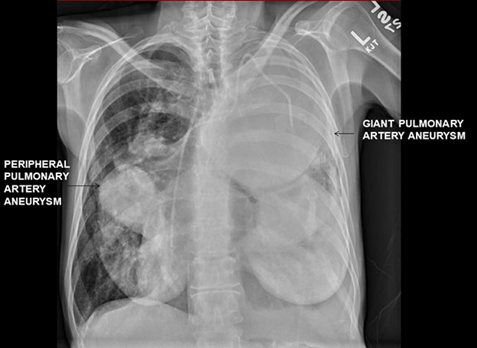
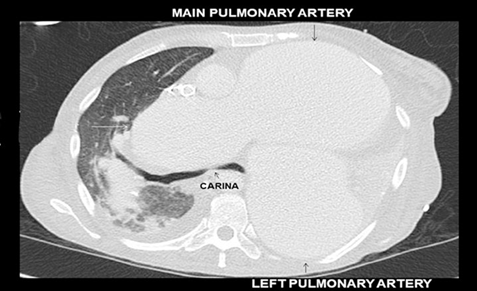
The accompanying images demonstrate giant pulmonary artery aneurysms in a patient with idiopathic pulmonary arterial hypertension (Image 1). In addition to the main pulmonary artery, both the left and right pulmonary arteries are aneurysmal and are compressing the lung parenchyma (Image 2).
SOURCE: Authors.
IMAGE 1 Giant pulmonary artery aneurysms in a patient with idiopathic pulmonary arterial hypertension.
SOURCE: Authors.
IMAGE 2 Left and right pulmonary arteries are aneurysmal and are compressing the lung parenchyma.
Congenital cardiac heart disease, infection and pulmonary arterial hypertension are leading causes of pulmonary artery aneurysms. Giant aneurysms (diameter >8 centimeters) can compress adjacent structures including the tracheobronchial tree leading to dyspnea, cough, chest pain, wheezing and stridor. Hemoptysis may herald aneurysm rupture. Additionally, tracheobronchomalacia can occur resulting in dynamic airflow obstruction.1,2
Diagnosis is often established with radiological imaging. Ventilation perfusion mismatch from lung collapse in patients with giant aneurysms can worsen cyanosis and hypoxemia related to pre-existing pulmonary arterial hypertension. Alleviation of such collapse and tracheobronchial compression may necessitate airway stenting.
Increases in pulmonary vascular resistance related to increased intrathoracic pressure and excessive sympathetic stimulation can precipitate aneurysm rupture, airway bleeding and exsanguination. Anesthetic management focuses on mitigating such factors. Although spontaneous ventilation minimizes increases in intrathoracic pressure, optimal placement of airway stents necessitates a still deployment field and muscle relaxation to minimize coughing. Awake fiberoptic intubation allows placement of the endotracheal tube beyond the point of tracheal compression safely in most circumstances. Pre-induction establishment of invasive arterial monitoring and large bore intravenous access is important. Induction is best initiated with the patient positioned upright to maximize functional residual capacity. Use of low tidal volume ventilation while avoiding excessive PEEP and recruitment maneuvers is also prudent. Critical airway obstruction, compression at the level of the carina, impending respiratory failure and refractory hypoxemia may warrant institution of pre-induction venovenous extracorporeal circulatory life support. Lastly, topicalization of airway with lidocaine and/or use of intravenous remifentanil infusion during emergence from anesthesia, may help mitigate coughing and stent displacement. 1-3











 text in
text in 



