What do we know about this topic?
Access to essential medicines, including opioids, is a component of the right to health. Strong opioids are a cornerstone of pain treatment. Morphine, fentanyl, hydromorphone, methadone and oxycodone are included in the WHO Model List of essential medicines for pain relief and palliative care.
What does this study contribute?
There are barriers to opioid availability and access in Colombia, related to the existing structure for guaranteeing equitable supply.
Lack of coordination between dispensing pharmacies and insurance providers, affect accessibility. Results also indicate that, even when available, opioids are not accessible to many patients due to administrative barriers.
INTRODUCTION
The essential medicines concept developed by the World Health Organization (WHO) 1 states that there is a list of minimum medicines for a basic healthcare system, including the most efficacious, safe, and cost-effective ones for priority conditions. According to the WHO, essential medicines are those that meet primary healthcare needs of the population. Thus, they should always be available, affordable, and cost-effective. In spite of this, access to essential medications is an unachieved goal for millions of people around the world, especially those living in countries with less developed economies 2.
Strong opioids are a cornerstone of pain treatment. Of these, morphine, fentanyl, hydromorphone, methadone and oxycodone are included in the WHO Model List of essential medicines for pain relief and palliative care 3. However, an estimated 61 million of people live in low- and middle-income countries with severely limited access to essential medicines for pain relief and palliative care, especially oral immediate-release morphine. Approximately 50% of the global population - 3.6 billion people who reside in the poorest countries - receive less than 1% of the opioids distributed worldwide 4.
In Colombia, there are institutions and processes that provide a structure for the management of availability and accessibility of medicines, as an essential function of public health. In this framework (Figure 1), opioids are classified as either "state monopoly" or "non-state monopoly" medications. The steps to availability and accessibility of each are as follows:
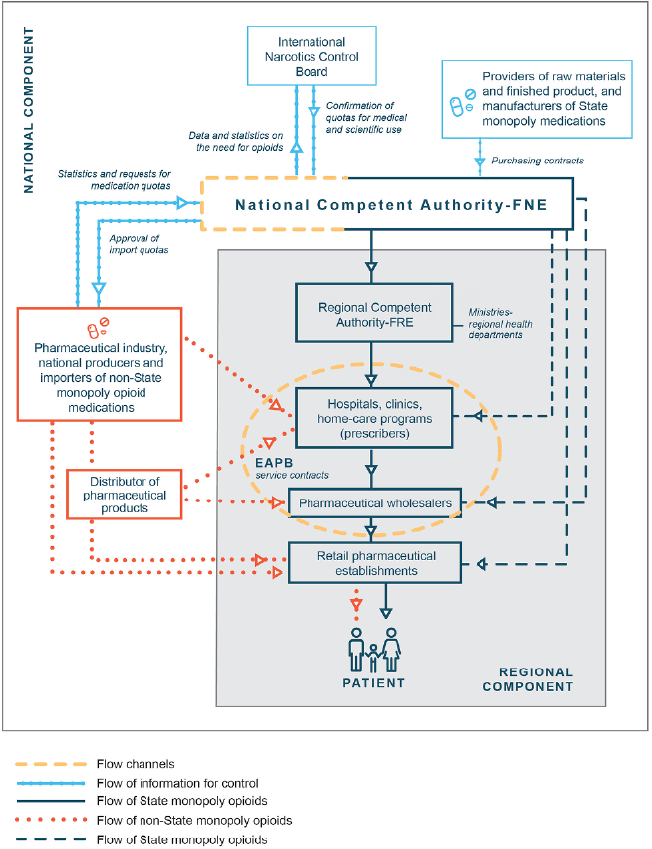
EAPB: Administrating Entities of benefit plans; FRE: Regulatory authorities/health departments; NNF: National Narcotics Fund. SOURCE: Authors.
FIGURE 1 Procurement and Distribution Monopoly and Non Monopoly Opioids
1) State monopoly opioids (MO): By decree, the government reserves the exclusive right to import, manufacture, distribute, and market generic hydromorphone, methadone, morphine and pethidine. The National Narcotics Fund (FNE for its Spanish acronym), a division of the Ministry of Health, is responsible for each of these steps as well as for monitoring and reporting. Once they are either manufactured locally or imported, the FNE stores the medications in a secure warehouse from which they are distributed to the 32 states of the country via different channels: a) to the corresponding regulatory authorities/health departments (FREs for Spanish acronym) in the 32 states; b) to hospitals and licensed clinics across the country (IPS for its Spanish acronym); c) to wholesalers; d) to insurance companies; and e) in Bogota (the capital), to a wholesaler which supplies a specific chain of retail pharmacies. To enable access, the FNE sells these generic medications at very low prices. All MOs are considered essential and are thus covered by the public health fund; therefore, whenever they are prescribed, patients have either to pay a minimal amount or nothing, depending on their income level.
2) Non-state monopoly opioids (NMO): Imported as branded products and sold by pharmaceutical companies. Pharmaceutical companies which have completed the necessary registration and licensing are allowed to import or manufacture, distribute and market commercially branded and patented opioid medications. Once manufactured locally or imported, the medications are distributed to the 32 states of the country via different channels: a) to hospitals and licensed clinics across the country (IPS); b) to distributors/ wholesalers; c) to pharmaceutical wholesalers; and d) to appropriately licensed retail pharmacies. For the purpose of this study, questions related to the following commercially branded opioids marketed by private companies were included in the survey: buprenorphine, codeine, fentanyl, hydrocodone, oxycodone, tapentadol and tramadol.
The FNE is the agency responsible for submitting the information on estimates and distributed amounts to the International Narcotics Control Board (INCB) for all controlled medications (MO and NMO) in the country. Pharmaceutical companies are required to submit to the FNE data on estimates and distributed opioids, based on the sales of their products. The annual reports of the INCB and data from the Colombian Palliative Care Observatory indicate that, over the past decade, there has been an increase in the distributed amount of opioid analgesics in the country, from 6.57 mg per capita in 2008 to 17.5 mg per capita in 2015 5,6. This includes both MO and NMO. This increase may reflect improved access for many patients, although this is still insufficient, according to recent reports7. Additionally, there are some periods of the year when shortages of raw materials or stockouts of opioid medications have occurred either at the FNE or any of the other distribution and dispensing entities. The goal of this study was to analyze the availability of opioids for the treatment of pain and for palliative care and identify barriers that interfere with appropriate access in Colombia.
METHOD
Cross-sectional study to identify availability of and accessibility to opioid medications in Colombia and the barriers affecting access. Data was collected using a survey distributed to prescribers. The design of the survey was based on a previous study which identified barriers to availability of and access to opioids in Colombia 8. Four coauthors developed the survey. A pilot test of the survey was carried out with 10 palliative care experts to identify difficulties and make improvements to facilitate proper understanding of the questions. Experts (defined for the purpose of this study as physicians with specialist training and more than 10 years of experience in the treatment of patients with pain and / or palliative care needs) were randomly selected from a list of specialists working in palliative care services.
An invitation to participate in the study was sent to the members of the Colombian Society of Anesthesiology (SCARE for its Spanish acronym) of the 33 administrative regions (states) that make up the Colombian territory. SCARE was selected as it is the largest association of physicians in the country and includes all specialties as well as General Practitioners (GPs). The survey was implemented from November 2017 to February 2018. Participation was voluntary and anonymous. Questions included sociodemographic information and perceived barriers to availability and accessibility.
For the purpose of analyzing the data, participants were divided in five regions: Amazon, Caribbean, Central, Northwestern, Orinoquia and Pacific, plus Bogota (the capital - 7MM). The barriers affecting availability were analyzed by facilities (for distribution and/or dispensing) and barriers affecting accessibility were analyzed by type. Descriptive analyses were conducted using relative frequencies for the categorical variables. To determine significance among regions and the categorical variables, a Fisher's exact test was used.
The study protocol was reviewed and approved by the Ethics Committee of Universidad de La Sabana in Bogota, Colombia (Reference MED225 of 2017).
RESULTS
Of the 1,208 prescribers in 28 states who responded to the invitation to participate, 806 completed the questionnaire (66.7% RR). Of these, 48% were general practitioners (GPs) while the remaining had completed either specialty or sub-specialty (Geriatric [22,9%], Anesthesia [14,4%], Internal Medicine [8,29%], Pediatrics [7,0%], Palliative Care [5,2%], Emergency Medicine [3,3%], Psychiatry [3,0%], and others). The average age of the participants was 38 years. Most respondents worked in inpatient services (70.2%) and outpatient services (22.5%). The remainder of the sample included home-care physicians (2.98%) and those working in other settings (4.22%). Over 78% of the prescribers reported treating >100 patients per month.
The regions with the largest number of participants represented in this study were Central (n=300) and Pacific (n=i08) plus the city of Bogota (n=216). Four states were not represented in the survey (Arauca, Guaviare, Vaupes, Vichada). Table 1 includes the list of regions, the corresponding states and the number of participants in each. Results are presented in two categories: Availability and Accessibility barriers, and within each, two subcategories (MO and NMO).
TABLE 1 Regions, states and number of participants.
| Region | States | Prescribers | |
|---|---|---|---|
| n | % | ||
| Amazon | Amazonas, Caqueta, Guainia, Putumayo | 10 | 1.2 |
| Bogota | Bogota D.C. | 216 | 26.8 |
| Caribbean | Atlantico, Bolivar, Cordoba, Guajira, Magdalena, San Andres y Providencia, Sucre | 69 | 8.6 |
| Central | Antioquia, Caldas, Huila, Quindio, Risaralda, Tolima | 300 | 37.2 |
| Northwest | Boyaca, Cesar, Norte de Santander, Santander | 71 | 8.8 |
| Orinoquia | Casanare, Cundinamarca, Meta | 32 | 4 |
| Pacific | Cauca, Choco, Nariño, Valle del Cauca | 108 | 13.4 |
| Total | 806 | 100 | |
SGURCE: Authors.
Availability barriers
Overall, 76.43% of participating physicians reported barriers to the availability of opioid medications. Table 2 presents the data for availability barriers by facility (for distribution and/or dispensing). Prescribers reported limited availability for MO (64.92%) and NMO (71.47%). In the case of MO, the facilities with barriers to availability most frequently cited were "Pharmacies authorized by health insurance companies," followed by hospital pharmacies and barriers at the FNE. The facilities with least reported barriers were the FREs. The facilities with barriers to availability most frequently cited for NMO, were "Pharmacies authorized by health insurance companies," where opioids are often unavailable for dispensing.
TABLE 2 Reported barriers on availability (for distribution and/or dispensing).
| Opioid type | Reported barriers | Frequency | Amazon (n=10) | Bogota (n=216) | Caribbean (n=69) | Central (n=300) | Northwest (n=71) | Orinoquia (n=32) | Pacific (n=108) | p value1 |
|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |||||
| Monopoly opioid medications | At pharmacies authorized by insurance companies | 341 | 33.3 | 75.9 | 65 | 68.9 | 71.4 | 71.4 | 80 | 0.16 |
| At hospital pharmacies | 336 | 50 | 72.2 | 82.5 | 66.1 | 83.3 | 71.4 | 68 | 0.14 | |
| At FNE | 178 | 33.3 | 28.7 | 47.5 | 43.2 | 35.7 | 33.3 | 33.3 | 0.19 | |
| At FREs | 98 | 0 | 16.7 | 10 | 25.1 | 26.2 | 9.5 | 22.7 | 0.15 | |
| Non-onopoly opioid medications | At pharmacies authorized by the insurance company | 428 | 60 | 85.3 | 78.3 | 82.6 | 73.3 | 90 | 84.9 | 0.34 |
| At retail pharmacies | 218 | 20 | 55 | 30.4 | 36.8 | 37.8 | 55 | 41.1 | 0.01 | |
| At hospital pharmacies | 263 | 80 | 41.1 | 56.5 | 55.7 | 60 | 45 | 43.8 | 0.04 |
n=Number of prescribers in each region. 1. Bold indicates p <0.05, statistically significant
SOURCE: Authors.
Regarding the availability of specific medications, fentanyl transdermal patches were reported as the most frequently available, followed by tapentadol tablets and oxycodone ampoules. The medications reported as being the least available were vials of oral morphine and morphine ampoules. There was a significant difference among the regions between retail pharmacies (p=0.01) and hospital pharmacies (p=0.04).
Accessibility barriers
Overall, 74.6% of participating physicians reported barriers to the accessibility of opioid medications. Table 3 presents the data for barriers to accessibility by type.
TABLA 3 Reported barriers to accessibility (by type).
| Opioid type | Reported barriers | Frequency | Amazon (n=10) | Bogota (n=216) | Caribbean (n=69) | Central (n=300) | Northwest (n=71) | Orinoquia (n=32) | Pacific (n=108) | P value1 |
|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |||||
| For monopoly opioid medications | Difficulty securing payment authorization from health insurance companies | 281 | 50 | 64.8 | 62.5 | 55.7 | 45.2 | 57.1 | 66.7 | 0.23 |
| Difficulties with medication dispensing | 212 | 333 | 40.7 | 35 | 50.8 | 35.7 | 57.1 | 42.7 | 0.24 | |
| Difficulties securing a new prescription | 215 | 333 | 51.9 | 37.5 | 50.3 | 45.2 | 28.6 | 333 | 0.07 | |
| Limited locations and operating times of dispensing pharmacies | 162 | 0 | 39.8 | 22.5 | 36.1 | 26.2 | 333 | 34.7 | 0.21 | |
| Cultural barriers | 150 | 16.7 | 333 | 17.5 | 32.2 | 42.9 | 28.6 | 30.7 | 0.33 | |
| Cost | 94 | 16.7 | 20.4 | 25 | 15.3 | 19 | 52.4 | 18.7 | 0.02 | |
| For non-monopoly opioid medications | Difficulty securing payment authorization from health insurance companies | 406 | 60 | 84,5 | 69,6 | 80,1 | 64,4 | 75 | 78,1 | 0,06 |
| Difficulties securing a new prescription | 235 | 0 | 46,5 | 34,8 | 51,2 | 48,9 | 40 | 35,6 | 0,07 | |
| Difficulties with medication dispensing | 205 | 20 | 35,7 | 37 | 41,3 | 44,4 | 55 | 37 | 0,64 | |
| Cost | 200 | 60 | 42,6 | 39,1 | 33,8 | 37,8 | 50 | 39,7 | 0,55 | |
| Limited locations and operating times of dispensing pharmacies | 162 | 20 | 36,4 | 19,6 | 31,8 | 24,4 | 35 | 31,5 | 0,42 | |
| Cultural barriers | 151 | 20 | 27 | 15 | 28 | 44 | 40 | 33 | 0,07 |
n=Number of prescribers in each region1. Bold indicates p <0.05, statistically significant
SOURCE: Authors.
The accessibility barriers for MO most frequently cited were "Difficulty securing payment authorization for medication from health insurance companies," "Difficulties securing a new prescription," "Difficulties having the medication dispensed," and "Limited locations and operating times of dispensing pharmacies." There was a significant difference among the regions for "Cost" (p=0.02). Accessibility barriers for NMOs most frequently cited, were "Difficulty securing payment authorization from health insurance companies," "Difficulties securing a new prescription," "Difficulties having the medication dispensed", and "Cost".
DISCUSSION
The mechanisms to ensure the availability of and accessibility to opioid medications are essential components of efficient health systems, and opioid medications are necessary for alleviating serious health-related suffering 4,9,10. Ensuring availability requires robust procurement and distribution systems, effective management and monitoring, as well as appropriate prescription and dispensing; this requires education of administrators and health professionals. The identification of barriers to availability and effective access to opioid analgesics is a priority for countries faced with challenges for achieving equity in health care 10.
Physicians in Colombia are authorized to prescribe controlled medications after they complete medical school and are not required to take additional training or courses in order to prescribe opioids. The large percentage of GPs in the prescriber group may reflect this prescribing privilege. The government has adopted several initiatives to improve access to medical care in rural and remote areas, and positions for GPs who are interested in taking active roles in the communities is a step towards better health care. The results of this study confirm frequent reports from pain and palliative care workers in Colombia stating that the availability of opioid medications in the country is inadequate 7,11-13. The analysis from this study also shows that reasons for limited availability of opioids which were identified in 2008, still persist to this day 8.
The results indicate that most of the barriers to opioid availability (both MO and NMO) are related to pharmacies authorized to dispense opioids by the different health insurance companies. There is often a lack of coordination among the agencies in charge of procuring and distributing the medications, affecting availability. At the regional level, there are problems associated with low interest of state health offices and governors in guaranteeing MO availability, which in turn results in no budget allocation for the procurement of the medications. For NMO, pharmaceutical companies have better procurement and distribution mechanisms in place, resulting in better availability of commercially, branded, albeit more expensive, formulations throughout the country.
Many years ago, the Colombian government adopted a law by which it reserves the exclusive right to import, manufacture, distribute, and market generic hydromorphone, methadone, morphine and pethidine, otherwise known as Monopoly Opioids (MO) 7. Although the primary intention of that law was to prevent diversion, it has had an important and positive impact on access as well. These medications are sold by the FNE at very low prices to the FREs which, in turn, sell them to hospitals and other licensed pharmacies. In addition, the government enacted a palliative care law and several regulations which call for opioid availability and accessibility for pain relief and palliative care 24 hours a day, seven days a week 14. However, if there is no political will at the state level, these generic, inexpensive medications are not made available, rendering the measures taken by the government ineffective.
Participants identified difficulty securing payment authorization from health insurance companies, limited number of pharmacies and their limited hours of operation, and difficulties securing a new prescription as the most frequent access barriers for both MO and NMO. For many patients, care is delayed and affected by a long and tedious authorization process. The availability barriers identified are similar to those described in published literature, including limited skills, knowledge and awareness among prescribers, restricted financial resources, supply problems, cultural attitudes, lack of political interest and trade controls 4,9,15-17. It is striking that the drugs reported as the least available were oral morphine vials and morphine ampoules, considering the importance given to morphine consumption for the development of palliative care, 18 the cost-effectiveness of its availability, and the regulations put in place in order to guarantee access in all regions and at all levels of care.
Those barriers affect not only medications but other treatments and interventions as well, which are many times resolved in court through the legal recourse of protection of fundamental rights in this case, access to medicines. This reflects a pervasive tension that exists in the country between the protection of the right to health on the one hand and, on the other, strengthening of a profit-oriented market 17,19. Some authors have argued that the pursuit of profitability leads to access barriers, especially in small towns and rural regions of the country 20. Other analyses on barriers to opioid access in palliative care 10,16,21 have identified opiophobia as the main cause of pain treatment barriers. However, factors related to the structure of the health system and the organizational barriers associated with prohibitionist opioid regulation must be considered, especially in rural areas with little access to medicines that are not included in national health plans. An action plan should be developed to reduce the problems associated with administrative formalities and their effect on effective access to medications for patients who require them.
A public health approach to access and availability of opioids should begin by recognizing the differences that exist within regions and how these conditions modify access to medicines. This work analyzes regional differences within a country, including social determinants in each geographic area, and opportunities for improving equity in health, particularly for people living in remote areas. Future areas of study relate to the benefits derived from the organization by opioid groups (MO and NMO) and its relationship with policies of access to essential medicines and health outcomes of the population.
This study has several limitations. The physicians who participated in the survey are members of the largest professional association in the country, with representatives from several fields and specialties. The Regions with the highest number of participants are those where the largest and most populated cities are located (Bogota, Medellin, Cali). Regions with less populated, large rural and farming areas, had less participants. In addition, no prescribers from four states (Arauca, Guaviare, Vaupes and Vichada) responded the invitation to participate in the survey, and thus are not represented in this study. These states rank the lowest in economic development, infrastructure and access to health. They also rank lowest in the reported consumption of opioids (6). It can be assumed that patients in rural, less developed areas, face additional or more severe challenges than those identified and described in this study. However, this aspect should be addressed in future research. Because of the uneven distribution of prescribers throughout the country (the vast majority are concentrated in regions where the largest cities are located), access barriers in areas with fewer participants represent the perception of physicians who work in these regions, without adjusting the estimates to the population, which could limit their comparability. Differences in access to opioids by care setting (hospital or outpatient facilities) and type of health insurance are identified as future areas of research.
CONCLUSIONS
Despite evidence of an increase in opioid use in Colombia, barriers to availability and accessibility still persist in the country. There are challenges in terms of securing payment authorization from health insurance companies, obtaining new prescriptions, and finding dispensing pharmacies that operate 24 hours a day, seven days a week, particularly for state monopoly opioids (hydromorphone, methadone, morphine and pethidine). Likewise, cultural and economic barriers hindering access to medications are identified. An important challenge for Colombian health systems in relation to access to opioids is to analyze the structure of distribution, availability and control of these medicines and the ability of national agencies to guarantee equitable supply, especially in less populated, rural or remote regions.
ETHICAL DISCLOSURES
Ethics committee approval
The study was reviewed and approved by the Ethics Committee of Universidad de La Sabana in Bogota, Colombia. Reference MED225-2017.
Protection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics commit-tee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).











 texto em
texto em 



