INTRODUCTION
Foreign body aspiration (FBA) is a paediatric emergency that can cause death from asphyxia 1,2. Making a diagnosis based on an abnormal physical examination and / or a radiological study only is often difficult. The rate of errors and discrepancies in radiology is around 3-5% 3, including the acquisition of abnormal images that suggest the presence of foreign bodies.
Thus, clinical evaluation of the child is essential, including a detailed anamnesis, preferably with a suggestive history of aspiration or a witnessed episode of asphyxia, and a thorough physical examination Further investigation and treatment sometimes require rigid bronchoscopy under general anaesthesia 2 in a remote location, far from the central operating room; so the level of reliability on the diagnosis prior to the procedure should be high.
Our objective was to highlight the importance of a multidisciplinary approach, discussing the clinical and imaging findings with the participation of the Radiologist, Anaesthesiologist, Pulmonologist and Paediatrician.
CLINICAL CASE
Following the obtention of the informed consent drafted by the Ethic's Committee of Centro Hospitalar Vila Nova de Gaia/ Espinho signed by the parents, the case of a 34-month-old girl, ASA II, referred for urgent rigid bronchoscopy on suspicion of FBA was presented.
The patient had a history of recurrent wheezing, and was followed by the Paediatric-Allergology clinic. From the age of 15 months the child frequently visited the paediatric emergency department with signs of respiratory distress: wheezing, dyspnoea, nose flaring, chest retractions and low peripheral oxygen saturation (-90%). The symptoms improved with inhaled salbutamol and she was never admitted to the paediatric ward for this reason. She had two normal previous chest X-rays and a negative Asthma Predictive Index. She was prescribed inhaled salbutamol 100 μg/dose (4 doses/day) and budesonide 200 μg/dose (1 dose/day), with poor treatment compliance. The parents were smokers and she was passively exposed to tobacco smoke. She had no known drug allergies and her National Vaccination Plan was in order.
She was brought to the emergency department because of suspected ingestion of a metallic blade 30 minutes earlier, having been found chewing on the object. No respiratory distress signs (RDS) were present at the time of the FBA. On objective examination, she presented wounds on her face and left lower lip (minor bleeding) and traces of lamina powder on the lower molars, with no additional findings. Her heart rate was 130bpm and blood pressure of 100/60mmHg. Eupnoeic (20 bpm), with a peripheral oxygen saturation at rest on air of 97%. No signs of choking, cough, sialorrhea, stridor or other RDS. Hydrated mucosa, without rashes, petechiae or other. No fever. Parents were unaware of pain. The cardiopulmonary auscultation and abdominal examination were normal.
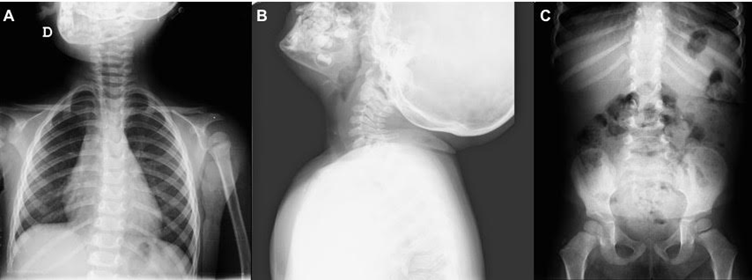
The AP view of radiographic study of the chest showed a small linear radiopaque image in the topography of the right upper pulmonary lobe (Fig. 1A). A similar image was identified at the level of the cervical trachea on the profile radiograph of the cervical spine (Fig. 1B). The abdominal x-ray, showed tiny radiopaque images on the topography of the gastric chamber, compatible with traces of the metallic object (Fig. 1C).
SOURCE: Authors.
FIGURE. 1 A. Chest X-Ray (AP): linear radiopaque image in the right upper pulmonary lobe; B. Cervical Spine Radiography (profile): similar image at the level of the cervical trachea; C. Abdominal Radiography (AP): radiopaque images on the topography of the gastric chamber.
During the pre-anaesthetic evaluation, in the absence of clinical signs compatible with FBA in a child with a history of bronchial hyperresponsiveness, the possibility of error in image acquisition / interpretation was considered. After a discussion with the Radiologist, a new direct digital radiographic study was conducted, with no images compatible with foreign bodies (Fig.2). The initial findings were considered to be artefacts and rigid bronchoscopy was not performed.
The child fasted and remained on clinical surveillance in the paediatric ward next to the paediatric emergency room for 24 hours. Temperature, heart rate, respiratory rate, blood pressure and pain were monitored every 2 to 3 hours, with no abnormal findings. The peripheral oxygen saturation was constantly monitored (98100%). Apart from fluid therapy, no other treatments or interventions were required.
At discharge, the patient was hemodynamically and clinically stable and tolerating oral feeding.
DISCUSSION
FBA is a more frequent occurrence in three to four year-old children 2 and is more common in males 1. It presents with a wide spectrum of manifestations 4,5, making its diagnosis challenging. It is essential to investigate a suggestive history or witnessed episode, search for acute manifestations and airway compromise, and to take radiographic images to identify and locate the foreign bodies and exclude complications or other causes. The nature of the aspirated material, the location of the obstruction, the time since aspiration and whether the child is fasting 1 should also be considered.
As stated by Fidkowski CW. et al 1 and Sink J. et al 5, organic materials (nuts and seeds), which easily swell and inflame, are the most frequently associated agents, with the bronchial tree being the most typical location. The larynx and trachea are usually less common places, although, if involved, they represent a higher risk due for the potential of total airway occlusion. The episode may manifest acutely, with expulsive cough, dyspnoea, wheezing 4,5, cyanosis and stridor, or late, with decreased unilateral vesicular murmur, intercostal retraction, recurrent pneumonia or pneumothorax 4.
Anteroposterior and lateral cervical radiographs and chest radiographs should be performed 2,4. However, according to Abd-ElGawad EA. et al 2, images are normal in about 30% of the cases and in 14 to 37% according to Hitter A. et al 4, since most foreign bodies are not radiopaque and typical indirect signs (emphysema, atelectasis, pneumothorax) are not present in all patients. Similarly, in a 2016 study with 102 children by Sink J. et al 5, sensitivity and specificity of imaging studies was 61% and 77%, respectively, with air trapping as the most frequent anomalous radiographic finding. However, the sensitivity and specificity of chest x-rays improves 24h after the episode 4.
In a child with suspected FBA with a past history of airway hyperresponsiveness, a positive radiological study but without any suggestive clinical signs, requires a sensible clinical approach based on the low initial sensitivity of imaging tests. Furthermore, an observed event has a positive rate of 87% for foreign body aspiration on bronchoscopy 6, which further increased our doubts in this particular diagnosis.
In this case, the cervical radiography - often requested in emergency settings, despite its diagnostic sensitivity of only 25.3% 7 - is intended to identify the presence of foreign bodies in the upper aerodigestive tract, but their exact location remains unclear. This exam often reveals soft tissue oedema, loss of cervical lordosis, or objects posterior to the trachea 1, but none of those were present in our case. We decided to perform a new radiographic study by direct digital acquisition; however, in case of high clinical suspicion, multidetector computed tomography imaging 1,4,7 is another option, with a sensitivity of almost 100% and a specificity ranging from 66.7 to 100% 4.
It should also be noted that image identification and interpretation by the radiologist are not totally error free 3. There is a myriad of causes: technical factors resulting, for example, from the imaging protocol used or the patient's body structure, influence of the clinical episode description (in this case, highly suggestive), relevant medical history (the existence of a wheezing diagnosis was a confounding factor), previous exams, cognitive biases, amongst others 3. Following a careful pre-anaesthetic clinical evaluation, with high degree of suspicion and excellent communication with our Paediatric, Radiology and Pulmonology colleagues, the conclusion was that the initial images represented a false positive, probably due to secretions, endoluminal sections, overlapping calcified or ossified structures 7 or, more likely, artefacts 2.
In terms of other diagnostic options leading to treatment, rigid bronchoscopy has been the gold-standard and most frequently used method of approaching FBA events 8. Nevertheless, considering that bronchoscopies are negative in a significantly variable percentage of cases 9,10 to 61% 4, potential complications were thus avoided (laryngeal oedema, pneumothorax, tracheal or bronchial laceration, hypoxia, cardiopulmonary arrest, among others 4). We were also concerned about other issues with this procedure, including difficult ventilation due to obstruction or atelectasis and the risk of transformation from partial to complete obstruction after anaesthetic induction 1. In this case, we avoided the risks of performing rigid bronchoscopy in a small child, in a remote place and with the support of unskilled staff.
Most recently, several studies have described the use of flexible bronchoscopy in this context, applying a myriad of different techniques 8,10,11. Flexible bronchoscopy has a number of advantages vs. rigid bronchoscopy: lower complexity and less time to perform 12; less trauma, lower risk of complications and allows for the identification and localization of foreign bodies in more distal bronchial areas, maintaining the diagnostic capacities as its main strength 8. Nevertheless, rigid bronchoscopy is usually necessary when dealing with more complicated airway instrumentation; hence the rigid bronchoscope should be immediately available if flexible techniques prove ineffective 13, 14. Consequently, proper management may be delayed and it is yet impossible to ascertain the superiority of flexible bronchoscopy in these cases 15.
In our clinical case, based on the high diagnostic suspicion but without a severe acute patient, flexible bronchoscopy could have been our diagnosis/treatment option if a conservative approach was not chosen. This approach in stable patients had already been advocated by Sheehan C. et al 9 and Haller L. et al 14. Watchful waiting was made possible based on the child's constant clinical surveillance and prompt availability of the anesthetic and bronchology team if deterioration occurred.
In conclusion, paediatric pre-anaesthetic evaluation, regardless of the context, on a routine or urgent basis is essential. When the clinical presentation is inconsistent with the history of the patient and/or with the radiographic images, a multidisciplinary approach is a must, in order to avoid delays in the identification and treatment of a potentially life-threatening situation and, also to avoid unnecessary invasive procedures involving significant anaesthetic risk for paediatric patients.
ETHICAL DISCLOSURES
Protection of human and animal subjects The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data The authors declare that no patient data have been disclosed in this article.
Right to privacy and informed consent A first degree relative gave express written consent, authorizing the publication of the case and the diagnostic test images. This document is the possession of the corresponding author.
Presentations
Not all you see is what it seems to be: challenges in pediatric foreign body aspiration" presented as a poster in the Portuguese Anesthesiology Society Congress, March 2019.
Not all you see is what it seems to be: challenges in pediatric foreign body aspiration" presented as a poster in Euroanaesthesia, June 2019.











 text in
text in 




