Introduction
Patient safety includes a set of processes, instruments, and methodologies based on scientific evidence, which seek to minimize the risk of suffering a reportable event with unwanted effects (REUWEs), or to mitigate the consequences of its occurrence during the process of health care.1 This implies the identification and reporting of the risks associated with patient care, which include clinical incidents and REUWEs, the latter, defined as situations that generate unintentional damage to the patient resulting from the provision of the health service2 and clinical incidents, which represent events that did not cause harm but had the potential to do so3 in order to implement the necessary safety barriers to protect the patient and improve the safety culture at the institutional level through the design of improvement strategies.4
Several studies have reported that the most commonly used systems in the clinical setting for the notification of REUWEs or clinical incidents are (a) the passive system through the method of voluntary reporting or self-reporting,5-7 which is carried out by any health workers who identify unsafe actions that represent a risk to patients; it is carried out confidentially and sometimes anonymously; and (b) the active system, which actively and systematically collects information on patient care, looking for latent failures and REUWEs, generating comprehensive reports that assess the possible risks during the entire patient care process.7,8
There is controversy over which system is the most appropriate to implement in health institutions, given not only the advantages and disadvantages that each of them presents, but also due to the characteristics of the context and organizational culture in health institutions. Passive reporting systems (RSs) have a strong appeal since their implementation is relatively easier and less expensive than the active RS; however, their main disadvantage is underreporting,9 that it is partly due to the fear that an error occurred during patient care becomes evident, and that can generate punitive repercussions to the members of the medical teams involved,10 and the lack of reporting culture in the institutions. On the other hand, the active RS requires a greater investment of time and resources to correctly execute a successful system, which is a major inconvenience from the perspective of health institutions, which have finite resources for patient care.11
An event search methodology in active RSs is Baker's methodology,12,13 which allows the detection of screening events through the application of an instrument that contains 11 criteria (screening events), which help to detect situations that suggest something unexpected happened and should be analyzed in depth. This methodology that has been previously validated in Colombia by the health technology and policy assessment group (GETS in Spanish) at Universidad Nacional de Colombia2,12 is applied to a certain sample of randomly selected medical records, to do an active search for clinical incidents and REUWEs.13,14
One of the objectives of accreditation of quality of the institutions providing health is the strengthening of patient safety. Regarding the event report, in Colombia, the notification of the REUWEs has been recommended suggesting the use of institutional self-report formats. Some institutions manage an online application in which health workers make reports of unsafe actions, which are characterized by behaviors that generate health-care practices that have the potential to cause REUWEs,9,15 which are subsequently analyzed by the patient safety manager.
The available evidence on the direct comparison of performance between active and passive RSs to detect a true REUWE, given that there is a screening event or an unsafe action, is insufficient. In consideration of the above, this study was developed, which aims to determine the operational performance in terms of the positive predictive value (PPV), concordance, and coincidence of the passive self-report system, compared to the active RS, for the detection of clinical incidents and REUWEs, in a health-care institution (Teaching Hospital) in Bogotá, Colombia.
Methods
Design and population
A cross-sectional study assembled in a cohort, in which were included patients that were hospitalized more than 22 hours at the surgical service during May to July 2027 period. There were not exclusion criteria. All patients that accomplish inclusion criteria were part of the population base.
Sampling
Active RS: A random sample of 200 medical records of patients hospitalized in the surgery service. The sample size was calculated based on the universe of patients hospitalized in the surgery department in the same period (N: 2200), 95% confidence level and 3% margin of error. Details on the methodology of the application of the active methodology are available in a previous publication.2
Procedure
The source of information for the passive RS was the database from the institutional self-RS, which contains information on unsafe actions, clinical incidents, and REUWEs reported voluntarily. The self-report in the institution is made in an electronic form, external from the medical record. All the institution's workers have access to this form from the computers. The reported data are analyzed by the patient safety office of the institution. Duplicate events were excluded from the analysis after confirming in the medical record that it was the same case or event.
The source for the active system was the medical records of the random sample of patients included and reviewed using the screening event tool of Baker2,23 that was carried out in the study about frequency of REWES at the institution (for more detail about its methodology refer to Ref.2).
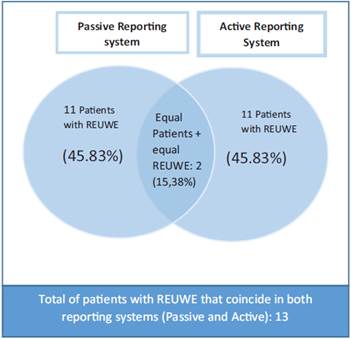
The review of the passive reporting database was done by an experienced investigator, the confirmation and classification of the study events was done in duplicate by 2 investigators based on the reconstruction of the case and the information in the medical record. The reported cases were classified as extra-institutional event, clinical incident, REUWE, or non-reportable event; following the algorithm of classification of safety events of the institution (Fig. 1).
Source. Authors from definitions taken from Estrada-Orozco et al2 and Pohlman et al.10
Figure 1 Safety event classification algorithm.
The analysis of the database of active reporting and classification of cases, such as screening event, clinical incident, and REUWE, was done by consensus of a group of experts,2 after the review of the medical record and following the algorithm of classification of safety events (Fig. 1).
After having the characterization and final classification for the patients with positive screening events from both RSs (active and passive), the data were analyzed comparatively.
Operational definitions
Clinical incident: It is an event that occurs during the clinical care of a patient, does not cause harm, but reflects failures in the care processes.3
REUWE unintentional injury caused by medical care, which causes delay in discharge, prolonged stay or disability, and that can threaten the life or cause the death of the patient. The developer group of this work has preferred the use of the term REUWE on adverse events, since we intend to reduce the punitive stigmatization associated with the adverse term, as well as encourage the report by including this term (reportable) to the denomination.
Non-reportable event: Another type of event that is reported and not related to unsafe patient care: complaints or claims, suggestions related to the food, environment, and hotel service.
Unsafe action or screening event: An event that can alert you to the increased risk of occurrence of a clinical incident or REUWE.2,9
Extra-institutional events: These are events that occurred outside the institution providing the health service.
Analysis
The Excel program and the Stata Version 14 statistical software were used. A descriptive analysis of the cases reported in the self-RS was made, presenting the relative and absolute frequencies according to the type of event, member of the medical team that reported, period of the day, and the department or reporting service. (Details of the analysis of the active RS and its results are available in Ref.2.)
For both RSs, the cumulative incidence of patients with REUWEs and clinical incidents, as well as PPVs (probability of being a true incident/REUWE since it was detected by the RSs) for their detection were calculated. The results were presented according to 2 units of analysis: first, reported events and the second, patients with reported events.
The level of concordance is only able to measure the patients who presented events and were detected by both RSs (unit of analysis: patient). However, the coincidence allows estimating for this group of concordant patients, if the events detected were the same or not. Mathematically, it is the proportion of this group in which the events detected by both RSs coincide (unit of analysis: REUWE). For the concordance analysis in the detection of patients with REUWE between the 2 RSs, the Kappa coefficient and its expected error were calculated. The proportion of reports that coincided (by REUWE and by patient) in both databases was also calculated. All results were presented with their respective 95% confidence interval (95% CI).
Ethical aspects
According to the general considerations contemplated in the declaration of Helsinki(16 and the local resolution 8430 of 1993 of the Ministry of Health and Social Protection,(17 the present investigation is considered without risk since secondary sources were used for the extraction of the information (databases), no direct intervention was performed on the patients, nor was any variable modified on the study subjects. The study was approved by the ethics committee of the National University of Colombia through Act 36084-2016.
Results
A total of 1200 patients were hospitalized in surgery during the period of May, June, and July 2017. Forty seven patients of the surgery service were informed at the base of the self-report system (passive report) for presenting at least 1 unsafe action during their medical care in this period of time. A total of 77 unsafe actions occurred in 47 patients (1.6 unsafe actions per patient) hospitalized in the surgery service, after excluding duplicates (14 reports). Of the 77 reports of unsafe actions, 30 reports (38.9% 95% CI 27.4248.58) were classified as REUWE. Details are given in Table 1.
Table 1 Frequency of security events detected by the self-report system (passive report).
| Reporting system | ||
|---|---|---|
| Self-report n:91 | ||
| n Events (%) | 95% CI | |
| Unsafe actions/screening evTFN2ents* | 77 (84.6) | 77.2-92 |
| Unsafe actions reported more than once | 14 (15.38) | 8-22.8 |
| Unsafe actions, N:77 n (%) | 95% CI | |
| Clinical incidents | 40 (51.94) | 40.97-62.91 |
| REUWEs | 30 (38.97) | 27.42-48.58 |
| Non-reportable events | 7 (9.09) | 8.8-9.2 |
CI= Confidence interval, REUWEs = reportable events with unwanted effects.
* After removing duplicates or unsafe actions reported more than once.
Source: Authors.
The most reported unsafe actions in the passive system by health teams were chemical phlebitis 20 unsafe actions (23%; 95% CI 5.52-20.46), skin lacerations due to fixation 8 unsafe actions (20.4%; 95% CI 3.62-27.27), and pressure zones 5 unsafe actions (6.5%; 95% CI 2.02-22.97); other unsafe actions are detailed in Table 2.
Table 2 Unsafe actions reported in the passive reporting system.
| Unsafe actions reported in the passive reporting system (N: 77) | n (%) | 95% CI |
|---|---|---|
| Non-performance of a scheduled medical procedure | 4 (5.2)* | 0.26-10.13† |
| Extra-institutional events | ||
| Poorly marked laboratory samples | ||
| No administration of medications or nutrition | ||
| Loss of material during a procedure | ||
| Falls | 3 (3.9)* | 0.0-8.20† |
| Self-extubation | ||
| Removal of the catheter by the patient | ||
| Inadequate administration of medications | 2 (2.66)* | 0.0-6.13† |
| Delay in performing a scheduled medical procedure | ||
| Error in the dispensing of nutrition | ||
| Loss of dental pieces and the | ||
| Posttransfusion reaction of blood products | ||
| Occupational accident | 1 (1.3)* | 0.0 to 3.81† |
| Self-medication of a patient | ||
| Swallowing of food in a patient with an orotracheal tube | ||
| Diarrhea during surgical procedure | ||
| Failure in venous access | ||
| Therapeutic failure of the medication | ||
| Puncture with a pre-filled syringe (biological accident) | ||
| Non-availability of nutrition in pharmacy | ||
| Lack of informed consent for surgery | ||
| Patient with fever in surgery rooms | ||
| Cardiac arrest with hypoxemia | ||
| Adverse drug reaction | ||
| Surgical reintervention | ||
| Referral to surgery without communication to the head of service | ||
| Sampling of blood to wrong patient |
The organization of unsafe actions in the table responds to a frequency criterion in its presentation and not to a special classification. CI = confidence interval.
* Absolute number and relative frequency.
† 95% confidence interval for each unsafe action reported.
Source: Authors.
The services with the highest use of the passive system to report unsafe actions were the intensive care unit 57.2% (44 actions, 95% CI 46.25-68.24) and hospitalization for surgery 23.4% (28 actions, 95% CI 23.97-32.78), followed by surgery rooms 24.3% (22 actions, 95% CI 6.52-22.06), other services 5.2% (4 actions, 95% CI 0.26-20.23). Regarding the period of the day in which the report was made, the morning was the most frequent 37.7% (29 actions, 95% CI 26.89-48.43), afternoon 22.2% (27 actions, 95% CI 22.8632.30), night 22.2% (27 actions, 95% CI 22.86-32.30), weekends 24.3% (22 actions, 95% CI 6.52-22.06). In 3.9% (3 actions, 95% CI 0.0-8.20), the time at which the report was made was unknown.
Concerning the report by members of the health teams, it was found that professional nursing was the staff that most used the passive RS, 76.6% (59 actions, 95% CI 67.2286.03), followed by nursing and laboratory assistants 20.4% (8 actions, 95% CI 3.6-27.27), physicians 5.2% (4 actions, 95% CI 0.26-20.23), physiotherapists and students each reported 2.6% (2 actions, 95% CI 0.0-6.23), and speech therapists and nutritionists each reported 2.3% (2 action, 95% CI 2.22-3.82).
Operational performance of the passive reporting system
A total of 47 patients with unsafe actions were identified by the passive system, of this number, 23 patients had clinical incidents (PPV: 48.93%, 95% CI 34.6-66.2 for the identification of patients with clinical incidents), and 24 patients had at least 2 REUWE (PPV: 52%, 95% CI 36.8-65.4 for the identification of patients with REUWE) (Table 3).
Table 3 Positive predictive values for the identification of patients with clinical incidents and REUWE based on passive and active reporting systems.
| Reporting systems | ||||
|---|---|---|---|---|
| Passive (%) | 95% CI | Active (%) | 95% CI | |
| PPV to detect patients with clinical incidents | 23/47 (48.9) | 34.6-66.2 | 33/57 (57.89) | 45.1-70.7 |
| PPV to detect patients with REUWE | 24/47 (51) | 36.8-65.4 | 24/57 (42.1) | 29.3-54.9 |
CI = confidence interval, PPV = positive predictive value, REUWE = reportable events with unwanted effects.
Source: Authors.
Of the 24 patients who presented REUWE, 29 patients (79%) had only 2 REUWE, 4 patients (26.6%) had 2 REUWEs, and 2 patient (4.4%) presented 3 REUWEs.
The cumulative incidence of patients with clinical incidents in the surgery service, estimated from the passive RS, was 2.92% (23/2200; 95% CI 2.2-2.7), and the cumulative incidence of patients with REUWE was 2% (24/2200; 95% CI 2.2-2.8).
Operating performance of the active reporting system
The active RS using the Baker's tool13 identified 57 patients, with screening events (unsafe actions) equivalent to 28% of the analyzed sample, of which 32 were patients with clinical incidents (PPV: 57.89%, 95% CI 45.272.7 for the identification of patients with clinical incidents), and 25 were patients with REUWE (PPV 42.2%, 95% CI 29.3-54.9 for the identification of patients with REUWEs). The behavior of the 2 RSs (passive and active) in relation to the PPV for the identification of patients with clinical incidents and REUWE was similar (Table 3). The cumulative incidence of patients with clinical incidents in the surgery service, estimated from the active RS, was 1.91% and the cumulative incidence of REUWE reported from the active system (11.8%), the comparison of the estimated cumulative incidence values from both RSs is shown in Table 4.
Table 4 Cumulative incidence of patients with clinical incidents or REUWE from passive and active reports.
| Reporting systems | ||||
|---|---|---|---|---|
| Passive n 1200 | Active n 202 | |||
| n Patients (%) | 95% CI | n Patients (%) | 95% CI | |
| Patients with unsafe actions/screening events | 47 (3.91) | 2.8-5.0 | 57 (28.21) | 22-34.4 |
| Patients with clinical incidents | 23 (1.91) | 1.1-2.7 | 33 (16.33) | 11.2-21.4 |
| Patients with -REUWE | 24 (2) | 1.2-2.8 | 24 (11.88) | 7.4-16.3 |
CI = Cconfidence interval, REUWE = reportable events with unwanted effects.
Source: Authors, using data from study and the previously published study.2
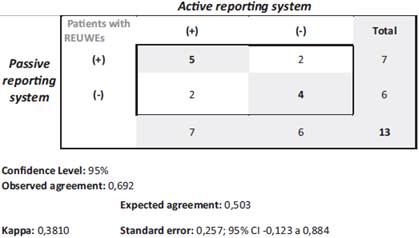
Concordance of the reporting systems (passive and active) in the identification of patients with REUWEs
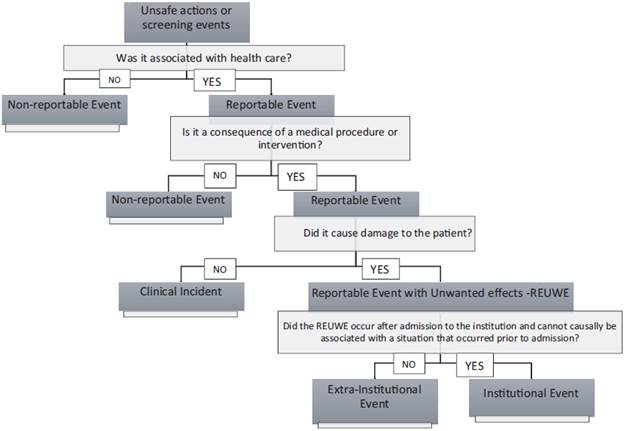
The agreement between the RSs for the detection of patients with REUWE resulted in 13 patients, coefficient of 0.3810 (Kappa) (95% CI -0.123-0.884) and standard error (SE) of 0.25. Details are presented in Fig. 2.
Source. Authors.
Figure 2 Concordance of the reporting systems (passive and active) in the identification of patients with REUWE. REUWE = reportable events with unwanted effects.
Thirteen patients coincided with at least 1 registry in both bases (detected by both RSs); however, only 2 patients (15.38%) were reported in both systems with the same REUWE (Fig. 3).
Discussion
The advancement of health systems and technologies worldwide and the inclusion of different actors in the health sector for the integral care of patients represent a complex scenario that can increase the risk of clinical incidents and REUWEs in hospitals.18 Hence, it is important to strengthen the institutional systems for reporting such events, as a trigger for the analysis and implementation of strategies to improve the quality of care.19
The present study reported the ability to detect true clinical incidents and REUWEs of 2 safety event RSs: the active and passive RSs. From the results, it is inferred that there are no differences in the PPVs of each system for the individual detection of the events mentioned (PPV patients with clinical incidents: passive 95% CI 34.6-66.2 vs active 95% CI 45.1-71.7; and PPV patients with REUWE: passive 95% CI 36.8-65.4 vs active 95% CI 29.3-54.9); however, the cumulative incidence of REUWE reported from the active system was higher than the incidence reported from the passive system, which is equivalent to a REUWE detection capacity of 83.5% more for the active RS.
These values are similar to those reported in the literature, where the REUWE detection capacity by the active RS exceeds the capacity of the passive RS by up to 95%.4 Although both incidence values found by the RSs analyzed are within the ranges reported in the literature (2.9%-16.6%),20 the great differences between the detection results in this study inally translate into an underestimation of the REUWEs in the passive system, with lower possibilities of analyzing the failures and learning them, for the prevention of new REUWE, since approximately 50% of REUWEs are preventable, which should be considered when preferring one over the other.
There are several causes that may explain underreporting in the passive RS. Burbano's study in 2013 reported that fear of being punished due the mistake is the main reason why professionals do not report, as well as lack of knowledge on what should be reported, fear of loss of credibility as a professional,21 in addition to the lack of time that is one of the most predominant justifications in health professionals.22
The kappa coefficient identified in this study to measure the concordance of active and passive RSs in the detection of patients with REUWE was acceptable (0.38), according to the Landis and Koch classification table, however, this value reflects the agreement of the subjects with REUWE, but does not reflect the coincidence between the REUWEs in each subject. The coincidence of patients and their REUWEs, which are reported by the 2 systems (active vs passive), is only 15.3%. Which means that, although both RSs have similar PPV for the detection of subjects with REUWE, the information on the events obtained from each RS is consistently different between them. These results allow exposing the variability of the systems against their ability to identify certain types of events and how the context of the analysis varies their performance capacity.
Regarding the services that have a greater culture of reporting unsafe actions, this investigation identified that the critical care unit is the service that exhibits the best behavior (reported 64.8% of all unsafe actions), followed by hospitalization in surgery (29.7%), which is consistent with what is reported in the literature.23 This may be due to the strict systems that characterize the critical care units, given the high complexity that they operate in patient care, which requires the adoption of elements of containment, improvement, and learning about clinical incidents and REUWE earlier.
An important finding in this study is that 71.4% of the unsafe actions that were reported through the passive system were made by nurses, which coincides with the nature of the main unsafe actions reported and the events involved: chemical phlebitis 16.5% and fixation lacerations 13.2%. This indirectly could reflect the asymmetry in the reporting culture in the institution.
Currently, the passive RS is most implemented in health systems, and the selection focuses on the advantages related to the cost and human resources needed in its application.24 However, in this work, it is notable that it requires adjustments or strategies that allow not only to improve its ability to identify REUWEs but also to reduce double records, which in this investigation accounted for 14% of the reports. The findings on the low coincidence of REUWE between the systems suggest that before preferring 1 system over another, they should be used in a complementary way, since the REUWEs detected by the active system are significantly different from those captured by the passive system.
The number of studies regarding the perception, knowledge, and commitment of the safety and report culture by the actors involved in the care of patients is increasing, although the scope of this research did not allow addressing these issues, the study results reflect that 7% of the reported events were non-reportable events, which could be related to a lack of familiarity regarding the process related to the identification and reporting of safety events, a fundamental link that determines the culture of security in an institution.25
The search for quality care has driven the implementation of various strategies focused on the prevention of risks for patients, ranging from the documentation of reportable events to the evaluation of strategies implemented for prevention,19 being the report of clinical incidents and REUWEs one of the tools for the improvement of safe patient care. The results of this work support this objective.
This study is one of the first approaches that establish the differences between passive and active RSs, based on the individual capacity to detect true clinical incidents and REUWE, as well as the concordance and coincidence between both RSs. The main strength of this study lies in the results on the direct comparison between both RSs. Regarding the application of the results of this work in the field of research, it is essential to consider the variability of the results when using different units of analysis (patients with REUWE vs REUWE) since individualizing the REUWE, although it represents difficulties to generate frequency estimators, it is necessary for an adequate characterization and to recognize timely opportunities for improvement in safety for patients.
The limitations are the number of patients with concordant REUEWE that generated imprecision of the Kappa coefficient results. The active search for events was only performed in a random sample of the total attention in the surgery service; this explains why it was only possible to calculate PPVs and no other operational characteristics such as sensitivity, specificity, and negative predictive values.
Conclusion
This work allows us to know the operational characteristics of passive RSs in relation to the active RS, in a teaching hospital in Bogotá, Colombia. The incidence of REUWE is substantially higher when the active system is used, so in the face of risk management activities where the learning of REUWE is necessary, it should certainly be considered. Since both systems provide different information regarding REUWE, it can be suggested that the best alternative is the combined use of the 2 strategies to strengthen their operational capabilities and have good notification management.
Although the 2 RSs demonstrated similar behavior toward their PPVs, the implementation of the 2 RSs with a complementary approach, which facilitates the timely detection of REUWE, would be appropriate to establish strategies that allow for better safety to patients during their hospital care. Similarly, the potentialization of the culture of reporting and the culture of safety at the institutional level is essential, which requires that all members of the health teams and other actors of the health sector be involved, to create solid networks with the same approach, non-punitive and fair safety culture.
Ethics approval and consent to participate
The study was approved by the ethics committee of the National University of Colombia through Act 36084-2016.
Consent for publication. Not applicable.
Availability of data and material. All data generated or analyzed during this study are included in this published article and a previously published article.











 text in
text in