What do we know about the pediatric airway?
Difficult management is the main cause of morbidity and mortality in pediatric anesthesia.
Anesthesia-related morbidity and mortality are highest in patients in the extremes of life.
General anesthetists are occasionally faced with the need to manage the pediatric airway, and complications may result in cardiac arrest, neurologic deficit or death.
What is the contribution of this review?
Nine not very well known or commonly used options to help with the successful management of the pediatric airway are described.
Knowing and incorporating adequate devices and techniques into the practice of anesthesia can improve quality of care and reduce perioperative morbidity and mortality in children undergoing anesthesia.
INTRODUCTION
Studies that assess morbidity and mortality in pediatric patients describe three main causes 1-3: respiratory complications derived from airway management -approach, laryngospasm, bronchospasm and acute hypoxia - which may result in cardiac arrest, neurologic deficit, or death; hemodynamic complications - hypotension and bradycardia; and medication errors. Some considerations that change clinical practice in pediatric airway management have been reported and reintroduced (Figure 1). This literature review aims to identify and summarize the findings related to the primary cause of morbidity and mortality in pediatric anesthesia, and emphasize things that anesthetists need to know based on the scientific reports that have been changing practice in pediatric anesthesia (Table 1).
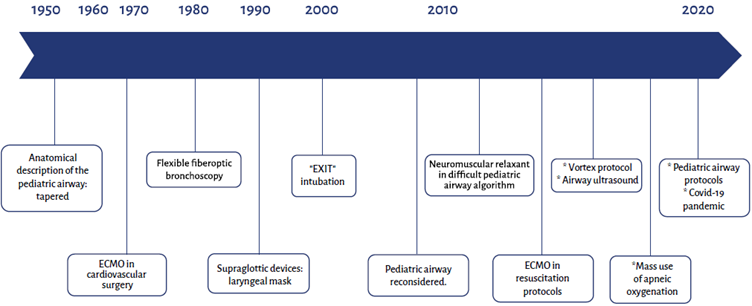
From 1950 to 2020. ECMO: Extracorporeal membrane oxygenation; EXIT: Ex uteri intrapartum treatment; US: Ultrasound. SOURCE: Author.
FIGURE 1 Timeline of developments in pediatric airway management.
PEDIATRIC AIRWAY ASSESSMENT
Three recently introduced elements are highlighted: pediatric airway classification, anatomical changes and ultrasound use.
Pediatric airway classification
Predictors in adults (Mallampati, thyromental distance, mouth opening, etc.) are not applicable in pediatrics because absolute measurements change in relation to growth. The Mallampati classification is valid in children over 5 years of age 4. In pediatrics, the use of a classification based on three elements has been proposed since 2010 5-7:
Past history. Previous experiences with the approach to the airway are considered. A history of a difficult management is highly sensitive and specific for the diagnosis of a difficult airway (DA); tracheostomy, prolonged intubation and post-extubation dysphonia are warning signs of potential difficulties during management.
Physiological changes. Active flue or flu episode within the past three weeks; a history of epiglottitis, bronchospasm, rhinitis, obstructive sleep apnea syndrome, adenoid or tonsillar hypertrophy are associated with DA. Pediatric patients with an apparently normal airway may develop complications such as laryngospasm and bronchospasm, resulting in rapid arterial desaturation that requires immediate implementation of adequate management strategies.
Anatomical abnormalities. Abnormalities of the lower third of the face, low-set ears, limited neck mobility and inability to open the mouth at least 3 of the child's finger breadths are associated with DA. In children who cooperate, the inability to project the mandible farther than the maxilla (inability to bite the upper lip with the lower teeth) is a finding associated with DA. A higher body mass index (obesity) is associated with greater perioperative complications 8.
Based on these three elements, the pediatric airway is classified as follows:
A. Anticipated difficult airway. Patients with abnormal anatomy or a clear history of DA. Examples: dysmorphic syndromes such as Pierre Robin. These children must be referred to specialized centers with expert staff and special resources for pediatric anesthesia.
B. Altered or suspect airway. Patients with no anatomical abnormalities but with physiological respiratory disorders or a history of prolonged airway manipulation, e.g., intubation in the ICU, history of tracheostomy or a flu episode. These children can be managed by general anesthetists provided the support from experts in pediatric anesthesia is available at the service.
C. Normal airway. Patients with no past history or anatomical of physiological disorders who can be managed by general anesthetists. An extremely low percentage of these patients may present with unanticipated DA.
Pediatric airway anatomy
Anatomical differences between pediatric and adult airways are clear. In the past, the shape of the pediatric larynx was described as tapered while the adult airway was described as cylindrical. This "dogma" in pediatric anesthesia emerged more than half a century ago from the studies by Eckenhoff 9, based on prior studies by Bayeux 10 and experiments with mummified pediatric anatomical models. In vivo studies 11,12 with computed tomography, magnetic resonance and fiber-optic bronchoscopy with spontaneous breathing suggest that the pediatric larynx has the same cylindrical shape of the adult larynx - even somewhat elliptical - with the anteroposterior diameter being longer than the lateral diameter and having two sites of maximum narrowness at the level of the cricoid ring, as described in old studies, and at the level of the vocal cords as a new finding 13,14. The controversy is still open with some experts challenging these findings 15 partly on the grounds that these measurements - comparisons not only between cadaver models and live children but also between spontaneous and controlled breathing, or even between inspiratory and expiratory phases - make consensus difficult 16,17. A useful recommendation in pediatric anesthesia is the use of tubes with pneumoplug, taking care not to exceed a balloon pressure of 20 mmHg 18, which has shown to be associated with a lower incidence of reintubations from tube exchanges, and a lower need for inhaled anesthetics 19.
Ultrasonography for the study of the pediatric airway
Ultrasound (US) was initially used to assess the adult airway 20, but publications on the assessment of the pediatric airway have been emerging over the past five years 21. US is used to make measurements that help predict a difficult approach to the airway, including the amplitude of the retrolingual space and the ability to measure the distance between the arytenoid cartilages in order to select the right endotracheal tube diameter 22. A superficial neck scan allows to identify the location of the cricothyroid membrane and tracheal rings for guidance should the need for emergency percutaneous access arise. Correct endotracheal intubation as well as selective ventilation due to endobronchial intubation can be detected by US through comparison of bilateral "pleural movement". Although these are simple, real-time bedside measurements, they are operator-dependent and require training to ensure correct image interpretation.
APPROACHES
Three techniques that have been reintroduced over the past decade are described.
Apneic oxygenation
An old technique consisting of the use of high flow nasal cannula (up to 15 liters per minute in adolescents) besides the conventional facial mask during anesthetic induction in order to achieve longer safe apnea time 23 and reduce the possibility of arterial desaturation which is faster and more severe in pediatric patients because of their lower functional residual capacity (oxygen reserve) and higher tissue oxygen consumption. The effectiveness of this simple practice has been proven, especially in the presence of DA, in patients with prior lung compromise, in critically ill patients 24, or whenever there is a risk of aspiration, where positive pressure ventilation during induction would be contraindicated 25. Isolated cases of pneumothorax have been described with the use of high flow devices in children 26.
Extracorporeal oxygenation
Derived from cardiovascular surgery, this form of oxygenation is maintained by means of an external oxygenation membrane and a pump to drive circulation while the heart remains in asystole. This device can provide two hours of cardiopulmonary support; after that time, it triggers inflammatory processes and serious cellular alterations. Extracorporeal membrane oxygenation (ECMO) came later and allows for longer periods of pulmonary and/or cardiac support, even over several days, without the acute problems associated with the extracorporeal circulation pump used in cardiovascular surgery. The use of ECMO, described in pediatrics since the 1970s 27, has been expanded and has been incorporated in cardiopulmonary resuscitation algorithms, for example 28. It also offers a management option in cases in which the pediatric airway is lost completely, for example in mediastinal mass resection or tracheal surgery 29,30. ECMO is effective at providing adequate oxygenation of the blood and removing CO2, allowing work on the airway for as long as it is needed. A specialized center with the necessary resources and staff training is required for its implementation. It is not widely used in our setting as of yet.
Fetal EXIT (Ex Uteri intrapartum treatment)
This procedure consists of maintaining the fetus attached to the placenta during cesarean delivery while the fetal airway is approached with the most appropriate technique for each individual case, ranging from traditional laryngoscopy to flexible fiberoptic bronchoscopy assistance or tracheostomy 31. It was first described in 199732 and its use has been growing due, on the one hand, to prenatal visits that allow early identification of fetal abnormalities that compromise the airway and, on the other hand, to ease of implementation 33. Once the airway is secured, the umbilical cord is ligated and the delivery can proceed. There is always the possibility of placental detachment or interruption of blood flow to the umbilical cord, requiring either faster maneuvers on the fetal airway or delivery and traditional neonatal airway management in an adjacent room.
DEVICES
Devices for the management of the pediatric airway may be grouped under three categories, as described below.
Basic or first-line (for ventilation)
The use of the facial mask, with or without the support of an oral or nasal cannula 34, to secure appropriate ventilation and oxygenation in the vast majority of children is the cornerstone for the management of the pediatric airway. Endotracheal intubation is secondary, except in specific conditions such as the risk of aspiration which requires securing the airway as soon as possible. There are no new considerations to discuss in this regard.
Intubation devices
Laryngoscopes. Essentially everything that is available today for adults is also available for pediatric patients, from the traditional laryngoscope with different blade sizes and styles - the straight blade offering some advantages in children - all the way to modern videolaryngoscopes 35. The latter, however, have not been shown to have the same results as in adults because they require longer intubation times when compared to the conventional laryngoscopes and are associated with lower first-attempt success. This may be attributed to the curvature angle of the blades which should be greater in pediatrics and also to the fact that they do not necessarily offer better alignment of the oral, pharyngeal and tracheal axis for intubation even though vision is better 36,37. Greater success with videolaryngoscopy has been reported in intensive care settings 38,39. Vendors offer blade sizes ranging from 00 to adult sizes and even devices that can be connected to a cell phone screen. Some of the most common videolaryngoscopes are the Storz®, GlideScope®, Truview®, Pentax AWS®, Airtraq®, McGrath®, and kingVission®, among others. The choice depends on the preference of each work team, budget availability and experience.
Supraglottic devices. There is a wide range of supraglottic devices for pediatric use, essentially the same as in adults 40. The first version of the laryngeal mask was described by Archie Brain in 1980 and its use in pediatrics became widespread since 1990. Studies show that second generation laryngeal masks offer greater advantages in terms of placement, less dislodgement, ease of ventilation and oxygenation; they also allow suction of gastric contents, some incorporate bite protector, and they also allow passage of traditional tubes for endotracheal intubation 43. Each work team must make a rational selection of the devices that best suit their practice.
Fiberoptic bronchoscope. Flexible fiberoptic bronchoscopy is the gold standard approach to the anticipated DA, while rigid fiberoptic bronchoscopy is the choice for removal of foreign bodies lodged in the airway. In "cannot ventilate, cannot oxygenate" scenarios, it can be used before front-of-neck access (FONA) 42. Since the description of flexible fiberoptic bronchoscopy in pediatrics in 1978, fiberoptic bronchoscopes of different sizes, even in diameters as small as 1.8 mm that allow the passage of a 2.5 mm internal diameter endotracheal tube have been developed. The smaller the fiberoptic bronchoscope, the finer the optic fiber and the greater the probability of damage. The 2.8 mm fiberoptic bronchoscope is the most commonly used in pediatrics and passes through 3.5 mm internal diameter tubes and larger. In the absence of experience with fiberoptic bronchoscopy in children, support from the pediatric pulmonologist must be requested. An option that has gained increasing popularity is the combination of devices, for example, flexible bronchoscopy-guided endotracheal intubation through a supraglottic device, described as successful in large series 43.
Front-of-neck surgical access (FONA)
There is an ongoing debate in pediatrics on whether this access is useful, especially in very young children, because of the very high incidence of complications and failed procedures, with an increase in inhospital mortality 44 due to issues such as location of the cricothyroid membrane and incorrect approach 45. This approach requires a very clear rationale. In a "cannot ventilate, cannot intubate" scenario in which none of the available options have worked when applied correctly and the child is going into acute hypoxemia, bradycardia, cardiac arrest and death, the only option is to resort to this procedure. The approach through the cricothyroid membrane is not recommended in children under 8 years of age due to the difficulty in identifying the space correctly and passing a tube of adequate size; therefore, it must be done through the tracheal rings 46. This procedure may be performed through puncture - percutaneous or open cricothyroidotomy - or through an incision - percutaneous or open tracheostomy. If no surgeon is available, the percutaneous access must be established by the anesthetist.
WHAT IS NEW IN ALGORITHMS
Different considerations
The different algorithms give priority to facial mask ventilation over endotracheal intubation because it is usually easier to ventilate children with the adequate facial seal technique which allows, with positive pressure, to create an air column that acts like a "splint" to maintain an open patent airway. In this scenario, intubation, usually more difficult in children, would take second place 47. On the other hand, in case of difficult ventilation or intubation and the absence of anatomical predictors of a difficult airway, neuromuscular relaxation can be used, as it makes it easier to provide facial mask ventilation and endotracheal intubation 48,49. The basic algorithm of facial mask ventilation followed by attempted intubation and/or placement of a supraglottic device continues to prevail, and if a "cannot ventilate, cannot oxygenate" emergency occurs, access through the neck would be considered. In pediatrics, combining strategies is valid, especially the combination of fiberoptic bronchoscopy + supraglottic device. The possibility of arousing the child to allow spontaneous breathing must be considered depending on each particular case 50. Intubation without muscle relaxation is feasible in neonates, using "gentle" ventilation (high frequency and low volume) in anticipation to rapid desaturation.
Vortex protocol
Described by an anesthetist and emergency physician in Australia 51, it consists of a funnel visual schematic that begins, at the top, with airway management using three of the four "life lines" - facial mask, endotracheal intubation and supraglottic devices - which are applied and alternated depending on the individual case in order to always maintain the patient in the green safety zone, with adequate oxygenation and ventilation. The fourth "life line", i.e., neck access in any of its modalities already described, is activated when the previous have failed. The protocol highlights nontechnical skills and teamwork and includes other important considerations besides the mere implementation of a sequence of steps contained in the algorithms. It can be accessed for free at http://vortexapproach.org where a more thorough description of the components and uses is available.
Considerations during the COVID-19 pandemic
The incidence of asymptomatic carriers among children is high, requiring great care during their management. Crying should be avoided whenever possible, because of abundant droplet production; therefore, excellent premedication and peaceful arousal are required. Positive pressure ventilation is allowed in neonates considering that low volumes result in minimal droplet scatter - less than 10 cm radius. Whenever possible, tubes with adequately inflated pneumoplugs should be used over supraglottic devices. This topic not being within the scope of this review, only the most important recommendations are summarized in Table 2, based on the recommendation of the Colombian Neonatology Association (ASCON) 52 and the consensus guidelines of the Pediatric Difficult Intubation Collaborative and the Canadian Pediatric Anesthesia Society 53.
TABLE 2 Recommendations for pediatric airway management during the COVID-19 pandemic.
SOURCE: Author.
CONCLUSIONS
Recent studies have led to paradigm changes in pediatric airway management. The anatomy of the pediatric airway is reassessed in vivo and the use of endotracheal tube with pneumoplug is proposed. Although intubation in children is more challenging, when a good technique is used, facial mask ventilation and oxygenation are easier. Tools are available for the objective assessment of the pediatric airway, enabling classification and determination of the level of care. The classification of altered or suspect airway is highlighted as a warning sign to anticipate potential complications. A large number of devices for approaching the airway are available in the market, essentially the same as are available for adults, including laryngeal masks for neonatal intubation. In a "cannot ventilate, cannot intubate" scenario, neuromuscular relaxation is an accepted option before front-of-neck access, or arousing the child if circumstances allow it. Techniques such as apneic oxygenation, ECMO and fetal EXIT may save lives in many cases. Finally, everything that has been described regarding pediatric airway management will be truly effective if anesthetists are trained in the use of the most accesible and adequate devices for every circumstance and if protocols and care guidelines are designed, shared and implemented, without losing sight of the fact that the cornerstone of pediatric airway management continues to be facial mask ventilation and oxygenation.











 text in
text in 



