Introduction
Submental intubation (SMI) was first described in 1986 by Hernández Altemir to treat the airway in adults with maxillofacial trauma for whom nasotracheal intubation is contraindicated due to skull base fractures, comminuted midface fractures, nasal septum defects causing physical obstruction to the airway and cases where orotracheal intubation is not ideal due to the desire to create transsurgical dental relationships. Therefore, SMI constitutes an intraoperative alternative to tracheostomy.1,2 Although the SMI surgical technique employed for children is the same as in adults, few articles have reviewed its pediatric use. Since its initial description, the prescription range for SMI, for both children and adults, has broadened and now includes orthognathic, reconstructive, and skull base surgery.3,4
SMI's main advantage is that it avoids the need to perform a tracheostomy and its related morbidity. SMI requires less time to complete and the resulting scar is aesthetically acceptable. In addition, its mini mum postoperative care and easy revertability are some of the notable benefits of this technique over tracheostomy.3
This research presents 2 cases of successful pediatric SMI. In accordance with hospital guidelines for research reporting, both cases were anonymously reported upon obtaining the patients' informed consent.
Case 1
Female patient, 7 years and 7 months old, admitted into emergency services with a diagnosis of secondary facial trauma caused by a bicycle fall, with extrusive tooth displacement in dental organs 11, 21, and 22, bilateral parasymphyseal fracture and nasal fracture with lateral displacement evidenced in the tomography. The patient was programed for open reduction and internal fixation of jaw fracture.
Anesthetic technique: Sevoflurane anesthetic induction through inhalation maintaining spontaneous ventilation, intravenous (IV) coinduction, and orotracheal intubation through flexible fibrobronchoscopy on second attempt with armed endotracheal tube (ETT) no. 5 with balloon.
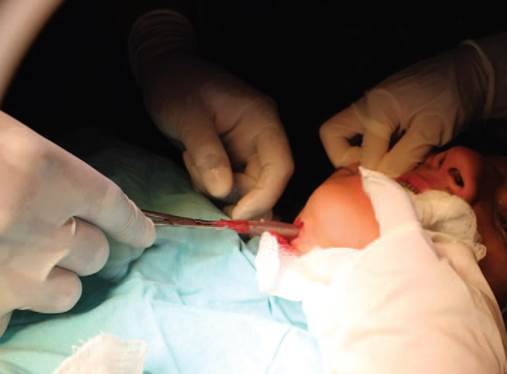
Surgical technique: Derivation following Hernández Altemir's sequence,2,5 considering Nyáràdy's2-2-2 proposal (2-cm-long incision, 2-cm away from the midline, and2-cmmedialinparallelwiththejawinthe submental area) (Fig. 1). Blunt dissection with clamp was performed, in contact with the lingual side of the jaw until reaching the mouth floor, displacing the skin muscles at the neck and mylohyoid and creating an intraoral tunnel for ETT passage; ETT removal was conducted using a hemostat (Fig. 2). ETT is attached to the skin with Nylon 3-0 suture. Proper ETT positioning of the ETT is checked and it is connected to the anesthetic circuit (Figs. 3 and 4). The tube is transferred to the oral position again before full removal. The submental incision is closed (Fig. 5), with intraoral closing deemed unnecessary.2

Source: Authors.
Figure 3 ETT fixation and placement of ETT connection for subsequent anesthetic circuit connection (Case 1). ETT=endotracheal tube.
Case 2
Female patient, 17 years old, diagnosed with class III dentoskeletal deformity due to anteroposterior maxillary and nasal septum deformity, programed for a Le Fort I osteotomy (5 mm maxillary advance) and for rhinoseptoplasty, at the patient's request.
Anesthetic technique: IV induction and orotracheal intubation through a GlideScope (Verathon, Bothell, WA, USA) videolaryngoscope on first attempt, armed ETT no. 6.5 with balloon.
Surgical technique: Submental derivation with the same technique as in Case 1 (Figs. 6-10).
There was no accidental ETT removal or lesions. The time required to perform the SMI was less than 10minutes. Apnea time (time disconnected from the circuit) was less than 2 minutes, with no significant oxygen desaturation. No greater complications were observed. No alterations of the lingual motor or sensitive nerves were registered. The postoperatory scarring of the submental wound was only detectable upon careful inspection with neck hyperextension. None of the cases showed traces of keloid or hypertrophic scarring.
Discussion
SMI is a valuable, safe, and quickly executable alternative to restore the airway in pediatric cases.
There are multiple modification proposals to the original technique for adults with an aim to decreasing complications (to reduce the risk of intraoperatory bleeding, lesion to close anatomic structures, and to diminish tube damage).6 Green and Moore7 propose a sequence with 2 ETT with non-detachable universal connectors; MacInnis and Baig5 describe a 2-cm midline incision posterior to the submandibular duct, with less bleeding; Hernández Altemir and Hernández Montero8 modified the technique using a reinforced laryngeal mask, allowing the use of SMI in severe laryngotracheal trauma; Nwoku et al9 performs an incision attempting to avoid touching important structures on the mouth floor; Mahmood and Lello10 propose making a 1-cm midline incision between the submandibular duct and lingual gum and mouth floor recession in order to decrease bleeding and avoid contact with any important structure; Hernández Altemir et al,11 in 2003, used a reinforced combitube to aid the pharyngeal plugging. It is relevant to note that, at the moment, no specific modifications for pediatric patients have been proposed.
In surgical cases benefitting from SMI, there are 3 main advantages: the ability to ensure dental occlusion intra-operation, ETT removal from the surgical site, and greater tissue recession for procedures at the base of skull through a transmaxillary approach (once the osteotomy is completed, the maxillary is receded downward to clear the visual field, which is limited in cases of nasal or orotracheal intubation).
Comparing SMI with tracheostomy, SMI shows no significant greater complications.12 Tracheostomy complications include hemorrhage, surgical emphysema, surgical site infection, recurring larynx nerve lesion, tracheal stenosis, poor scar aesthetics, tracheoarterial fistula, and death.2 SMI has less reported complications, is less costly and requires less time than a tracheostomy and leaves an aesthetically acceptable scar.
No complications were observed in our case; however, the gravest reported complication is accidental trans-operatory extubation. Amin et al13 and Sharma et al14 reported partial accidental extubation in pediatric cases when the tube is pushed through the submental incision. The most frequent late complication was the development of superficial skin infections.2,6 Damage to the ETT is another potential problem that arises during the change of tube position from oral to submental position. Lesions may also arise during maxillofacial procedures, either due to a drill bit when placing a rigid fixation or to a saw blade during osteotomies, particularly in the chin. Other reported minor complications include the formation of orocutaneous fistula, tube displacement or obstruction, transient paresthesia of the lingual nerve, venous hemorrhage, and mucocele formation.2,6
There are reports of usefulness of this approach in facial trauma patients, and less frequently in orthognathic surgery cases. This report shows the case of a patient with multiple facial fractures for whom nasotracheal intubation was contraindicated, due to fractures in the midface and nasal bones and to the need of intermaxillary fixation. The second case corresponds to an orthognathic surgery patient who needs ensured occlusion to fixate maxillary advance, as well as a rhinoseptoplasty, which impeded nasal intubation; the SMI allowed to observe the real modification of the nasal base and the upper lip without ETT interference. With nasotracheal intubation, the intraoperatory evaluation of changes in the nasolabial complex, midline evaluation and incisor teeth exposure during orthognathic surgery cannot be performed with the necessary precision. In addition, complementary procedures, such as simultaneous rhinoseptoplasty, cannot be performed without changing the tube.
Green and Moore proposed a modification to the SMI; for our patients, we preferred to use Hernández Altemir's sequence, because of the lesser apnea time (with the modification, the time is greater than when attempting a second laryngoscopy by disconnecting the tube and moving it to the submental route). In addition, damages to the balloon of the ETT cuff due to the repeated contact between the Magill forceps and the balloon when performing the second intubation.7
Our proposal to decrease accidental extubation is to deflate the balloon of the ETT cuff by only passing the ETT through the submental route, leave the balloon within the oral cavity and make an incision of maximum 1 to 1.5 cm in children, enough to allow ETT passage. We recommend passing the ETT through the derivation in the shortest time possible, decreasing apnea time as much as possible. The child presents lesser apnea tolerance due to greater oxygen consumption, decrease of residual functional capacity, a tendency for alveolar collapse, rapid hypercapnia, and respiratory reflex development with potential morbidity, such as laryngospasm and bronchospasm.
In our experience, we had a clear intent to keep the procedure conservative given the patient's anatomic features.
Conclusion
SMI in maxillofacial surgery is a viable and safe technique for pediatric patients with secondary fractures following facial trauma and in orthognathic surgery, serving as an alternative to tracheostomy when no intraoperatory nasal or tracheal intubation is indicated.
Ethical responsibilities
Protection of persons and animals. This research did not entail the performance of any experiment neither in human beings nor in animals.
Data confidentiality. The authors hereby declare that no patient data appear in this article.
Right to privacy and informed consent. The authors obtained informed consent from the nonidentifiable patients referred to in this article. This document is the property of the correspondence author.











 text in
text in