Introduction
In 2016, Forero et al1 presented the first description of the erector spinae plane (ESP) block and since then, it has shown high effectiveness for the management of various painful processes, including chronic pain and surgical procedures involving the thoracic wall, the breasts, and the abdominal wall.1,2
Placing a Nuss bar as a method for the correction of pectus excavatum is a painful process that involves passing a pre-shaped metal bar through the chest of the patient, and then the bar is rotated 180° inside the chest to elevate the sternum.3,4 The in situ stability of the bar is variably associated with bone callus formation, which represents additional difficulty for removal,5-7 in addition to a higher incidence of acute and chronic postoperative pain following removal.8,9
In ESP cadaveric studies, the local anesthetic agent distributes throughout the connective tissue and the ligaments, anteriorly and toward the transverse process into the paravertebral space, anesthetizing not only the ventral and dorsal branches of the spinal roots, but also the communicating branches that carry the autonomic fibers from the sympathetic ganglia.1,2 Notwithstanding its potential use in thoracic surgeries, there is only 1 publication on ESP block as an analgesic method following the surgical placement of the Nuss bar.10
Following is a discussion of one of the first reports (probably the first) on the use of a bilateral thoracic ESP block as the primary postoperative opioid-free analgesic method for the removal of the Nuss bar in an adolescent patient.
Clinical case
This is a 17-year-old male patient, American Society of Anesthesiologists (ASA) Classification 1, 60 kg of body weight and a body mass index of 19. Relevant history: controlled asthma and surgical placement of the Nuss bar 3 years earlier.
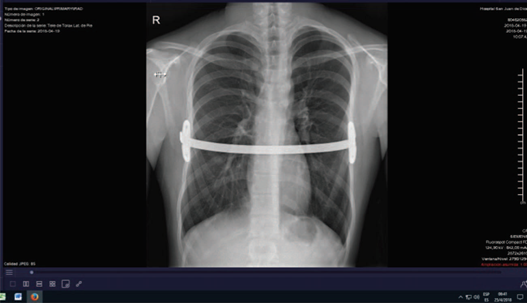
During the pre-anesthesia visit, the physical examination found the patient in good general condition, with no predictors of difficult airway, persistent rib cage deformity, and left scoliosis (Fig. 1). The chest X-ray shows the presence of the Nuss bar placed across (Fig. 2). After explaining the risks and complications of anesthesia, the informed consent was signed.
Basic monitoring was used in the operating room (noninvasive blood pressure monitoring, continuous electrocardiogram, and pulse oximetry). A peripheral 18-G catheter was inserted and the induction of anesthesia was administered with 100 mg of fentanyl, 120 mg of propofol, 35 mg of atracurium, and 8 mg of dexamethasone. The patient was intubated with a first attempt grade 1 laryngoscopy. The maintenance of anesthesia was provided with sevoflurane at a minimum alveolar concentration of 1.0.
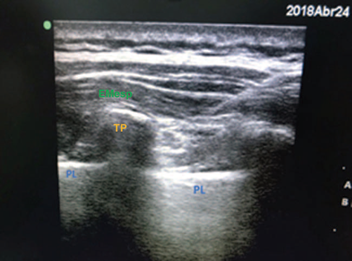
Following the induction of anesthesia, the patient was placed in lateral decubitus for the ESP block. Asepsis of the dorsal thoracic region was conducted followed by ultrasound-guided exploration (using a 13-16 MHz lineal ultrasound probe, Sonosite Inc., Bothewell, WA). The bilateral transverse vertebral processes were identified in a longitudinal section at the level of T6, the rhomboid major muscle, the erector muscles of the spine, and the fascia between the latter and the pulmonary pleura (Fig. 3). The puncture was performed at this level with a 22 G x 50 mm faceted tip echogenic needle, in cephalic-caudal direction. The infiltration of the local anesthetic was performed between the erector muscle of the spine and the T6 transverse process, injecting 30 mL of bupivacaine 0.25% on each side, with no associated complications.
Source: Authors.
Figure 3 Ultrasound image of the local anesthetic distributed between the rhomboid muscle and the erector spinae. EMesp=erector muscle of the spinae, PL=pleura, TP=transverse process.
The patient was placed in decubitus supine position and the surgical procedure began, which lasted for 1hour. The bar was removed and the findings indicated that it was partially ossified on both sides, with right margin prevalence. The patient remained stable throughout the procedure and 30 minutes before completion of surgery, a 100 mL elastomeric pump was placed with 12.5 g of metamizole and 300 mg of diclofenac sodium, at a rate of infusion of 2mL/hour, programed for 48 to 50hours. No opioids were used as analgesics or during the trans/postoperative period. The neuromuscular block was reversed with 0.5 mg of atropine and 1mg of neostigmine; the patient was then extubated free of complications.
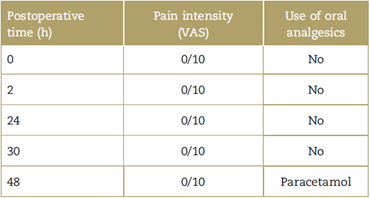
During the immediate postoperative period and follow-up until discharge after 30 hours, the patient was assessed using the verbal analog scale (VAS) and reported pain of 0/10. During the telephone follow-up 48 hours later, the patient said he had no pain, but reported having used paracetamol (Table 1). After 2 hours in the recovery room, the pinprick test was conducted on the anterior and posterior aspect of the thorax, documenting reduced bilateral sensitivity from T2 to T11 on the anterior and posterior thoracic walls; at the left para-sternal level, the patient still had 1/3 of the sensitivity, while on the right para-sternal level, the patient reported total absence of sensitivity.
Discussion
The procedure to place and remove the Ness bar is associated with several complications. In accordance with the level of deformity, pulmonary restriction, cardiac compression, and associated alterations should be considered; however, its management is invariable linked to significant postoperative pain.11 Placement and removal of the Ness bar can be extremely painful surgeries, and hence diverse anesthetic and analgesic methods have been reported in the literature, among which the most frequent one is general anesthesia using the thoracic epidural catheter.12
The thoracic epidural catheter for the management of Nuss procedures is considered the method of choice. The catheter may be in place for up to 3 days to facilitate pain management, and while the levels of analgesia are comparable with the intravenous techniques, it may take half of the time.11-13 Nonetheless, the catheter presents several frequent technical and clinical complications, that occasionally may be disastrous. The incidence of failure is up to 3.6%,14 with the possibility of sympathetic block, dural puncture, nerve and spinal cord injury,11 as well as failed placement because technically it is more difficult. Moreover, its use has been associated with extended hospital stays and higher use of opioids.13 The use of opioids is also associated with adverse effects, including nausea, vomiting, urinary retention, and constipation.15,16
Managing pain after a Nuss procedure, using only intravenous (IV) analgesic agents, has not offered clear benefits. The cases reported are usually few and contradictory, and it is not considered a reasonable option when other analgesic approaches are available.17
Multimodal pain management has recently experienced a boom in the literature, with a view to providing the most reasonable option for patient analgesia.18 This management includes the use of non-steroidal anti-inflammatory agents (NSAIDs), paracetamol, oral opiates, ketamine, gabapentin-like agents, incisional catheters, and the use of regional anesthesia.19-21 There are no reports on the removal of the Nuss bar using these techniques.
The key contribution of this case involves the high analgesic effectiveness of the ESP block, even 48 hours postop; the possibility to avoid the use of opioids; the low probability of complications, and the easy implementation of the procedure. There is limited literature describing the management of pain in Nuss procedures with the ESP block.
The multimodal approach herein described is consistent with the approach by Sánchez et al,11 that reported a case on the correction of pectus excauatum using an epidural catheter, NSAIDs, and metamizole, that resulted in satisfactory analgesia.
Nardiello and Herlitz10 is the only report using the ESP block as the primary analgesic method in the context of multimodal analgesia associated with the Nuss procedure, where satisfactory levels of analgesia were accomplished using a bilateral ESP block, in addition to metamizole, paracetamol, and IV ketoprofen, in 2 pediatric cases for the correction of pectus excauatum and pectus carinatum.
However, there are no reports on the use of the technique for the removal of the Nuss bar, which represents an additional novelty of our report.
This study may have some limitations since it is just 1 case. Though it may be logical to assume that the trauma generated by the removal of the Nuss bar is similar to the trauma resulting from the placement of the bar, this is just an assumption and not a fact. Moreover, the 48-hour follow-up was indirect, via telephone.
Conclusion
Notwithstanding the limitations, it may be concluded that this case points to the strong applicability of the ESP block as an element of postoperative analgesia, in the context of opioid-free multimodal analgesia in thoracic surgery, and represents an interesting field for future studies.
Ethical responsibilities
Protection of persons and animals. The authors declare that no experiments in human beings or animals were conducted for this research.
Confidentiality of the data. The authors declare that they have followed the protocols at their worksite on the disclosure of patient information.
Right to privacy and informed consent. The authors have obtained the informed consent of the patient described in the article and the informed consent of the mother. These documents are in the hands of the corresponding author.











 text in
text in