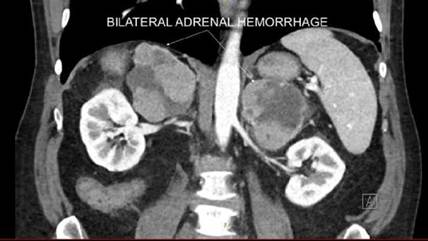
The accompanying image demonstrates hemorrhagic infarction of enlarged adrenal glands in a patient with coronavirus-disease-2019 (COVID-19) (Image 1). In addition to COVID-19, hypercoagulable states such as metastatic disease, heparin-induced-thrombocytopenia and antiphospholipid syndrome can precipitate adrenal hemorrhage.1 Although the mechanism remains unclear, it has been suggested that stress related increased adrenal arterial blood supply in conjunction with adrenal venous thrombosis may lead to capillary rupture and hemorrhagic infarction. Hypercoagulability in COVID-19 has been attributed to decreased fibrinolysis, vascular endothelial dysfunction and activation of procoagulant pathways by the virus induced inflammatory response.2 Bilateral adrenal venous thrombosis and hemorrhage, is an important consequence as it can precipitate adrenal crisis; a life-threatening medical emergency.3
Diagnosis necessitates a high index of suspicion as patients present with non-specific symptoms. Clinical features in awake patients include abdominal pain, fever, nausea, vomiting, hypotension and confusion. In mechanically ventilated and sedated patients, increasing hemodynamic instability and worsening metabolic acidosis may be suggestive. Acute glucocorticoid deficiency impairs action of angiotensin-II and norepinephrine leading to profound vasoplegia while mineralocorticoid deficiency precipitates hypovolemia. Presence of a high serum corticotrophin level, low serum cortisol, hyperkalemia, hyponatremia, hypoglycemia and sudden decrement in hemoglobin levels support the diagnosis. Radiological imaging including computed-tomography, ultrasonography and/or magnetic resonance imaging helps confirm presence of adrenal hemorrhage.
In critically ill patients with shock, differential diagnoses may include worsening sepsis, COVID-19 related cytokine-storm and propofol-infusion-syndrome especially in the context of prolonged propofol induced sedation (> 4 mg/kg/hr for > 48 hours). Treatment priorities include administration of intravenous hydrocortisone, isotonic fluid resuscitation, dextrose infusion to mitigate hypoglycemia and management of hyperkalemia. Hydrocortisone is preferred over other steroids for treatment in view of its dual glucocorticoid-mineralocorticoid action. Additionally, embolization of adrenal arteries may be required to control hemorrhage. Decision to commence anticoagulation, in the presence of adrenal hemorrhage, may necessitate consultation with a hematologist.











 texto en
texto en