Introduction
Cardiac arrest (CA) is the sudden and, in principle, potentially reversible interruption of circulation and spontaneous breathing. According to the literature, the main etiology is cardiovascular disease,1-3 with a general incidence of 375,000 adults/year in Europe and 162,000 adults/year in the United States; however, in intensive care units (ICU), it varies between 5.6 and 78.1 for every 1000 patients admitted.1
In Colombia, according to the statistics agency Depar tamento Nacional de Estadistica (DANE), 68,640 deaths related to cardiovascular diseases in patients over 15 years of age were reported in 2017.4 Attempts have been made at describing the local epidemiology of CA in different settings. In 2011, Valencia et al5 reported that, in Cali, 80% of cases occurred in the emergency service and 20% in the ICU.
It is estimated that close to 200,000 hospital admissions are complicated with a case of CA every year, with a survival of only 20% at discharge6 and a large proportion of survivors with sequelae. There are differences between arrests occurring and addressed in the hospital and those occurring in an out-of-hospital setting,7,8 perhaps due to the fact that, in the latter, resuscitation maneuvers are initiated later. Likewise, survival after in-hospital CA may vary depending on the service in which it occurs: 16% in the ICU, 23% in the emergency department, and 12% in inpatient units.9
However, no studies have been conducted in Colombia describing the clinical characteristics of patients with CA in ICU, their survival, not to mention the neurological sequelae after discharge. The objective of this study was to determine the clinical characteristics of CA in patients hospitalized in different ICU of the Medellin metropolitan area over a 12-month period.
Materials and methods
Observational study that included patients over 18 years of age who went into CA in several ICUs of the Valle de Aburrá and Medellin metropolitan area over a 1-year period (January 2017-January 2018). The protocol was submitted for evaluation and approval by the Ethics Committee of Universidad de Antioquia and the different participating institutions: Hospital San Vicente Fundación (4 ICUs, 45 beds); IPS Universitaria (3 ICUs, 32 bed); and ESE Hospital Manuel Uribe Ángel (1 ICU, 14 beds).
Each of the studied units had a 1:2 practical nurse: patient ratio and were covered around the clock by critical and intensive care medicine specialists.
The inclusion criteria were patients over 18 hospitalized in the ICU who went into CA; pregnant patients and patients admitted to the ICU because of post-CA state were excluded.
After the protocol was approved by each of the participating healthcare institutions, a coordinator re sponsible for completing the relevant electronic data collection form was appointed at each site. In addition, a periodic audit of patient data reported as eligible was conducted by the principal investigator team. The primary source for data collection was the individual clinical record.
Four types of ICU were considered for the analysis: cardiovascular, surgical, medical, and polyvalent or mixed. The epidemiological visualization window was 12 months and 100% of the patients with eligibility criteria in the three healthcare sites were effectively included in the study analysis.
Statistical analysis
Qualitative variables are presented in the form of proportions or frequencies. The Shapiro-Wilk test was used to run the normality tests for quantitative variables. Variables showing a normal distribution are presented in terms of means and standard deviations. Variables with non-normal distribution are expressed as medians and interquartile ranges.
An exploratory analysis was conducted among the variables in accordance with the type of ICU. Chi square (χ2) homogeneity tests were used for qualitative variables, ANOVA for normal quantitative variables, and the Kruskall-Wallis test for non-normal quantitative varia bles. All analyses were carried out using the SPSS 24 statistical software package.
Results
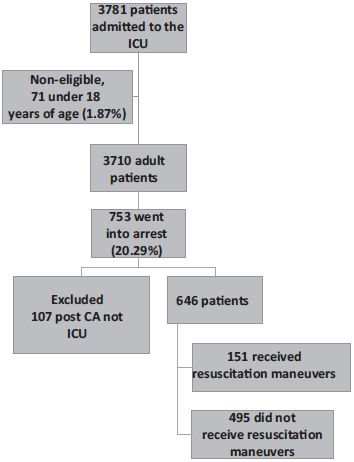
In 3781 patients admitted to the different ICU during the study period, 646 CA events were analyzed, and, of these, 151 effectively received resuscitation maneuvers (Fig. 1).
The overall incidence of CA was 17.1% (95% confidence interval [CI]: 15.9%-18.3%): 13.9% for Hospital Manuel Uribe Ángel (95% CI: 11.6%-16.7%); 18.8% for Hospital Universi tario San Vicente Fundación (95% CI: 17%-20.8%) and 16.7% for IPS Universitaria, Leon XIII campus, (95% CI: 14.9%-18.7%) (P = 0.4761).
The overall incidence rate was 21 for every 1000 days of ICU stay. When this event is analyzed in patients who can receive resuscitation, the incidence is 4.0% (95% CI: 3.4%-4.6%).
Table 1 shows the characteristics of all CA events that occurred in the ICUs. Annex 1 shows the characteristics of effectively resuscitated patients in the ICU.
Table 1 Clinical and demographic characteristics of all CA in the ICU.
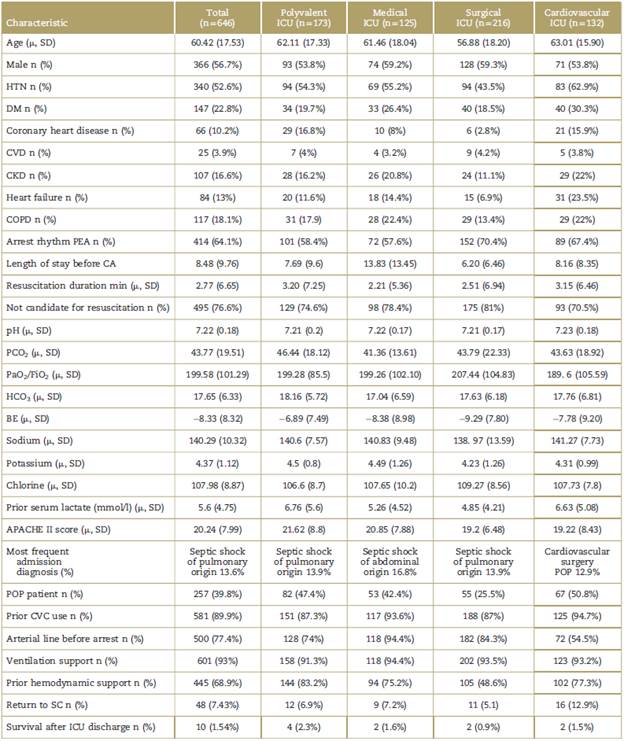
μ = means, BE = base excess, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVC = central venous catheter, CVD = cerebrovascular disease, DM = diabetes mellitus, HCO3 = bicarbonate, HTN = chronic arterial hypertension, PaO2/FiO2 = oxygen pressure and inspired oxygen ratio, PEA = pulseless electrical activity, POP = postoperative, SC = spontaneous circulation, SD = standard deviation.
Source: Authors.
The most common cause of CA in resuscitable patients in the ICU was septic shock in close to 50.3% of all cases, followed by cardiogenic shock in 14% of cases. This relationship was the same in all the types of ICUs studied (Table 2, Fig. 2).
Table 2 Attributable causes of CA in patients who underwent cardiopulmonary resuscitation.
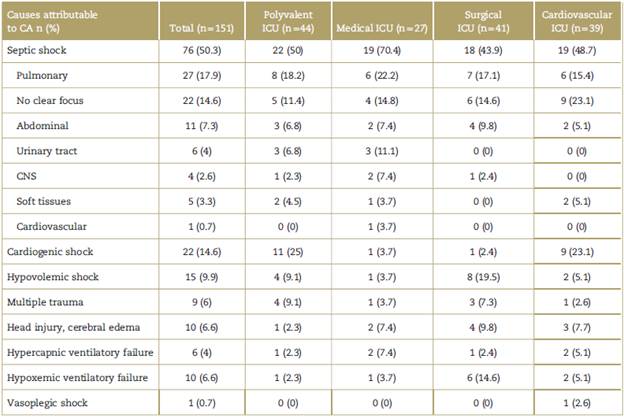
CA = cardiac arrest, CNS = central nervous system, ICU = intensive care unit.
Source: Authors.
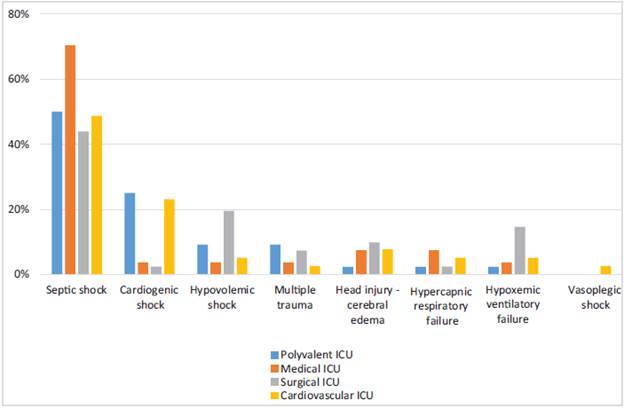
Source: Authors.
Figure 2 Attributed CA causes according to the type of ICU. CA = cardiac arrest, ICU = intensive care units.
Median stay before CA in resuscitated patients was 3 days and the most common arrest rhythm was pulseless electrical activity (PEA) in 54.3%. Median duration of resuscitation maneuvers was 9 minutes, with no differ ence between the different rhythms.
Of the total number of CA patients who received cardiopulmonary resuscitation (CPR) maneuvers, 25.8% returned to spontaneous circulation, but only 6.6% were discharged alive from the ICU.
For patients with CA who returned to spontaneous circulation, mean age was 55.87 years with a median resuscitation time of 7.28 minutes, none received thera peutic hypothermia during the postarrest period, and only 7.69% of the arrest rhythms were amenable to defibrillation.
The median neurological score for overall performance Cerebral Performance Category (CPC) was 1 (interquartile range [IQR] 1-3) and the median on the Glasgow scale was 15 (IQR 11-15). Of the 10 patients who were discharged alive from the ICU, only 5 were discharged alive from the hospital, with a median CPC of 1 (Table 3).
Discussion
Studies on the incidence and characteristics of CA in ICU are not found frequently in the world literature, contrary to what could be expected. This limits the possibility of implementing strategies to lower the incidence.
CA is a catastrophic event associated with high mortality and considerable morbidity.1 However, statistics show that survival after in-hospital CA is 3.8 times higher than for out-of-hospital arrest7 given that the possibility of returning to spontaneous circulation and minimizing neurological damage depends on how soon basic but high-quality resuscitation maneuvers are initiated and the timely availability of technology resources. This means that expected outcomes are better in CA that occurs and is managed in the hospital setting.
However, differences are found inside the same hospi tal, depending on the care setting. Better results are found in the surgery area because of the characteristics of the surgical patients, continuous monitoring and specialized care.10
For patients receiving care in the ICU, considerations are different from what is found in other in-hospital settings, because of continuous telemetry monitoring and immediate availability of specialized human resour ces. Although this would lead to the assumption that outcomes ought to be better in this population, patients receiving care in the ICU are the most complex and severely ill, resulting in worse outcomes in view of their limited physiological reserve, as was shown in this report.
Efendijev et al11 conducted a systematic review of the literature on the incidence and prognosis of adult patients who went into CA while in the ICU. Their results revealed a prevalence of ICU CAs ranging between 0.6%9 and 7.8%12 and an incidence ranging between 5.6 and 78.1 for every 1000 admissions. This study identified a prevalence of 4% and an incidence of 40 cases of CA that received CPR maneuvers for every 1000 patients admitted. Moreover, a rate of 4.9 CA for every 1000 ICU bed days was found, a rate that was not reported in other studies.
ICU patients are often labeled as non-resuscitable in advance due to their poor prognosis, either because of their current condition or their underlying disease. Of the 3710 eligible patients, there were 495 (13.3%) CA events which were not managed with CPR maneuvers because of the advance do not resuscitate directive from the patient or the family, or because of medical futility considered by the attending team. In the literature, advance directives to not resuscitate were found in 0.3% of cases, much lower than the result in this study.
When analyzing CA, it is critical to identify the initial arrest rhythms, because of differences in management and prognosis. In our study, the rhythm found most frequently in patients with CA who were resuscitated was PEA in 54% of the events, similar to the finding by Efendijev et al1 in their systematic review in which non-defibrillatable rhythms (pulseless electrical activity and asystole) were the most frequent, ranging between 55% and 84% of the events. Considering the underlying pathophysiology of coronary disease and heart diseases in general, a higher frequency of defibrillatable rhythms was expected as initial CA presentation in patients hospitalized in cardio vascular ICUs; however, non-defibrillatable rhythms were found to have the highest incidence, at 46.2%. This could perhaps be attributed to occupancy by a good number of cardiac surgery patients in whom CA is associated with complications such as cardiac tamponade, hemorrhagic shock, bradyarrhythmias, and vasoplegic shock.
The American Heart Association13 reported that hypo thermia was used in 35.6% of the patients who returned to spontaneous circulation after CA as a neuroprotective strategy in the ICU (maintaining the temperature between 32 and 34 °C), in particular if the initial arrest rhythm was defribillatable. In this study, none of the 10 patients who returned to spontaneous circulation received that therapy. This may be explained by the change in the level of recommendation between the 2010 and the 2015 guide lines, which went from recommending deliberate hypo thermia to targeted temperature management between 32 and 36°C.
The present study has several limitations. First, being a descriptive study, no comparisons can be made to provide definitive conclusions regarding important outcomes. Second, given the sporadic occurrence of the event, data were collected from the clinical record, limiting the information to that documented by the treating physicians, which results in potential information bias. In addition, the Ulstein method, which allows all the participants in the management of CA to collect data, was not used in this study. Third, the number of patients may be limited, a drawback that we tried to address with the multicenter design and a 12-month data collection period. Fourth, although for the analysis ICUs were classified according to their designated use in each site as medical, polyvalent, surgical, or cardiovascular, in reality they are all polyvalent units due to bed occupancy factors.
Table 3 Resuscitation characteristics of all CA events occurring in the ICU in patients who received CPR maneuvers.
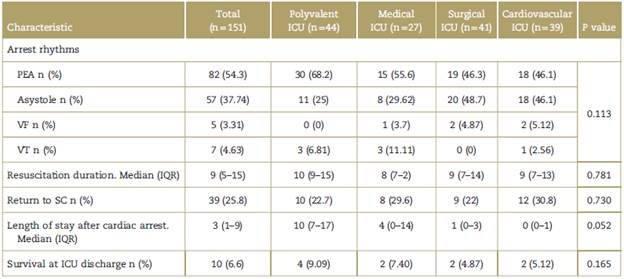
CPR = cardiopulmonary resuscitation, IQR = inter-quartile range, PEA = pulseless electrical activity, SC = spontaneous circulation, VF = ventricular fibrillation, VT = ventricular tachycardia.
Source: Authors.
Conclusion
Although infrequent, CA in the ICU is catastrophic and associated with high mortality, both at discharge from the ICU as well as from the hospital. The local epidemiology in terms of incidence and rate of event occurrence in the ICU is consistent with the epidemiological data reported in the literature; however, the incidence of "non-resuscitation" in the ICU is by far higher than that reported internationally.
Moreover, it is clear that the few patients that are discharged alive after an event of this type have an apparently good neurological prognosis.
However, studies with a better methodological design are needed to identify factors that may potentially improve survival after CA in ICU and the main causes of "non-resuscitation" in our ICUs.
Ethical responsibilities
Human and animal protection. The authors declare that the procedures followed were in compliance with the ethical standards of the responsible human experimenta tion committee, and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that they have followed the protocols of their institutions pertaining to patient information disclosure.
Right to privacy and informed consent. The research was approved by the institutional ethics committee in minutes no. 005 of March 31, 2016 which state the waiver of the informed consent requirement given that the study is classified as having no risk in accordance with Ministry of Health Resolution 8430 of 1993. The corresponding author is in possession of this document.











 text in
text in