceptors from the area postrema and the structure that controls vomiting to the follicle stimulating hormone and to estrogens.15
It was also found that the patients that received desflurane as part of their general anesthesia are more likely to experience PONV following prophylaxis as compared with the patients who were not exposed to halogenated anesthetic agents. This result is consistent with previous research studies that found that the use of halogenated agents is a risk factor for the development of these postoperative symptoms.16,17 In 2014, Choi et al published a study that assessed the incidence and the risk factors for PONV in patients with IV-PCA based on fentanyl and antiemetic prophylaxis with 5-HT3 receptor antagonists. The univariate analysis in this study found an increased occurrence of PONV in patients in whom volatile anesthetic agents were used. However, the multivariate analysis just identified a significant association with the use of desflurane versus sevoflurane.18 This may be due to the fact that desflurane clearance is faster than the other halogenated agents, allowing for an early recovery of consciousness; moreover, it is associated with more upper airway irritation which triggers the development of this complication.14,19
In terms of the age variable, the median for cases was 42 years (interquartile range [IQR]: 57.5-31.5), while for controls the median was 51 years (IQR: 64-35), the OR was 0.98 (95% CI 0.96-0.99, P ≤ 0.013). So the conclusion was that the odds of experiencing PONV tend to decrease as age progresses. This information has been studied since 1999 by Sinclair et al, who identified a 13% drop in the probability of PONV per every 10 additional years (OR of 0.87, 95% CI 0.8-0.9, P ≤ 0.0008). This may be explained by a reduction of the autonomic reflexes with age.20 More recently, an incidence of 27.2% was reported in patients under 50 years old, versus 14.4% for those over 50 years old.21 However, the studies conducted by Yi et al14 and Choi et al18, failed to show an association between age and the occurrence of PONV.
Moreover, although no statistically significant association was identified between the duration of anesthesia and the occurrence of PONV, the patients that experienced the event had a longer exposure to anesthesia than the patients who did not experience any PONV. This result is consistent with the literature reviewed. In 2002, Apfel et al22 found an OR of 1.36 (95% CI 1.22-1.51, P ≤ 0.001) per every hour of exposure to anesthesia. Another more recent study in 2012, found that in surgeries lasting 1 hour or more, the probability is 1.83 (95% CI 1.41-1.92, P ≤ 0.001) as compared against shorter duration surgeries.21 Finally, in 2014 Choi et al18 identified that a duration of anesthesia beyond 180 minutes is associated with an increased occurrence of PONV.
Among the strengths of this study, it is worth mentioning that the cases and controls belonged to the same population base. Properly defined inclusion and exclusion criteria were established, which enabled a reduction in the selection bias; currently there is a limited amount of literature assessing the risk factors for PONV following antiemetic prophylaxis. However, the study may have information biases since a differential search of the exposures between cases and controls may have been conducted by the researchers, or patients may not have described the symptoms to the healthcare staff, and there may be an under-registration resulting in an underestimated OR. The low frequency of the event studied may be due to the 2 previously described situations. Moreover, nitrous oxide was not included as a variable in the study because it is not used in our institution. Finally, this research was conducted in 1 single healthcare center that delivers high complexity care and relies on multiple integrated services, characteristics that are absent in most of the healthcare institutions in Colombia.
The information collected from this study contributes to close the knowledge gap about the factors associated with the occurrence of PONV, following prophylaxis. The study led to the identification of those conditions previously described in the literature as risk factors for PONV that continue to impact on the development of these symptoms, despite the administration of antiemetic agents. This information will provide the basis to optimize the prevention strategies aimed at reducing the incidence of this complication in patients cared for at the FVL.
In conclusion, the results of the study suggest that the female gender and the use of desflurane are risk factors for the development of PONV, in patients who received pharmacological antiemetic prophylaxis. Furthermore, elderly individuals have lower odds of experiencing this complication.











 text in
text in