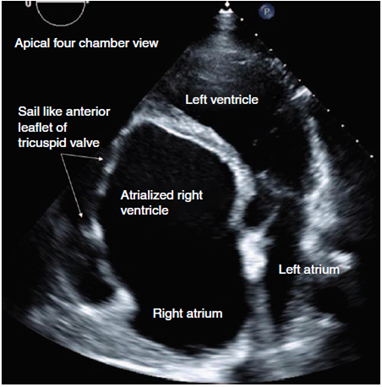
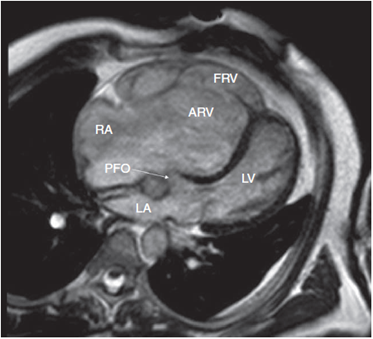
Ebstein anomaly is a rare congenital malformation of the tricuspid valve. The anterior leaflet is often redundant with a "sail like" appearance (Fig. 1, Video 1a, http://links.lww.com/RCA/A880 and Video 1b, http://links.lww.com/RCA/A881) while rudimentary septal leaflets are apically displaced (Video 2a, http://links.lww.com/RCA/A882 and Video 2b,http://links.lww.com/RCA/A883). This divides the right ventricle into a large atrialized and a small functional chamber. Tricuspid regurgitation is common.1,2 Commonly associated cardiac defects include patent foramen ovale (Fig. 2) and atrial or ventricular septal defects. In addition, presence of accessory conduction pathways can lead to preexcitation and arrhythmias. Clinical presentation varies with severity of tricuspid regurgitation. Severe disease often leads to right ventricular failure and cyanosis from right-to-left shunting with earlier presentation in childhood. Mild tricuspid regurgitation is well tolerated into adulthood. Definitive diagnosis requires cardiac magnetic resonance imaging and echocardiography.
Source: Authors.
Figure 1 Apical 4-chamber view displaying sail like anterior leaflet of tricuspid valve in Ebsteins anomaly.
Source: Authors.
Figure 2 Cardiac magnetic resonance imaging demonstrating key characteristics of Ebstein anomaly. ARV=atrialized right ventricle, FRV=functional right ventricle, LA=left atrium, LV=left ventricle, PFO=patent foramen ovale, RA=right atrium.
Occasionally, a large atrialized right ventricle can predispose to protrusion of the basal interventricular septum into the left ventricular outflow tract during systole resulting in narrowing of the outflow tract. This creates a venturi effect, leading to systolic anterior motion of the mitral valve leaflet and dynamic obstruction (Video 3a, http://links.lww.com/RCA/A884 and Video 3b, http://links.lww.com/RCA/A885).2 The accompanying images are from a 60 year old patient with bladder cancer who presented for cystectomy.
Anesthetic management during non-cardiac surgery focuses on minimizing pulmonary vascular resistance (PVR) and maintaining systemic vascular resistance (SVR). High PVR exaggerates right-to-left shunting through a patent foramen ovale worsening cyanosis. Increased pressures in the atrialized right ventricle, lead to protrusion of the septum into the left ventricular outflow tract, worsening dynamic obstruction with resultant fall in cardiac output. Hypoxia, hypercarbia, acidosis, hypothermia, and excessive positive end-expiratory pressure increase PVR and are avoided. Maintaining high SVR with judicious titration of vasopressors helps decrease dynamic left ventricular outflow tract obstruction and right-to-left shunting through the patent foramen ovale.1,3
Ethical responsibilities
Protection of people and animals. No experiments on people or animals were done.
Confidentiality of the data. All protocols at our institute were followed and patient or hospital identifiers have been removed from all images.
Right to privacy and informed consent. As patient and hospital identifiers have been removed, no informed consent was solicited for this production.











 text in
text in 


