Every year, around 300 million surgical procedures are performed worldwide 1,2, with an estimated 4% early postoperative mortality rate. 3,4 However, little is known about global quality of surgery, specifically in middle-income countries.
Colombia, similar to other Latin American countries, has an interesting diversity of healthcare needs. In urban settings, the healthcare offered is among the best in Latin America, with top-quality hospitals and educational programs comparable to those in the USA or Europe. In contrast, in most rural areas of Latin America, including some of the most remote locations in the world (like the Pacific Coast or the Amazon forest), a frail and fragmented healthcare system prevails, similar to the conditions in very low-income countries. At least 7.1 million people (15.1% of the population) lack hospital access within a 2-hour drive, and despite these characteristics, the early reported postoperative mortality is low - 0.74%. 5
This diversity represents a major challenge for an appropriate unbiased estimation of perioperative mortality. Additionally, it is important to understand how external factors at the macro level, including economic and administrative issues, social conditions, technological changes and health care inequalities, may influence clinical performance and quality of surgical care. 6
The Covid-19 pandemic has overwhelmed many health and social systems globally, resulting in a significant number of deaths, both directly and indirectly. One of the major concerns of surgical services is operating on patients during the COVID-19 pandemic. It is common knowledge that patients infected with SARS-CoV-2 perioperatively have a higher risk of 30-day mortality (23.8% (268 of 1128)) and a higher risk of postoperative pulmonary complications (51.2% (577 of1128)) than similar patients undergoing surgery before the pandemic 7. These findings should lead to a critical reflection about the urgency and safety of performing surgery in patients with current infection or a recent history of SARS-2-CoV infection. Moreover, middle-income countries have not been adequately represented in previous assessments of the perioperative risk for SARS-CoV-2
Conducting meaningful health research in Colombia, Latin America, and other middle-income countries typically involves significant challenges. Time limitations have been identified as a significant barrier to research engagement, as well as shortage of financial resources, lack of mentorship, and limited interest and incentives to generate high-quality knowledge. 8,9 Many of these limitations are reduced by contributing to well-organized global efforts to produce high-quality, adequately powered research in the perioperative setting.
The GlobalSurg Collaborative, coordinated through the NIHR Global Health Research Unit on Global Surgery, was recently created to address the need to improve mortality and outcomes after surgery in low- and middle-income countries (LMIC), through high quality collaborative research and training. To accomplish its goals, the GlobalSurg Collaborative conducts international surgical research, especially including low- and middle-income countries. Over the past 5 years, they have collected data from more than 40,000 patients to examine outcomes after emergency abdominal surgery, surgical site infection rates, and patient outcomes following breast, gastric and colon cancer surgery; currently GlobalSurg Collaborative has a number of ongoing randomized and epidemiologic studies. The emergence of the Covid-19 pandemic has had a major impact on health care delivery, and spurred the creation of CovidSurg Collaborative in partnership with GlobalSurg Collaborative, promoted by an international group of surgeons and anesthesiologists to measure the impact of SARS-Cov-2 on surgery and perioperative care worldwide.
Addressing surgical disparities requires both immediate relief efforts and long-term investments to improve access and outcomes. It also requires the unwavering participation of several stakeholders from a broad range of surgical and anesthesia specialties and settings (i.e., rural and urban areas).
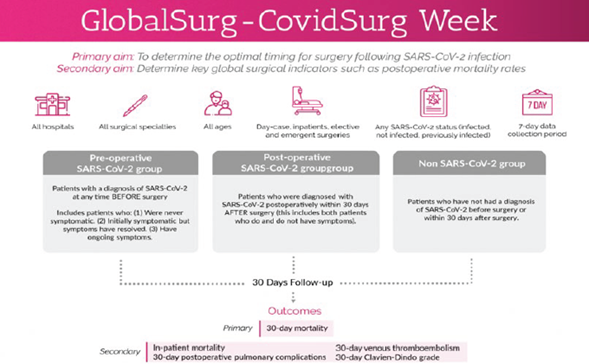
To tackle the urgent need for additional and globally representative COVID-related and non-COVID related perioperative mortality data, a new collaborative study has been suggested, under the name of the GlobalSurg-CovidSurg Week. This study collects perioperative outcomes data from all surgical patients during one specific week in October 2020. All hospitals, all surgical specialties, and patients of all ages and with any SARS-CoV-2 status are eligible to participate. The results of this study will help to define the optimal timing for surgical patients previously infected with SARS-CoV-2.
Following the findings from the CovidSurg study, Surg Week also intends to address one of the previous limitations, which was the lack of a contemporary non-SARS-CoV-2 infected comparator group, by having 3 groups of patients: patients with pre-operative Covid-19, people who never had Covid-19, and patients who developed SARS-CoV-2 infection postoperatively (Figure 1). The secondary aim of this study is to identify global surgery indicators, highly needed in Latin America.
Over 1,700 hospitals across 129 countries have now registered. Working together we will collect a large amount of data that can be generalized globally, to be able to accomplish the goals set forth in this study. This will probably be the largest international surgical study ever conducted, involving low and middle-income countries across the world.
Would you be interested in joining the study? Colombia and other Latin American countries are well positioned to make significant contributions to this study, and there are no limits to the number of hospitals and surgical subspecialties that can contribute. The commitment requires collecting data over 7 consecutive days in October 2020, from all consecutive patients undergoing surgery involving at least one surgical subspecialty.
The benefits from contributing to this effort are several. As a contributor, you and every contributing member of your data collection team, will be recognized as a co-author of the study. In addition, you will benefit from the camaraderie of a global productive research collaborative. The satisfaction derived from collaborating as equal partners, in order to contribute to globally relevant research, cannot be over-emphasized. This is one of the most effective and efficient ways to contribute to research that is relevant, both globally and locally.
Furthermore, a Colombia-wide research momentum paves the way for building together further research projects in the future. One added benefit is the opportunity to use country-specific data collected from Colombia for future publications. This data will also be relevant to global surgery indicator tracking and reporting.
We would be delighted to have every hospital, and every surgical sub-specialty involved, collecting data from all surgical patients.
If you are interested, please join us. We will certainly welcome the opportunity to assist you in taking your next steps for research ethics approval at your local institution.











 text in
text in