What do we know about this problem?
The number of surgical procedures is increasing worldwide. Colorectal surgery as treatment for colorectal diseases is associated with postoperative complications and prolonged hospital length of stay.
What is the contribution of this study?
This study provides clinical experts with better and more up-to-date evidence regarding multimodal enhanced recovery programs focused on critical outcomes in colorectal surgery.
INTRODUCTION
Over the past decade, there has been an increase of approximately 33% in the number of surgical procedures worldwide 1. At the same time, important advances have been made in colorectal surgery, although challenges still remain, mainly as refers to the high frequency of postoperative complications in up to 40% of patients, requiring prolonged hospital length of stay (LOS) 2 and resulting in up to a four-fold increase in care costs 3.
The multimodal perioperative care program, also known as enhanced recovery after surgery (ERAS), emerges as a health technology designed to reduce surgical stress and postoperative morbidity by means of standardization of preoperative, intraoperative and postoperative care components based on the best available evidence 4. Colorectal surgery is the setting in which greatest development and widespread use of the program has been achieved, mainly in high income countries 5-8, as evidenced by the large number of publications on the topic 4. However, there is still broad variability in clinical practice, and outcomes following colorectal surgery continue to be challenging, probably due to methodological limitations in the body of evidence which have not been examined to this date.
In this regard, there is a need to determine the true impact of the program on health outcomes, as well as the certainty of these results for decision-making on its potential implementation and allocation of resources for perioperative care. The objective of this research was to assess the certainty of evidence and the size of the effectiveness and safety of the multimodal perioperative program in elective colorectal surgery.
METHODS
A systematic literature review (SLR) was conducted in accordance with the protocol established and approved by the Ethics Committee of the Universidad Nacional of Colombia Medical School. The report of this review complies with the completeness recommendations contained in the PRISMA statement.
The search for evidence was conducted in the Medline (Ovid), Embase and Cochrane databases using the terms colorectal, colon, colonic, rectum, sigmoid, rectal, colorectal, fast-track, enhanced recovery surgery (ERAS), surgical, procedure, resection, laparoscopic. The search strategies are shown in Complemenatry content A. Also, the review looked into the references of the included studies through manual search, theses, research papers and abstracts. Searches were not limited by language or date of publication and included publications up until February 2020.
The following were the inclusion criteria: a) Reports of systematic reviews and/or meta-analyses of moderate confidence (non-compliance of up to one critical criterion, different from the search strategy and study selection, and from reporting of risk of bias assessment of primary studies included) according to the AMSTAR-2 tool; b) reports of randomized clinical trials (RCTs) and controlled clinical trials (CCT) or observational studies in case of not finding systematic literature reviews (SLRs); c) inclusion of adult populations (> 18 years) taken to elective colorectal surgery under a multimodal perioperative care program, compared to standard care. The program was defined as standardized perioperative management in colorectal surgery, including enhanced recovery programs (ERAS) or fast-track programs. Studies were excluded if the multimodal program did not include elements of the three phases of the perioperative period, if they had methodological limitations that compromised the confidence of the results, and if they did not report risk of bias of the primary studies included.
Primary outcomes were morbidity or complications, and postoperative mortality. Secondary outcomes were length of hospital stay (LOS) and readmission rate.
Two reviewers working independently selected the articles based on titles and abstracts; for articles with selection potential, full-texts were obtained and read, verifying eligibility criteria; disagreements were solved by consensus between the two reviewers. The methodological quality of the SLRs was reviewed by the same two researchers using A Measurement Tool to Assess Systematic Reviews (AMSTAR), version 2 9. Modifications to the categories of the tool were considered, as follows: moderate confidence, non-compliance with up to one critical criterion other than the search and study selection strategy and the risk of bias of primary studies included; low confidence, non-compliance with up to two critical criteria; and those that did not fall in these categories were considered to be of critically low confidence, while partial yes assessments were considered compliant. The high confidence category was maintained as defined by the tool. One of the reviewers used a specific form to enter the data of interest for moderate and high confidence SLRs, while another researcher verified the information.
The body of evidence was defined as the best quality and more updated SLR (maximum 5 years since publication until the search date) that answered the research question, in accordance with the proposal by Gaitan et al. 10. The GRADE method, through the application of GRADE pro, was used to assess the certainty of the results for the body of evidence 11.
Statistical analysis and information synthesis
A narrative synthesis of the findings in the included studies was made. Frequency and association measures were reported, including relative risk (RR), odds ratio (OR), hazard ratio (HR) and mean differences (MD), with 95% confidence intervals, when available in the papers included.
This article is the result of an original research carried out as a prerequisite to obtain a Master's degree in Clinical Epidemiology from the Universidad Nacional of Colombia. It was approved by the Ethics and Research Committee of the Universidad Nacional of Colombia of Medicine School. It is considered a risk-free research, as it is a synthesis of retrospective published information with no changes in the variables of actual individuals. No animal or human experiments were conducted.
RESULTS
Overall, 863 references were retrieved by the search. Of these, 33 were considered potentially eligible and the rest were excluded due to the reasons described in Figure 1. The full texts for the 33 were assessed and, in the end, 6 SLRs were included 12-17. Exclusions are detailed in Complementary content B.
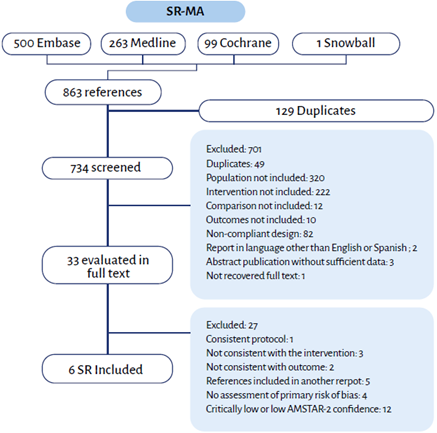
ERAS: Enhanced recovery after surgery, RCT: Randomized clinical trial. SOURCE: Authors.
FIGURE 1 PRISMA search, study selection and inclusion.
Description of included studies
The characteristics of the included studies are shown in Table 1. The six SLRs included six RCT-type primary studies, one included both RCTs and CCTs 13 and one included RCTs and observational studies 16. For the literature search, four databases were queried on average. The median number of studies in each SLR was 14.5. Of the six included studies, five metaanalysis synthesized the information. One reference analyzed patients with cancer and benign condition as well as the surgical approach 13, a second one focused on the laparoscopic approach and a third one focused on adults 65 years or older 16. Five SLRs used the Cochrane risk of bias assessment tool and the Downs and Black IQ Index to assess the quality of the included studies 16. Regarding SRL methodological quality, two were rated as high confidence 14,16 and the others were classified as moderate confidence in accordance with the modified AMSTAR-2.
TABLE 1 Characteristics of the included systematic literature reviews.
| Author | Search date | Queried databases | Design | Number of studies included | ERAS/ Traditional care | Meta-analysis | Risk of bias tool | AMSTAR-2 | |
|---|---|---|---|---|---|---|---|---|---|
| Bagnall, 2014 16 | January 1947 -February 2014 | Medline | RTC | 2 | 234 | No | Quality Index | HIGH | |
| EMBASE | Observational | 11 | 35 | ||||||
| CENTRAL | 3 | ||||||||
| Greco, 2013 12 | Up to June2012 |
BioMedCentral PubMed Scopus CENTRAL |
RTC | 16 | 1181/1195 | Yes | Cochrane tool | MODERATE | |
| Greer, 2018 13 | 2011 - July2017 |
Medline (Ovid) CINAHL |
RTC | 22 | 2207/ | Yes | Modified Cochrane tool | MODERATE | |
| CINAHL | RTC | 3 | 2043 | ||||||
| Ni, 2019 17 | Up toOctober2019 |
PubMed EMBASE Cochrane Library Web of Science ClinicalTrials.gov |
RTC | 13 | 639/ 659 | Yes | Modified Cochrane tool | MODERATE | |
| Spanjersberg, 2011 14 | Up to 2009 |
CDSR DARE CENTRAL NHS Economic Evaluation Database |
EMBASE ISI Web of Knowledge (Web of Science) ASCRS MEDLINE |
RTC | 6 | 119/118 | Yes | Cochrane tool | HIGH |
| Zhuang, 2013 15 | January 1966 - July 2012 |
Pubmed EMBASE CENTRAL |
RTC | 13 | 953/957 | Yes | Cochrane tool | MODERATE | |
ERAS: Enhanced recovery after surgery, RCT: Randomized clinical trial. SOURCE: Authors.
The definition of the multimodal perioperative program in colorectal surgery was found to vary in terms of the items contained, with a range between four and eighteen items. The items found in the six SLRs were: preadmission education, preanesthetic medication avoidance, mechanical bowel preparation and preoperative fasting, use of carbohydrate loading, hypothermia prevention, minimally invasive surgical approach, and early drain removal. The items gathered for each SLR are shown in Table 2. Morbidity or postoperative complications, LOS, readmission rates and mortality were outcomes of interest in all SLRs. Other outcomes included ileus, surgical site infection, time to first flatus, ambulation and oral intake initiation.
TABLE 2 Elements of the ERAS (enhanced recovery after surgery) program.
| Program elements | Bagnall (16) | Greco (12) | Greer (13) | Ni (17) | Spanjersberg (14) | Zhuang (15) |
|---|---|---|---|---|---|---|
| Counseling, education and information prior to admission | x | x | x | x | x | x |
| Nausea and vomiting prevention | x | x | x | x | x | |
| Preanesthetic medication avoidance | x | x | x | x | x | x |
| Antimicrobial prophylaxis and skin preparation | x | x | x | x | ||
| Bowel preparation avoidance | x | x | x | x | x | x |
| Preoperative fluid and electrolyte therapy | x | x | x | x | ||
| Antithrombotic prophylaxis | x | x | x | x | x | |
| Symbiotics | x | |||||
| Preoperative fasting and carbohydrate loading | x | x | x | x | x | x |
| Standard anesthesia protocol | x | x | x | x | x | |
| Intraoperative fluid and electrolyte therapy | x | x | x | |||
| Hypothermia prevention | x | x | x | x | x | x |
| Minimally invasive surgical approach | x | x | x | x | x | x |
| Thoracic epidural | x | x | x | |||
| High O2 concentrations | x | |||||
| Nasogastric tube removal | x | x | x | x | x | |
| Non-opioid postoperative analgesia | x | x | x | x | x | |
| Postoperative fluid and electrolyte therapy | x | x | ||||
| Early urinary catheter removal | x | x | x | x | x | x |
| Postoperative blood glucose monitoring | x | x | ||||
| Postoperative nutritional care | x | x | ||||
| Early mobilization | x | x | x | x | x | |
| Early food intake | x | x | x | x | x | |
| Prokinetics, ileus prevention | x | x | x | x | ||
| No drains | x | x | x | x | x | |
| Audit | x |
SOURCE: Authors.
Table 3 shows the results of the outcomes assessed in each of the SLRs included.
TABLE 3 Primary results of the included systematic literature reviews.
| Outcome | Bagnall (16) | Greco (12) | Greer (13) | Ni (17) | Spanjersberg (14) | Zhuang (15) |
|---|---|---|---|---|---|---|
| POP complication | ERAS: 5 % vs. no-ERAS: 21 % (p = 0.045) | RR: 0.60 (IC 95 % [0.46-0.76]) | RR: 0.66 (IC 95 % [0.54-0.80]) | RR: 0.59 (IC 95 % [0.40-0.86]) | RR: 0.52 (IC 95 % [0.38-0.71]) | RR: 0.71 (IC 95 % [0.58-0.86]) |
| ERAS: 27 % vs. no-ERAS: 59 % (p < 0.0001) | ||||||
| POP mortality | No deaths reported | RR: 1.19 (IC 95 % [0.52-2.71]) | OR peto: 1.79 (IC 95 % [0.81-3.95]) | RR de 0.89 (IC 95 % [0.34-2.38]) | RR: 0.53 (IC 95 % [0.12-2.38]) | RR: 1.02 (IC 95 % [0.40-2.57]) |
| Hospital length of stay (days) | Between -2 and -4 (p < 0.05) | WMD -2.28 días (IC 95 % [-3.09 a -1.47]) | MD: -2.62 (IC 95 % [-3.22 a -2.02]) | WMD: -2.00 (IC 95 % [-2.52 a -1.48]) | MD: -2.94 (IC 95 % [-3.69 a -2.19]) | Primary LOS DMP: -2.44 (IC 95 % [-3.06 a -1.83]) |
| Total LOS DMP: -2.39 (IC 95 % [-3.70 a -1.09]) | ||||||
| 30-day readmission rate | Not reported | RR: 0.78 (IC 95 % [0.50-1.20]) | RR: 1.10 (IC 95 % [0.81-1.50]) | RR: 0.65 (IC 95 % [0.35-1.20]) | RR: 0.87 (IC 95 % [0.08-9.39]) | RR: 0.93 (IC 95 % [0.56-1.54]) |
CI: confidence interval, ERAS: enhanced recovery after surgery, MD: Mean difference, LOS: length of stay, OR: Odds Ratio, p: p value, POP: Postoperative, RR: Relative Risk, WMD: Weighted mean difference. SOURCE: Authors.
Complications and/or morbidity
The study by Bagnall et al., which gathered information on elderly patients, found a range of complications between 5% and 27% in the ERAS groups, as compared to a range of 21 to 59% in the groups receiving standard care (p < 0.05) 16. A similar direction of the effect in favor of the ERAS group was found in the studies by Greco et al., Greer et al., Spanjersberg et al. and Zhuang et al., reporting a reduction in the risk of postoperative (POP) complications between 39% and 48% 12-15.
In terms of the complexity of the complications, Spanjersberg et al. did not find differences in major and minor complications between the groups (p = 0.34). In contrast, there was a difference in overall complications in favor of the ERAS program, with 58% risk reduction (p = 0.003) 14. Greco made a distinction between surgical complications (bleeding, need for reoperation and others) and non-surgical complications (Foley catheter reinsertion or complication and aspiration/ infection pneumonia) as safety outcomes. There were no differences between the groups in terms of surgical complications, while the risk of non-surgical complications was lower with ERAS (RR: 0.40, 95% CI 95 [0.27-0.61]) 12; a similar finding was reported by Zhuang et al. for surgical complications 15.
According to Bagnall, respiratory complications were less frequent in the ERAS group, 5.1% vs. 16.4% (p < 0.0001) 16; like Greco, they found that ERAS was protective against these types of complications (RR: 0.41, 95% CI [0.220.76]) and also against cardiovascular complications (RR: 0.51, 95% CI [0.290.89]); no differences were found in terms of urinary tract complications (RR: 0.39, 95% CI [0.11-1.37]), although Bagnall et al. described higher urinary tract infection in elderly patients in the standard care group 4.3% vs. 11.2% (p = 0.047). There were no differences in anastomotic leak, surgical site infection or ileus (p = 0.86, p = 0.14 and p = 0.53, respectively) 12.
Ni et al. found that ERAS reduced POP complications by 41% in patients undergoing laparoscopic colorectal surgery (RR: 0.59, 95% CI [0.40 to 0.86]) 17, a finding that was also reported by Greer et al. in their subgroup analysis by surgical approach, with a 41% reduction in laparoscopic surgery (RR: 0.59, 95% CI [0.39-0.90]), and risk reduction of 37% (RR: 0.63, 95% CI [0.49-0.83]) in open surgery. In patients with colorectal cancer who received ERAS, the risk of postoperative morbidity dropped by 39% (RR: 0.61, 95% CI [0.46-0.80]), while this reduction was 52% in patients with rectal cancer (RR: 0.48, 95% CI [0.27-0.88]) and 55% in patients with benign conditions (RR: 0.45, 95% CI [0.25-0.81]) 13.
Certainty in the findings for the postoperative complications outcome was very low and, consequently, it is subject to change in the light of new evidence, according to the GRADE methodology used to assess certainty of the body of evidence corresponding to the SLR conducted by Greer et al.
Readmission rate and mortality
All the studies consistently reported absence of differences in these outcomes when the multimodal perioperative program was compared with traditional care (13,15,17). Although, in their studies, Greco and Spanjersberg conducted sensitivity analyses using data from low/ moderate risk of bias studies, the results did not show any differences either (RR: 0.53, 95% CI [0.09-3.15]) 14. Certainty of the findings for postoperative mortality and readmission outcomes was very low and, therefore, subject to change in the light of new evidence.
Length of hospital stay
The six SLRs reported shorter LOS in favor of the multimodal care program. Bagnall found reductions ranging between 2.5 and 4 days 16. Zhuang made a distinction between primary and total LOS, the latter defined as primary plus LOS after readmission within the first 30 days of the surgery and, in both cases, described differences in favor of the program (p < 0.00001), with an average reduction of 2.44 days (95% CI [-3.06 to -1.83]) in primary LOS and 2.39 days [-3,70 to -1,09]) in total LOS 15. Greer, Greco and Spanjsberg reported similar findings 12-14.
In a meta-analysis of 24 studies, Greer et al. found a mean difference of 2.62 days in LOS reduction (MD: -2.62, 95% CI [-3.22 to -2.02]) when ERAS was compared with traditional care. Depending on the surgical approach, they reported that in patients who underwent open surgery, the reduction was 2.55 days (95% CI [-3.43 to -1.67]), while for laparoscopic surgery, the reduction was 2.76 days (95% CI [-3.58 to -1.93]).
Moreover, the reduction for patients with colorectal cancer was 2.88 days (95% CI [-4.03 to -1.73]), 2.25 days (95% CI [-3.69 to -0.81]) for patients with rectal cancer, and it was highest in benign conditions, at 3.16 days (95% CI [-3.97 to -2.34]) 13.
The certainty of the findings for the LOS outcome was very low and, therefore, subject to change in the light of new evidence.
Other outcomes described
Bagnall et al. reviewed time to ambulation and found it to be shorter in the ERAS group (p < 0.001) for patients >65 years. Moreover, one of the included studies reported differences in favor of ERAS in terms of less cases of pulmonary and urinary tract infections, postoperative heart failure and delirium 16. Greer et al., on the other hand, found assessment of postoperative pain in only two studies and quality-of-life assessment in a single study, with no clinically significant changes 13.
Findings relating to gastrointestinal function showed differences in favor of the multimodal program. Greer et al. classified these outcomes as moderate, describing that, of the 22 studies in which return of intestinal function was assessed, 21 found differences, and of 14 which assessed time to resuming a solid diet, 13 found differences 13. Bagnall et al. and Zhuang et al. reported a shorter time interval to the first flatus (MD -1.02 days, 95% CI [-1.36 to -0.67]) and to bowel movement (-1.12 days, 95% CI [-1.37 to -0.87]); and also described positive results in the ERAS group for early fluid tolerance (p < 0.001) 15,16. Additionally, Spanjersberg et al. reported that patients receiving ERAS compared to standard care, tolerate initiation of oral intake 42 hours earlier (p = 0.042), solid diet three days earlier, with return of bowel activity two days earlier (p < 0.001) than patients receiving standard care 14.
In terms of adherence to the program, the study by Bagnall et al. was the only that looked specifically at the elderly. They observed that in patients over 64 there was less compliance with early initiation of fluids, solid diet and early catheter removal when compared to younger patients (p < 0.0001). In patients 75 and older, adherence to laparoscopic surgery was lower, while adherence to the use of abdominal drains was higher, when compared to patients between 64 and 74 years of age (p < 0.002). In patients over 79 years of age, adherence to bowel preparation, use of antiemetics and epidural analgesia was higher compared to the 70-79 age group, in which adherence to fluid restriction and early ambulation was higher 16.
Finally, the SLR conducted by Greer et al. was selected as the body of evidence because it was shown to be the most updated, it was given a moderate rating of confidence on the modified AMSTAR-2, and contained the primary studies which were included in the other SLRs reviewed 13. The results of the certainty evaluation using the GRADE methodology indicated that evidence certainty is very low, based on the fact that the primary studies included in the SLR showed a high or unclear risk of bias and high heterogeneity and nonevaluation of the publication risk by the authors of the SLR. The details of the results are shown in Table 4.
TABLE 4 Certainty of evidence.
| Study design (n) | Risk of bias | Inconsistency | Indirect evidence | Inaccuracy | Other considerations | N.° of participants in each arm (ERAS/no ERAS) | Effect | Certainty | |
|---|---|---|---|---|---|---|---|---|---|
| Relative (95% CI) | Absolute (95% CI) | ||||||||
| Hospital length of stay (mean difference assessment) | |||||||||
| Randomized trials (24) | Very seriousa | Very serious b.c | Not serious | Not serious | Strong suspicion of publication bias | 1.838/1.949 | - | MD 2.62 days less | ©OOO |
| Very strong associationd | [3.22 less to 2.02 less] | VERY LOW | |||||||
| Overall postoperative morbidity (Relative Risk assessment) | |||||||||
| Randomized trials (19) | Very seriousa | Seriouse | Not serious | Not serious | Strong suspicion of publication biasd | 1.464/1.465 | RR 0.66 | 99 less for every 1.000 | ©OOO |
| [0.54 a 0.80] | [From 134 lessto 58 less] | VERY LOW | |||||||
| Postoperative mortality (Follow-up: median of 30 days; assessed with Odds Ratio-Peto) | |||||||||
| Randomized Trial (22) | Very seriousa | Not seriousf.g | Not serious | Serioush | Strong suspicion of publication biasd | 1.619/1636 | OR 1.79 | 4 more for every 1.000 | ©OOO |
| [0.81-3.95] | [From 1 less to 16 more] | VERY LOW | |||||||
| Postoperative readmision (Follow-up: median of 30 days; assessed with Relative Risk) | |||||||||
| Randomized trials (19) | Very seriousa | Not seriousf.g | Not serious | Serioush | Strong suspicion of publication biasd | 1.196/1.313 | RR 1.10 | 6 more for every 1.000 | ©OOO |
| [0.81-1.50] | (From 12 less to 32 more ) | VERY LOW | |||||||
CI: Confidence interval, ERAS: Enhanced recovery after surgery, MD: Mean difference, OR: Odds ratio, RR: Relative risk, SMD: Standardized mean difference.
a. Reports that the majority of the studies were shown to have a high and unclear risk of bias. b. Statistically substantial heterogeneity is reported (I2 > 70%), unexplained in exploratory analyses on the basis of study design or length of stay in the control group. Despite high protocol variability between the two groups, the sensitivity analysis did not show changes in the combined effect. c. No CI overlap. d. Dos not report publication bias assessment. e. Important heterogeneity: I2 > 40% < 70%. f. CI overlap g. Low heterogeneity: I2 < 40. h. Narrow, non significant CI.
SOURCE: Authors.
DISCUSSION
Surgical care is a critical component of medical care and contributes to social and economic development in general 4. Colorectal surgery is the treatment option that offers the highest probability of cure for colorectal disease, and perioperative care is an imperative challenge, given the increasing occurrence of this disease and the growing number of chronic diseases, such as cancer, in an aging population 1.
Postoperative complications are significantly frequent among patients undergoing colorectal surgery, affecting quality of life of both patients and families. Moreover, complications result in a substantial increase in healthcare-related costs due to longer hospital stay and the need for additional procedures and care 3. This research was prompted by these issues and, having found a large number of secondary studies on the effectiveness and safety of the program of interest, it is considered to provide the most up-to-date evidence on the effectiveness and safety of multimodal perioperative care programs in colorectal surgery.
Although the amount of information retrieved reaffirms the concern regarding the course of the perioperative period, the evident methodological limitations of the studies may fuel the controversy or foster resistance to implementation. Moreover, it is important to underline the redundancy of SLRs that process information derived from the same primary studies, as had been reported in the review by Chambers et al. 18. The SLRs included in this review suggest that the implementation of the multimodal perioperative care program in colorectal surgery is effective at reducing overall postoperative mortality and hospital length of stay, but it does not offer conclusive results in terms of mortality and readmission rates. However, the certainty of the results is very low according to the GRADE methodology, which means that new research could result in changes in the estimated effect.
No significant results in favor of the program were reported for mortality or readmission rates, which might be explained by the low frequency of occurrence of these events and by the limited size of the primary studies included in the SLRs. It is also important to consider that short follow-up periods, restricted only to the period between hospital discharge and readmission, prevent any determination of strong long-term outcomes.
Because of the nature of the program, some of its components may have been implemented in control groups, defined as standard or traditional care in the primary studies. The components of the standard care were not spelled out clearly enough in the included reviews so as to allow the identification of differences between the intervention and the comparator. Although the bias that this could introduce against the program is recognized, results in terms of complications and LOS still favor the intervention.
Three limitations are recognized: first of all, the review protocol was not registered, considering that the review was conducted within the framework of a health technology assessment. However, it is worth explaining that the health technology assessment had a protocol which included the systematic review and was approved by the Ethics Committee of the Universidad Nacional of Colombia Medical School; second, no subgroup analyses were reported in accordance with a combination of program items and their relationship with outcomes so as to lead to program optimization and targeting towards specific outcomes associated with the particular needs of the institutions; third, issues associated with the most recent version of AMSTAR when applied to SLRs conducted before the update, as has been recognized by the developers of the tool 9. In this research, of the 33 SLRs found, 12 had to be excluded based on their quality assessment using AMSTAR-2, even though the research group introduced a modification in the rating, allowing the use of items categorized as partial which, in the tool, are considered as non-compliant; otherwise, only one SLR could have been considered. It is important to highlight that the modification to the rating tried to maintain high quality and was stringent in the assessment of the items related to risk of bias as well as search criteria.
An important consideration that calls researchers and clinicians to reflection is the relevance of patient-reported outcomes. Although our search focused on LOS, POP complications and mortality, none of the reviews included described quality-of-life or patient-reported outcomes, which are considered relevant for all decisions that involve them and their families, as reaffirmed by Street 19. It is expected that those outcomes will be considered in future research.
In conclusion, despite differential findings in favor of the multimodal perioperative program in colorectal surgery in terms of reduced POP complications and LOS reported in SLRs, the certainty of these findings is very low and, therefore, subject to change in the light of new evidence. Consequently, there is no certain evidence at the present time to recommend the implementation of this program in elective colorectal surgery. New research with good methodological quality and that includes patient-reported outcomes is required in order to provide a clear understanding of the benefits of the program.
ETHICAL RESPONSIBILITIES
Ethics committee approval
This research was approved on February 8, 2019, by the Ethics Committee of the Universidad Nacional of Colombia Medical School (Minutes No. N° 002-014-19).
Human and animal protection
The authors declare that no human or animal experiments were carried out as part of this research.
ACKNOWLEDGEMENTS
Authors' contributions
All the authors participated in the design and conduction of the systematic review within the framework of a Master's thesis in Clinical Epidemiology. KC, EC, OG and JD worked on the idea and design of the study. KC and LR conducted the search and collected the data. KC, EC, OG, JD, LR interpreted the results and worked on the final drafting of the manuscript.











 text in
text in 



