Introduction
Heart failure is a growing healthcare problem worldwide, despite all the progress made in terms of pharmacological therapy.1,2 There is a particular group of patients with severe heart dysfunction that develop refractory symptoms to conventional medical therapy, which is associated with poor quality of life and high mortality rates.2,3
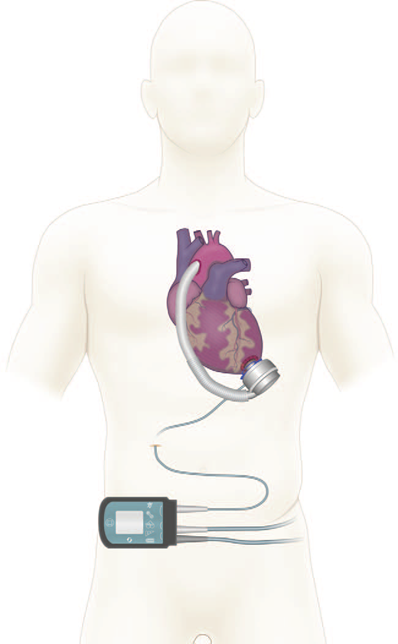
In response to the limited number of pharmacological options in this clinical setting, the use of ventricular assist devices (VAD) as destination therapy has been implemented in the last few years in patients with advanced cardiac failure; this strategy has proven to be effective, and provides adequate quality of life which is makes it increasingly popular around the world.4,5
During the perioperative period, one of the challenges of anesthetic management in patients undergoing The HeartMate 3 (Abbott, Chicago, IL, USA) type VAD implantation in postoperative pain control, an issue that becomes relevant in view of the type of surgical approach, the manipulation of intrathoracic organs, and the use of thoracotomies, which are all factors that may increase the occurrence of cardiopulmonary complications and hospital length of stay.6-8
Currently, the recommendation is to use multimodal analgesia, including regional techniques such as epidural analgesia or paravertebral block; however, the above-mentioned techniques may be limited by the use of anticoagulants during the perioperative period.5-8
Recently, Forero et al9 described the erector spinae plane (ESP) block as an effective approach to neuropathic pain of the chest wall and analgesia after thoracic surgery. This case report discusses the use of this rescue analgesia technique for the management of acute postoperative pain in a patient undergoing HeartMate 3 type VAD implantation.
Clinical case
Male, 74-year old patient with a history of chronic kidney disease stage 3, ischemic cardiomyopathy with left ventricular ejection fraction of 20%, and coronary heart disease with angioplasty plus stents, INTERMACS 4 (Interagency Registry for Mechanically Assisted Circulatory Support). The patient was managed by the heart failure team with levosimendan boluses and recurrent hospitalizations. Body weight: 65 kg; size: 1.63 m.
The patient received a HeartMate 3 type VAD implant as destination therapy; the surgical approach was sternotomy under balanced general anesthesia. The induction of anesthesia was with lidocaine, fentanyl, propofol, and vecuronium, and orotracheal intubation through direct laryngoscopy. The maintenance of anesthesia was performed with fentanyl, propofol, and sevoflurane infusion. A PCA (Patient Controlled Analgesia) regimen with bolus doses of fentanyl 20 μg, 5-minute block interval, maximum dose of 200 μg in 4 hours and oral acetaminophen 500mg every 6hours was established.
During the first 48hours after surgery, the patient experienced very severe pain-visual analogue scale (VAS) 8 to 10, predominantly in the left hemithorax, which was partially modulated with the PCA system and recorded a use of 540 μg of fentanyl in 48hours (Table 1). In addition, a left lung atelectasis was documented and interpreted by the treating physician as a complication secondary to the shallow breathing pattern caused by pain. Simultaneously, the patient presented with nausea, vomiting, and hallucinations that were considered adverse effects from the use of opioids. Consequently, 3 days after surgery, the decision was made to perform a rescue ESP block with interfascial catheter implant.
Table 1 Fentanyl patient controlled analgesia opioid use log.
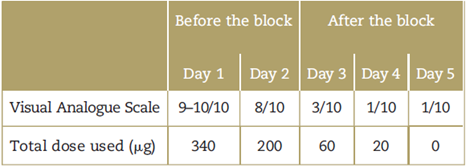
VAS=visual analogue scale. Source: Authors.
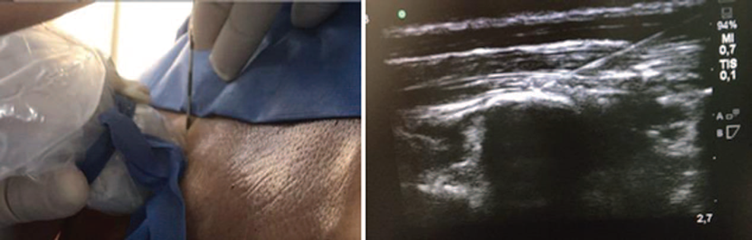
Since the patient was anticoagulated with unfractionated heparin infusion, the infusion was discontinued 4 hours before the procedure. The patient was transferred to the operating room after submitting the informed consent, and the ESP block was performed under ultrasound guidance, in accordance with the technique described by Forero et al9 with a single Tuohy No. 18 needle puncture in the left hemithorax, at T6 to T7; 0.25% bupivacaine with epinephrine, 0.5% lidocaine, and 4mg of dexamethasone were administered, for a total volume of 20mL. The interfacial catheter was inserted without any complications (Fig. 1). At the end of the procedure, the pain intensity dropped to mild (VAS: 1-3) and the anticoagulation was reinstated 2 hours after the procedure.
Follow-up: 1 rescue bolus with 0.25% bupivacaine 20 mL every 24 hours for 3 days through the catheter were required. Analgesia control VAS: 1 to 3 and reduced use of fentanyl at 80 μg at 96 hours, without any further adverse effects (Table 1). The decision was made to remove the catheter 5-days postimplantation, together with the thoracotomy tubes, and discontinuation of heparin for 4hours. There were no complications.
Discussion
Long-term VADs as destination therapy or as bridge therapy to recovery are increasingly being used for the management of patients with refractory heart failure.2-5 Currently, one of the challenges in perioperative management is adequate control of analgesia. This is because the surgical technique involves sternotomy or thoracotomy,5,10 and in the particular case of the HeartMate 3 (Abbott, Chicago, IL, USA) device, its intrapericadial localization at the level of the left ventricular apex in patients with cardiomegaly, positions the device against the rib cage5,10 (Fig. 2), which simultaneously increases the pain intensity from moderate to severe and in some cases may lead to difficult pain management, with a higher incidence of pulmonary complications due to the shallow breathing pattern, hypoventilation, and inability to produce effective coughing, which promotes the development of atelectasis and pneumonia, with increased morbidity and mortality.11 In addition, when oxygenation and ventilation are compromised, increased pulmonary vascular resistance is encouraged, which may have a negative impact on the right ventricular function,12 hence disrupting the hemodynamic performance and the patient's evolution, resulting in extended hospitalization.
In our institution, the management of analgesia for heart surgery patients is done using the intravenous fentanyl PCA system and oral acetaminophen. However, the management of acute postoperative pain in HeartMate 3 patients has been challenging in terms of analgesia control because occasionally it may require rescue boluses with other morphine-like opioids, increasing the probability of adverse effects.
Consequently, the decision was made to look for a rescue alternative to help us achieve adequate pain control and allow satisfactory cardiopulmonary rehabilitation. The ESP block was then an interesting option.
The ESP block at the thoracic level was initially described by Forero et al9 as a regional technique for peripheral block at the interfascial level, administering a certain volume of local anesthetic agent into a deep place of the erector spinae muscle. The anesthetic agent spreads longitudinally at the cephalic-caudal and ventral-dorsal level, impregnating the ventral and dorsal branches of the spinal root nerves in the thoracic region, extending 3 to 5 dermatomes at the upper and lower levels of the puncture site, according to the findings of the anatomical dissection in cadaveric models and confirmed with radiological studies.13
In addition, there is impregnation of the local anesthetic agent at the level of the thoracic sympathetic chain, which blocks the autonomic response and enhances visceral pain control.9 It must be highlighted that due to its easy identification with ultrasound, the puncture site, and the distribution of the anesthetic agent at the interfascial level, this represents a safe technique for the management of somatic and visceral pain. Nevertheless, there needs to be awareness of the fact that it only produced ipsilateral block at the puncture site and hence 2 punctures will be needed to achieve a complete approach in surgical procedures with central sternotomy-like incisions.
Since the technique was first described in 2016, multiple papers have been published in the literature on the analgesic use of the ESP block for rib fractures,14 non-cardiac thoracic surgery9,15 and breast surgery.16,17 In heart surgery, the information is limited; some successful cases have been described for thoracic approaches10 and in minimally invasive surgery.18 Recently, the use of the ESP block was reported in patients undergoing left VAD implantation through thoracotomy, using continuous infusion of local anesthetic for analgesia control purposes, with optimal results.10 In this particular case, maintenance was provided with intermittent boluses (daily), but when comparing the results, similar behaviors may be observed with regards to pain perception and the use of opioids.
Conclusion
The US-guided ESP block at the thoracic level was an innovative, easy, and safe regional technique, which provided an effective postoperative management option as part of the multimodal analgesia strategy in a patient undergoing HeartMate 3 type VAD implantation.
Patient opinion
The patient said to have experienced considerable improvement and comfort after the procedure. After doing a risk-benefit analysis, the patient stated that he would highly recommend the procedure and agree to undergo the procedure again.
Ethical considerations
Protection of persons and animals. The authors declare that all the procedures were conducted in accordance with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of the data. The authors declare that their usual workplace protocols on the disclosure of patient information were followed.
Right to privacy and informed consent. The authors have obtained the informed consent of the patient discussed in this article.











 text in
text in