INTRODUCTION
There is frequently the assumption that pregnant women with intracranial lesions experience increased intracranial pressure and the risk of herniation is considered a contraindication for neuraxial anesthesia. 1
Tuberous sclerosis (TSC), is a disorder caused by alterations in one of two different genes, the TSC1 gene or the TSC2 gene with multi-systemic involvement, mainly of the central nervous system, producing benign tumors in the brain and in other organs. Seizures and renal hemorrhage are frequent manifestations of this disease.2-3
For the anesthesiologist, the decision to administer regional versus general anesthesia in patients with intracranial lesions is challenging. A risk-benefit balance is necessary, since none of the two approaches are free from harm.4-6
The recommendations for the management of anesthesia in pregnant women with brain tumors 6-8 are not always straightforward when the patient does not have intracranial hypertension. The decision about whether to administer neuraxial anesthesia or not, will depend on the anesthesiologist, the patient's preference, and a comprehensive preoperative assessment. 7-9
This article discusses the case of a parturient with TSC who underwent a category 2 caesarean section under combined spinal-epidural anesthesia (CSE), and developed a neurological complication 24 hours after surgery.
The patient submitted her written consent.
CASE REPORT
This 28-year old primiparous patient had been diagnosed with TSC during childhood, after presenting generalized tonic-clonic seizures and typical skin manifestations, such as hypomelanotic macules, facial and nail angiofibromas. A TSC2 gene mutation was isolated.
The prenatal risk assessment did not show any signs of cardiac, renal, retinal, or pulmonary dysfunction, and neither any cognitive disorders.
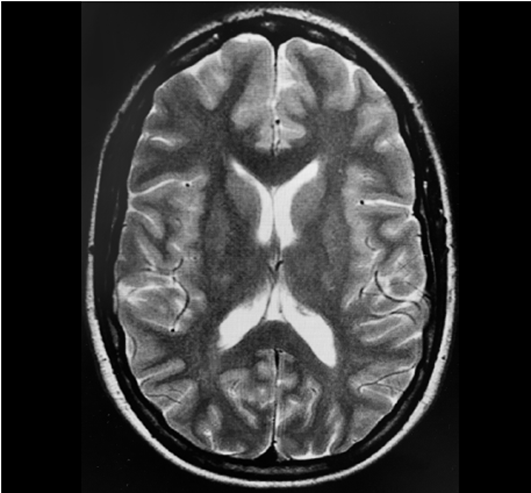
The last brain magnetic resonance imaging (MRI) performed in February 2017 showed no evidence of evolution of subcortical tubercles or sub-ependymal nodules, which are specific to the disease (Figure 1). She had not experienced any epileptic crisis since 2014 and was being treated with lacosamide 250 mg twice a day throughout her pregnancy. She experienced three episodes of tension migraine with spontaneous remission during pregnancy. In 2019 the patient was admitted to the hospital with premature rupture of the fetal membranes in her 3ist week of gestation, and a caesarean delivery was indicated because of poor fetal tolerance. The minimum fasting period established was six hours prior to the procedure, after having a light meal. Blood analyses did not show any significant alterations. In the absence of signs of intracranial hypertension (ICH), and based on the previous imaging tests, CSE anesthesia was administered uneventfully. After locating the epidural space at the level of L3-L4 with an 18-Gauge Tuohy needle, 9 mg of 0.5% hyperbaric bupivacaine plus 20 micrograms of fentanyl were administered using a 27 G Whitacre needle. The epidural catheter position was 10 mm. No complications developed during the intraoperative and early postoperative period.
After 24 hours, the patient developed left-side facial-brachial hypoesthesia and left hemicranial headache, with no other neurological signs. An urgent brain MRI was performed, which showed a recent onset, right frontal cortical bleeding tumor with no mass effect. A 3D-MRI was then performed for a more accurate diagnosis of the tumor and anatomic description (Figure 2). The patient was diagnosed with glioblastoma multiforme, and was then discharged 15 days after admission, with residual paresthesia in the left hand, and was scheduled for elective neurosurgery.
The patient underwent a macroscopic total removal of all visible tumors, followed by subsequent cycles of radiation therapy and was monitored by the oncologist.
DISCUSSION
This case illustrates the difficulty in prescribing a neuraxial block for labor in the presence of a chronic brain condition such as TSC. In the presence of a severe neurological complication, the neuraxial block may be blamed as the culprit for the complication. 9-11
Tuberous sclerosis is a multisystem disease with predominant involvement of vital organs, especially the central nervous system. The Tuberous Sclerosis Association has established the criteria to diagnose TSC. 3(Chart 1). The course of the disease varies according to the patient, and presents with mild to very severe symptoms. Tumors may grow in any organ, but most frequently they develop in the brain and the kidneys. Malignant tumors are unusual, and primarily occur in the kidneys. With appropriate medical support, most patients can have a normal life expectancy. 2-3
CHART 1 Diagnostic Criteria for Tuberous Sclerosis according to the American Association.
| Major Criteria |
|---|
|
|
| Minor Criteria |
|
|
SOURCE: Authors.
In terms of neurological lesions, these are characterized by the presence of three types of benign tumors or hamartomas. The cortical tubers usually appear on the surface areas, though they may develop deeper inside the brain; subependymal nodules emerging from the ventricular wall, and astrocytomas that may cause ICH by blocking the cerebrospinal fluid (CSF) drainage. 2,6
11% of the patients develop hamartomas and other upper airway tumors, which makes general anesthesia difficult due to the potential risk of obstruction and bleeding. 12 Fleisher 12 describes approaching the airway using Sevorane induction and fiber optic bronchoscopy, as well as dexmedetomidine in awake patients. Therefore, the management of the airway should follow the recommendations of the anesthesiology guidelines in patients with a difficult airway.12
All pregnant women with ET, before delivery, should undergo a brain and spinal MRI to rule out any space occupying or vascular lesions that are a contraindication for epidural analgesia or spinal anesthesia. Specifically, in patients with an additional diagnosis of epilepsy, not having an MRI is a contraindication for epidural analgesia or spinal anesthesia.13 There is no consensus recommending the time to repeat a new imaging test, but given the natural evolution of the disease, the development of any neurological symptoms during pregnancy makes it necessary to consider the need for a new MRI to avoid diagnostic delays, particularly in this type of patients.
In the absence of contraindications for neuraxial anesthesia, pregnant women with brain tumors who show no mass effect, no clinical findings, or images suggestive of ICH, are likely to have a minimum risk of complications after a dural puncture. So there is always the need to weigh the benefits versus the risks of administering neuraxial or general anesthesia. 9,11
In our case, the patient was neurologically stable. The stability of pathologic intracranial lesions in a prior MRI leads us to believe that the patient had not experienced any recent intracranial processes. The fact that our patient experienced several episodes of headache with spontaneous remission during pregnancy, was not considered an alert sign, since this is a frequent occurrence during pregnancy 13, and no additional neurological symptoms were present.
In our case, the intratumoral bleeding mechanism was unclear, and the chronology of the onset of the headache and focal deficit was compatible with a spontaneous tumor bleeding. One could argue that it could also be related to a drop in intracranial pressure due to a cerebrospinal fluid fistula in the lumbar epidural space after the CSE, as described in the literature. 11,13 However, this is unlikely, when using a 27G Whitacre spinal needle, especially if the intracranial pressure was previously normal and a single puncture was performed. 14-15 In fact, Shaik et al. 14 described an incidence between 1.1 and 12.8% of post-dural puncture headache (PDPH) after CSE for scheduled caesarean section. However, Muhammad et al.15 reported a PDPH incidence of 0% with a 27G Quincke needle in this setting. During vaginal birth, the risk of PDPH is increased when the patient makes an active pushing effort for vaginal birth, but the risk of PDPH is certainly lower in cesarean section.15
In this case, the development of intracranial bleeding after delivery, may be the result of the rapid hormonal and hemodynamic changes during the postpartum period; the impact on coagulation and on the blood vessel walls may have caused the bleeding of a preexisting intracranial lesion.
Nevertheless, some studies have shown that ICH primarily develops during the antepartum period, especially during the third trimester. Our patient did not experience any hypertension, nor did she have a history of preeclampsia during pregnancy, but she described migraine episodes that may be predisposing for tumor bleeding.16
When a caesarean section is performed under general anesthesia in a patient with an intracranial tumor, the risk of hemodynamic changes during tracheal intubation and surgery increases, which may affect the intracranial pressure. 9,13,17 Therefore, choosing the best anesthetic technique may be challenging and the advantages and disadvantages of each technique should be considered, in addition to any relative and absolute contraindications for neuraxial block (Chart 2).13
CHART 2 Contraindications to neuraxial block in obstetric patients.
| Absolute: |
|
|
| Relative: |
|
|
| Controversies: |
|
|
SOURCE: Authors.
Finally, in patients with TSC, an accurate diagnosis of all the masses should be performed and any frequent comorbidities such as epilepsy, respiratory tract lesions, Wolff-Parkinson-White syndrome-related cardiac arrhythmias 9, or kidney tumors that could impair the renal function, should be ruled out before delivery. 3,9,10,11 A strict neurological follow-up after delivery is highly recommended to detect any postpartum complication like in the case of our patient.18 There is no literature in our country regarding the diagnosis of glioblastoma multiforme in pregnant women with tuberous sclerosis.
CONCLUSION
This is a case report of a preterm twin delivery in a patient with TSC who developed intracranial bleeding associated with an unidentified glioblastoma, 24 hours after caesarean delivery under CSE.
Intradural or epidural anesthesia should be administered upon imaging of the brain and the spinal structures. A finding of ICH or medullary tumors are a contraindication for neuraxial techniques. In contrast, the absence of lesions is probably not reliable enough to rule out the subsequent occurrence of another lesion, and any unusual symptoms should be subject to further investigations.
ETHICAL DISCLOSURES
Protection of human and animal subjects The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent The authors declare that no patient data appear in this article. The authors have obtained the informed consent of the patient and/or subject referred to in the article. This document work in the power of the correspondence author.
ACKNOWLEDGMENTS
Contribution by the Authors
CRA: Assisted in gathering the articles and writing the paper.
NB: Assisted in gathering the articles for the introduction and discussion, and in writing the paper.
LDDP and EGA: Assisted in gathering the articles for the introduction and discussion.
FGR: Assisted with writing the paper.











 text in
text in