What do we know about this problem?
Patient reported outcomes (PRO) are effectively measured using questionnaires, apps or over the phone interviews, and measure the quality of life and the overall perception about the health status.
Multiple trials have shown the adoption of PRO following cephalic duodenopancreatectomy (DPC), with controversial reports in terms of quality of life and going back to normal everyday life activities.
What does this new trial contribute?
Study in Latin population adopting PRO following DPC, using the EQ-5D-5L questionnaire, compared against a control group.
The overall health perception following DPC is slightly lower than in patients undergoing laparoscopic cholecystectomy.
The differences in quality of life perception are based on: increased pain, presence of anxiety/depression and disruption of activities of daily life.
INTRODUCTION
Cephalic duodenopancreatectomy (DPC or Whipple procedure) has undergone several technical transformations since it was originally described over one century ago. This procedure us indicated for pancreatic neoplasms, and less often for chronic pancreatitis or cystic lesions. 1 The initial mortality was of around 30 % and there are current reports of up to 4 % in high volume institutions; however, the mortality ranges between 30 and 60 %. 2 The most frequent postoperative complications are delayed gastric emptying, pancreatic fistula and surgical wound infection, which reflects in the rate of readmissions, reinterventions and longer hospital stay. These aspects impact the patient's quality of life, which is extremely important but seldom assessed. 3
Historically, in 1948, the world Health Organization (WHO) defined health as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity". 4 Later, this definition was accompanied by the term quality of life, which evolved from a conceptual definition to a series of scales and questionnaires used to measure the overall perception of the individual, in terms of functionality, pain, disability, and mental state. 5,6 Moreover, the ongoing technological evolution and target therapies of cancer patients - including pancreatic cancer - have been able to improve their survival and long term results. However, these pathologies are accompanied by distressing symptoms that negatively affect functionality and quality of life, even long after the initiation of treatment, with an impact not just on the patient, but on the family and the people around them. 7
Patient reported outcomes (PRO), in terms of medical therapy-associated quality of life, may be considered a compensation measurement between the benefit of surviving, the toxicity of the treatment, and the physical and emotional wellbeing of patients. 8 Currently there are a number of generic, multidimensional instruments and designed for all types of cancer, an even for chronic pathologies.
There are several studies - with controversial reports - in terms of quality of life after DPC due to adenocarcinoma or chronic pancreatitis with discretely lower scores in the quality of life indicators as compared against patients undergoing laparoscopic cholecystectomy. 9 However, another prospective trial in patients with pancreatic resection (68 % due to pancreatic adenocarcinoma) showed that the quality of life decreases during the three postoperative weeks, but then return to the preoperative baseline levels and is maintained for up to six months- 10 Moreover, Ruckert et al., in a retrospective trial with 67 patients undergoing DPC due to chronic pancreatitis, quality of life was evaluated using a measurement instrument comparing against healthy volunteers and found that most patients obtained similar results and were able to satisfactorily return to their activities of daily living. 11
With this background, the purpose of this trial was to compare the groups of patients to whom the same instrument was administered to measure quality of life: one group of patients with DPC and a control group undergoing laparoscopic cholecystectomy in the same hospital. The instrument used was the EQ-5D-5L questionnaire 12-14, validated for Colombia and designed by EuroQol Group. The underlying hypothesis was that patients undergoing DPC could have the same perceptions in terms of quality of life, as those undergoing laparoscopic cholecystectomy.
MATERIALS AND METHODS
A retrospective cohort trial was conducted, reviewing all patients who underwent DPC by the hepatobiliary surgical team (HPB), between July 2018 and February 2020, and the management of the condition in an institution in Medellín (Colombia). All the procedures analyzed were performed by the same surgical team made up by two surgeons and two anesthesiologists, specialized in HPB. The selection criteria were defined as follows: 1) Inclusion criteria: patients programmed for DPC, regardless of the type of pathology (benign, malignant) and age over 18 years old; and 2) exclusion criteria: carcinomatosis or vascular infiltration that required cancelling the surgery. The quality of life data collection was conducted during April 2020 and a minimum follow-up of 2 months was required. All variables, except exposure to the quality of life questionnaire, were accurately collected from each patient's electronic medical record, and the reviewers never reassessed the diagnoses or any other information already recorded in the medical charts. The groups were defined as patients undergoing DPC and the control group was patients undergoing laparoscopic cholecystectomy secondary to gallbladder lithiasis, matched by gender, age and date of the intervention. Secondary source data were assessed, such as the demographic characteristics, diagnosis, length of hospital stay, and 60-day mortality.
In order to measure the quality of life reports by patients, an authorization was requested from the EuroQol research foundation (EuroQol Office, Marten Meesweg 107, 3068 AV Rotterdam, The Netherlands) in order to administer the EQ-5D-5L questionnaire. An approved version of the questionnaire translated into Spanish was approved by expert consultants specialized to produce a language adaptation prepared and approved for Colombia since 2012 (registry number 34496). 13,14
This health questionnaire was administered over the telephone to all patients by one of the investigators, other than the patient's treating physician, to avoid interviewer bias. The questionnaire is made up of five questions or quantitative dimensions and are related to quality of life, at the time of administering the questionnaire. These dimensions are: 1) Mobility, 2) Personal Care, 3) Activities of Daily Life, 4) Pain/Discomfort and 5) Anxiety/depression. Each dimension includes 5 possible answers and the patient may only select one answer per dimension to describe his/her best health status (for instance, Mobility: 1: I do not have a problem to walk, 2: I have mild problems to walk, 3: I ha e moderate problems to walk, 4: I have severe problems to walk 5: I am unable to walk). The last question is a numeric quantitative scale reflecting the overall health status scored from 0 to 100, where 0 represents the worst imaginable health and 100 the best imaginable health; every patient is required to give his/her numeric answer.
For the sake of completeness of this article, the STROBE guide for cohort trials was used. The data collection and analysis were approved by the Ethics Committee of Clínica CES, on March 10, 2020 and in accordance with the legal provisions that govern the scientific, technical and administrative standards for health research, under Resolution 8430 of 1993, whereby this research project is considered risk-free. The verbal informed consents were obtained over the telephone, prior to administering the quality of life questionnaire.
The analysis took into account the characteristics of the variables and used the SPSS software version 20.0 to process the information. In terms of the quantitative variables, the corresponding central tendency and dispersion measurements were used, in accordance with their distribution, using the Kolmogorov-Smirnov test, expressed as medians and interquartile range (IQR). With regards to the qualitative variables, the description was made in terms of absolute and relative frequencies; a bivariate exploratory analysis is presented. The quality of life variable was dichotomized due to the patient's failure to select an answer in some of the dimensions evaluated. Hence, the score for the first 44 dimensions of the EQ-5D-5L questionnaire was classified as: 1) I do not have any problems or I have mild problems, and 2) I have moderate, severe, or serious problems, resulting in a dichotomic variable for these dimensions. These variables were analyzed via a comparison of proportions, with the independence Pearson's statistical Chi squared, using the lowest risk variable as a reference value (I do not have any problems or I have mild problems), the raw odds ratios (OR) are calculated with the corresponding 95% confidence intervals (95 % CI) using 2x2 tables. For the better health variable score, the bivariate analysis was conducted using the Mann-Whitney U test. An alpha value of less than 0.05 was considered statistically significant.
RESULTS
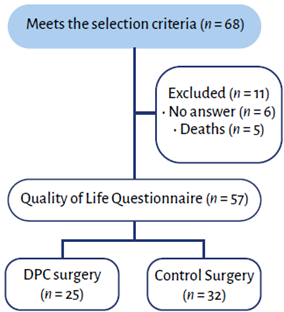
Sixty-eight patients met the inclusion criteria from July 2018 through February 2020, 6 of which failed to answer the telephone call y 5 passed away. The EQ-5D-5L questionnaire was administered to 57 patients (Figure 1). Of the 5 patients who died, only 1 was classified as death in less than 60 days; the rest were all beyond 60 days.
In the terms of the demographic and clinical characteristics of the 68 patients in the initial cohort, 30 (44.1 %) underwent DPC surgery and 38 (55.8 %), underwent laparoscopic cholecystectomy; they were matched by age gender, and date of the procedure, with a 1:1 an approximate ratio (0.78). 63.2 % of the total cohort of patients were females, with a mean age of 60 years. The most frequent diagnosis in the DPC group was pancreatic cancer (30 %), followed by papillary adenocarcinoma (26,7 %); while in the cholecystectomy group, the most frequent diagnosis was lithiasis (100 %). The hospital stay for the DPC group was 7 days (IQR 5-11) and in the cholecystectomy group was 1 day (IQR 0-1). The 60-day mortality was 3.3 % (n = 1) for the DPC group, and 0 for the control group (Table 1).
TABLE 1 Demographic and clinical characteristics (n = 68).
| DPC (n = 30) | Laparoscopic cholecystectomy (n = 38) | |||
|---|---|---|---|---|
| Characteristics | n | % | n | % |
| Female | 15 | 51.7 | 26 | 71.8 |
| Age* | 59 | 50-60 | 60 | 48-68 |
| Diagnosis | ||||
| Lithiasis | 0 | 0 | 38 | 100 |
| Pancreatic cancer | 9 | 30.0 | 0 | 0 |
| Papillary adenocarcinoma | 8 | 26.7 | 0 | 0 |
| Duodenal tumor | 2 | 6.7 | 0 | 0 |
| Distal cholangiocarcinoma | 2 | 6.7 | 0 | 0 |
| IPMN | 2 | 6.7 | 0 | 0 |
| NET. head of the pancreas | 2 | 6.7 | 0 | 0 |
| Chronic pancreatitis | 3.3 | 0 | 0 | |
| Chronic pancreatitis + IPMN | 3.3 | 0 | 0 | |
| Locally advanced adenocarcinoma | 3.3 | 0 | 0 | |
| Retroperitoneal tumor | 3.3 | 0 | 0 | |
| Solid pancreatic pseudopapillary tumor | 3.3 | 0 | 0 | |
| Length of stay * | 7 | 5-11 | 1 | 0-1 |
| 60-day mortality | 1 | 3.3 | 0 | 0 |
*Median (IQR), DPC: Cephalic duodenopancreatectomy; IPMN: Intraductal papillary mucinous
The PRO evaluation based on the EQ-5D-5L questionnaire showed the prevalence of the first two answer options, which qualitatively are a higher score (Table 2). The re-categorized questionnaire is presented in a dichotomous fashion based on the patient's answer - in accordance to the description under Materials and Methods -as: 1) I do not have any problems or I have mild problems, and 2) I have moderate, severe or serious problems. The results for mobility were OR: 0.41, 95 % CI [0,30-0,57], p = 0.103) and for personal care, OR: 0.42, 95 % CI [0.32-0.58], p = 0.254; most patients in both the DPC and cholecystectomy groups said "I do not have any problems or I have mild problems", and these measurements do not show any significant differences. With regards to measurements about daily life activities, the results were: OR: 0.38, 95 % CI [0.27-0.54], p = 0.017; pain/discomfort: OR: 2.33, 95 % CI [0.99-5.48], p = 0.013; and for anxiety/depression, the OR: 0.39, 95 % CI [0.28-055], p = 0.019, evidencing differences between DPC surgery and the control group (Table 3).
TABLE 2 Quality of Life Questionnaire EQ-5D-5L (n = 57).
| Questionnaire EQ-5D-5L | DPC (n = 25) | Laparoscopic Cholecystectomy (n=32) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Mobility | ||||
| I have no problems to walk | 19 | 76 | 32 | 100 |
| I have mild problems to walk | 4 | 16 | 0 | 0 |
| I have moderate problems to walk | 1 | 4 | 0 | 0 |
| I have severe problems to walk | 1 | 4 | 0 | 0 |
| I am unable to walk | 0 | 0 | 0 | 0 |
| Personal care | ||||
| I have no problem to shower or get dressed | 20 | 80 | 32 | 100 |
| I have mild problems to shower or get dressed | 4 | 16 | 0 | 0 |
| I have moderate problems to shower or get dressed | 1 | 4 | 0 | 0 |
| I have severe problems to shower or get dressed | 0 | 0 | 0 | 0 |
| I am unable to shower or get dressed | 0 | 0 | 0 | 0 |
| Activities of daily life | ||||
| I have no problem to conduct my activities ofdaily life | 17 | 68 | 32 | 100 |
| I have mild problems to conduct my activities of daily life | 3 | 12 | 0 | 0 |
| I have moderate problems to conduct my activities of daily life | 1 | 4 | 0 | 0 |
| I have serious problems to conduct my activities of daily life | 3 | 12 | 0 | 0 |
| I am unable to conduct my activities of daily life | 1 | 4 | 0 | 0 |
| Pain/Discomfort | ||||
| I have no pain or discomfort | 10 | 40 | 25 | 78.1 |
| I have mild pain or discomfort | 4 | 16 | 3 | 9.4 |
| I have moderate pain or discomfort | 6 | 24 | 3 | 9.4 |
| I have strong pain or discomfort | 4 | 16 | 1 | 3.1 |
| I have extreme pain or discomfort | 1 | 4 | 0 | 0 |
| Anxiety/ Depression | ||||
| I am not anxious or depressed | 17 | 68 | 31 | 96.9 |
| I am slightly anxious or depressed | 4 | 16 | 1 | 3.1 |
| I am moderately anxious or depressed | 1 | 4 | 0 | 0 |
| I am very anxious or depressed | 3 | 12 | 0 | 0 |
| I am extremely anxious or depressed | 0 | 0 | 0 | 0 |
| Score Best imaginable health* | 80 | 60-90 | 100 | 90-100 |
*Median (IQR) , DPC: Cephalic duodenopancreatectomy.
SOURCE: Authors.
TABLE 3 EQ-5D-5L questionnaire based on patients' answers (n = 57).
| EQ-5D-5L Questionnaire | DPC (n = 25) | Laparoscopic Cholecystectomy (n=32) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | OR (IC 95 %)1 | p | |
| Mobility | 0.41 [0.30-0.57] | 0.103 | ||||
| None or mild | 23 | 92 | 32 | 100 | 100 | |
| Moderate. severe problems or unable | 2 | 8 | 0 | 0 | 0 | |
| Personal care | 0.42 [0.32-0.58] | 0.254 | ||||
| None or mild | 24 | 96 | 32 | 100 | 0 | |
| Moderate. severe. or unable | 1 | 4 | 0 | 0 | 0 | |
| Activities of daily life | 0.38 [0.27-0.54] | 0.008 | ||||
| None or mild | 20 | 80 | 32 | 100 | 100 | |
| Moderate. severe. or unable | 4 | 16 | 0 | 0 | 0 | |
| Pain/discomfort | 2.50[1.52-5.94] | 0.007 | ||||
| None or mild | 14 | 56 | 28 | 87.5 | 0 | |
| Moderate. severe. or unable | 11 | 44 | 4 | 12.5 | 0 | |
| Anxiety/depression | 0.39 [0.28-0.55] | 0.019 | ||||
| None or mild | 21 | 84 | 32 | 100 | 100 | |
| Moderate. very or extremely anxious | 4 | 16 | 0 | 0 | 0 | |
| Score general health status 2 | 80 | 6090 | 100 | 90-100 | - | 0 |
1 Independence Pearson's statistical Chi squared; 2 Median (IQR); DPC: Cephalic duodenopancreatectomy.
SOURCE: Authors.
The participants expressed that their overall health perception was 80 points for Whipple (IQR 60-90) versus 100 points for the control group (IQR 90-100) (p = 0.003); however, both scores are close to the best score (100 points).
DISCUSSION
There is a limited number of studies on our population assessing the quality of life of patients after DPC, as compared to a control group, using the EQ-5D-5L questionnaire. In has been found that in general these patients report a slightly lower quality of life than the control group, which emphasizes the need to adopt in our medical practice the use of tools organize and classify this information, with a view to improving healthcare processes and perioperative follow-up. 15
DPC is a complex and high-risk procedure, indicated for pancreatic adenocarcinoma, ampullary carcinoma, ampullary adenoma, neuroendocrine tumors, cholangiocarcinoma, duodenal neoplasm, pancreatic and/or duodenal trauma, and chronic pancreatitis. 16 High volume centers report a mortality of 4 %, and up to 50% morbidity as a result of pancreatic fistula and/or gastric emptying disorders. Additionally, there are long-term consequences ranging from malnutrition - associated with weight loss and malabsorption - to the need for micronutrient supplementation. The 5 year survival es between 20 and 30 %, depending on the tumor localization: 22 % for localized, 9 % for locoregional and 2 % for metastatic disease. 17-19 In contrast, cholecystectomy is a common, intermediate risk surgery, usually laparoscopic, with the advantages of a lower postoperative pain incidence and shorter hospital stay, in addition to faster return to normal activities. 20 This is because the metabolic stress levels (activation of the sympathetic system) are lower the first day after surgery, in contrast to the open technique, where these levels normalize after three days. 21
With regards to cancer, its therapy involves physical complications, psychological alterations typical of this diagnosis, and toxic effects due to medications affecting functionality and quality of life. Therefore, management should not only focus on the disease, but in the resulting experience and the consequences on the patient and his/her environment. 7 It is important to know the short-term results of the surgical outcome of patients undergoing DPC and validate the impact on quality of life and functionality, that can be measured in terms of satisfaction with treatment outcomes, disability, mood disorders, and associated pain. 22
The evaluation of the patient's functional status, the social factors and his/ her expectations should be an integral part of the comprehensive health assessment, since these may affect the postoperative outcomes, as shown by Kim et al., in a literature review that showed that patients who readmitted after seven postoperative days, were mostly associated with social and family factors, while readmission before seven days were associated with loss of independence, and these were linked to increased mortality. 23
The surgical outcomes or the effects of therapy may be measured through the PRO, though these are not necessarily administered by the medical staff. 7,23 Patient Reported Outcomes - PRO - may be used from the immediate postop, to learn about the intensity of the symptoms and the impact on the patient. This requires a good doctor-patient relationship that facilitates communication and allows the identification of the patient's expectations with regards to the disease and recovery. The implementation of PRO in the clinical practice requires knowledge of the available questionnaires; the International Society for Research on quality of Life offers a pathway for planning and implementation. The selection of the questionnaires must take into account the characteristics to be measured: symptoms, functional performance and/ or quality of life. When administering the questionnaires, the patient should be informed about their objective, since in many cases these questionnaires will be administered periodically. 7
There are several forms available in the literature to assess the PROs. A measurement instrument EQ-5D (EuroQol until 1996) was developed in 1990 and comprises two parts: a descriptive system EQ-5D and a Visual Analogue Scale (VAS). This is a standardized, self-administered, patient-friendly questionnaire, available in 170 languages. The version EQ-5D-5L was introduced in 2009, which included a 5-dimension assessment (mobility, personal care, activities of daily life, pain/ discomfort, and anxiety/depression), each one of them comprises 5 items to describe the problem (no problem, mild, moderate, severe problems and disability). 24
The best timing for data collection varies according to the disease and the procedure; questionnaires should be administered individually to each patient, to avoid perception errors. The PROs may be distributed via email, telephone calls, text messaging, videoconferencing, or direct interview, in order to get immediate feedback on the patient's current condition. The information collected may be put to multiple uses, including research, quality improvement of care, cost auditing and evaluation. These data focused on patient experience represent feedback about medical care and help to improve clinical management processes. 25
There are controversial reports in the literature about quality of life and DPC. In 2000, Huang et al., conducted a trial to assess quality of life of patients after DPC. The sent out a questionnaire with three focus areas: physical, 15 items; psychological, 10 items; social, 5 items to 192 patients, and the resulting scores were 78 %, 79 % and 81 %, respectively. These scores were similar to the those obtained from laparoscopic cholecystectomy groups and groups of healthy volunteers and showed that patients after DPC could satisfactorily return to their daily activities, with scores that were slightly lower than those of other groups assessed. 9 In this trial, the general perception about the health status was lower among DPC patients versus the laparoscopic cholecystectomy patients, mostly because of poorer scores with regards to pain/discomfort and anxiety/ depression.
With regards to the quality of life questionnaires, in 2016 Basch et al, selected 766 patients receiving chemotherapy for solid tumors - breast, genitourinary, gynecological and lung - to be administered a measurement tool (EQ-5D) and report about worsening of symptoms to their doctors before the consult or to continue with the traditional control visits system. The treating physicians received alert messages due to worsening of symptoms, based on the answers to the questionnaire so that they could improve their care.
This study showed that those patients to whom the questionnaire was administered, reported better quality of life (34 % vs. 18 %; p < 0.001) as compared to the control group; this was a consequence of the symptoms report via the questionnaire. 26. Heerkens et al., between March 2012 and July 2016, assessed the association between quality of life measured with the EORTC-QLQ-C30 questionnaire (European Organization for Research and Treatment of Cancer - Quality of Life Questionnaire-) and the impact of postoperative complications in accordance with the Clavien-Dindo classification in 137 patients undergoing pancreatic cancer surgery. 50 % of the patients presented at least one serious complication over the first 12 months following surgery. However, there were no quality of life-associated differences between the two groups. 27
A more recent study by Sutton at al., including 35 colon cancer patients undergoing surgery, showed that the PRO metrics using EQ-5D questionnaires, in addition to other psychosocial validation parameters, enabled the identification of patients with unmet needs and postoperative difficulties. This led to the implementation of processes to design additional therapies focused on the medical gaps and ratified PRO as a promising long-term follow-up tool. 28
When comparing the various instruments to measure PRO, such as EQ-5D-5L, EQ-5D-3L and EORTC-QLC-C30, using logistic regression models, the result was that the instruments with the lowest underestimation of the results - in terms of quality of life assessment -was EQ-5D-5L; consequently, we decided to use this questionnaire for this study. 12 This research project found that the administration of the questionnaire enabled the identification of a slightly lower perception of the overall healthcare status by patients undergoing DPC, in contrast with the laparoscopic cholecystectomy patients. It should be highlighted that 20 % of the DPC group of patients reported strong and extreme pain, leading to assess the need to refer these patients to chronic pain management services during their follow-up, in order to mitigate this perceptions and lead to the development of new management policies. The literature says that pain relief after pancreatic surgery due to chronic pancreatitis may be variable - between 62 % and 85 % -, which leaves behind a number of patients experiencing chronic pain.
Risk factors for persistent pain even after one year of surgery have been identified, specifically in cases of pancreatic inflammation: long time between the onset of symptoms and surgery (over 3 years); use of preoperative opioids, and more than five endoscopic procedures. 29 In a 15-year follow-up trial including 166 patients undergoing DPC due to chronic pancreatitis, the study showed that un to 13 % of the patients continued using opioids chronically and 16 % were unable to satisfactorily return to their regular activities. 30 All of these data point to the need to change the management policies for these patients, and to involve additional services such as long-term pain management clinics.
Moreover, the results of this research project show a significant level of anxiety/ depression in these patients, which is consistent with the literature - between 30 and 50 % -, when the cause is related to cancer. 31 These symptoms usually begin before surgery and biological and molecular association have been suggested as the causal agents - overexpression of the indolamine dioxygenase enzyme, disruption in the serotonin synthesis, increased levels of metabolites such as quinolinic acid, but there are no conclusive studies to be able to establish a specific pharmacological therapy. 32 Patients at high risk of depression and/ or anxiety should be promptly identified preoperatively, in order to deliver holistic care - including psychological support throughout their treatment - since such conditions affect not just the quality of life, but long-term survival, cognition and immune system function. 33
The major limitation is that this is an observational trial with a secondary source that could be biased, since the information was not collected based on the objectives of the trial; likewise, there is information bias, specifically the participants' memory to complete the quality of life questionnaire, in addition to the absence of a serial evaluation which hinders the identification of changes over time, since this is a dynamic measurement. Further studies are required - probably multicenter trials - since this research project was conducted in just one clinical center, with specific characteristics and a multidisciplinary team that could not be available in other places. The decision was made to use the EuroQol Group questionnaire, which is a generalized and multidimensional instrument; however, it is important to validate these results through other instruments designed to measure PRO in patients undergoing DPC.
CONCLUSIONS
Patients undergoing DPC have an overall health perception slightly lower than patients undergoing laparoscopic cholecystectomy. This difference is mainly due to increased pain, anxiety/depression and limitation in their activities of daily life. No differences were identified in terms of mobility and personal care.
The use of the EQ-5D-5L questionnaire for measuring quality of life is easy and should be administered routinely, both among inpatients as well as among outpatients, taking into account that these measurements contribute with valuable information when considering intervention activities in patients, such as liaison with pain clinic and psychological assessment, so that they can be used as a reference for new management protocols focused on quality of life.
ETHICAL RESPONSIBILITIES
Protection of persons and animals
The authors claim that no experiments in humans or animals were conducted for this research project.
ACKNOWLEDGEMENTS
Contributions
JPAL: Study concept, design and plan; data collection, analysis and interpretation of the data, drafting of the manuscript, approval of the final manuscript.
CQV: data collection, analysis and interpretation of the information, drafting of the manuscript, approval of the final manuscript.
PSZ: statistical analysis, analysis and interpretation of the results, drafting of the results, drafting of the manuscript, approval of the final manuscript.











 text in
text in