INTRODUCTION
Severe asthma affects over 250 million people around the world and represents high healthcare costs 1,2. Severe asthma is defined as a condition that fails to respond to high doses of inhaled or systemic steroids, or long-acting bronchodilators 1. Interventional pulmonology has made significant progress in the management of this condition using bronchial thermoplasty 3. The procedure involves high frequency administration on the bronchial smooth muscle to reduce muscular hypertrophy, which improves airway resistance 1. The immediate complications associated with the procedure are mainly bronchoconstriction and increased secretions. There are other early complications that may present up to seven days post-procedure, including the exacerbation of asthma symptoms with coughing, dyspnea and secretions; infection, atelectasis due to mucus, bleeding and later on pulmonary abscess and pneumothorax.
Bronchial thermoplasty is done under general anesthesia, using intravenous and inhaled drugs 4-6. Patients undergoing the procedure are mostly ASA II and III, therefore there is a need to design a safe anesthesia plan to be able to conduct the procedure. The use of a laryngeal mask in procedures under general anesthesia allows for the controlled access to the airway, with minimum vocal chords stimulus, and its wide inner diameter facilitates ventilation with little restriction when introducing the flexible bronchoscope; hence, it is an alternative to orotracheal intubation during thermoplasty.
Thermoplasty is a relatively new procedure and there are few studies in our setting that have documented the complications of the procedure. The purpose of this study is to describe the immediate and early complications of bronchial thermoplasty conducted under multimodal anesthesia with laryngeal mask, at a high complexity institution.
MATERIALS AND METHODS
This retrospective case series selected all patients undergoing bronchial thermoplasty between 2014 and 2019. The medical record of the patients was reviewed, taking into account variables such as weight, sex, size, associated diseases, the patient's ASA classification, type of anesthesia and complications during and immediately after the procedure: hypotension (mean arterial pressure below 70 mm Hg), hypoxemia (oxygen saturation less than 88 %) and severe bronchospasm (non-responsive to inhaled β-agonists), as well as early complications (up to seven days post-procedure), and which required in-hospital management (for instance: asthma crisis, atelectasis, lung collapse). The proportion of complications of all the procedures performed was estimated. This study was reviewed and approved by the Research Ethics Committee of the Institution (Minutes No. CEI-431-2020).
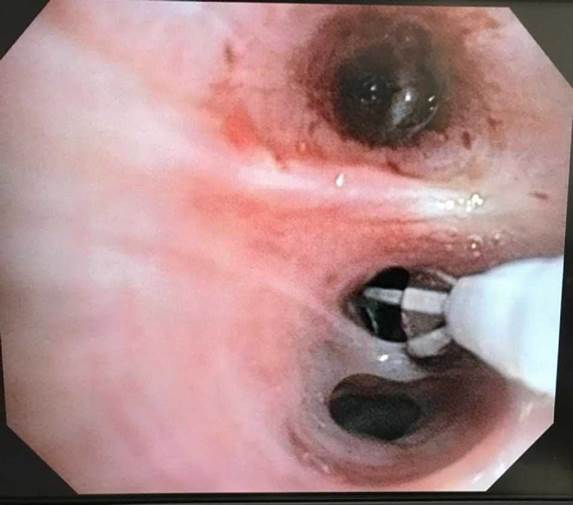
Thermoplasty was indicated by the treating pulmonologists in patients who remained symptomatic, despite the use of high-dose inhaled steroids and long-acting bronchodilators. The procedure was performed in three sessions, at least three weeks apart: the first session on the right inferior lobe; the second session on the lower left lobe; and the third session on the upper lobes on both sides. Each session systematically began from the most distal to the most proximal airway, pursuant to the international recommendations 7,8. Image 1 illustrates the bronchioles during the activity of the thermoplasty electrode.
On the day of the procedure, the patient was required to comply with the following requirements: not having received prednisolone over the last three days; oxygen saturation above 90 % on room air; not having experienced any asthma crises over the past 48 hours; being free from any active infections or reactivation of the allergic condition; and having signed the informed consent for the procedure.
Anesthetic procedure
The anesthesia process included non-invasive monitoring of vital signs (tensiometer, pulse oximeter, electrocardioscope, capnography) and the administration of prophylactic drugs 1 hour before the procedure: IV methylprednisolone 50 mg, nebulization with 4 to 8 inhalations of salbutamol and 0.6 mg intramuscular atropine. The induction of anesthesia was performed with IV xylocaine and propofol at 2 mg per kg of body weight and target controlled infusion (TCI) of remifentanil, at a dose-effect of 5 ng/mL and a maintenance period of anesthesia with TCI sevorane or propofol at a dose-effect of 2 µg/ml_, and remifentanil to reach a concentration in the effect site of 5 ng/mL. The selection of the maintenance drug was based on the opinion of the clinician and the anesthesiologist. The airway was managed with laryngeal mask and endotracheal topical anesthesia with xylocaine 0.5 cm3 per kg of body weight (9). Following the procedure, the patients were monitored in the recovery room for at least four hours, considering the risk of bronchospasm.
RESULTS
Table 1 summarizes some of the characteristics of the patients who underwent the procedure. All of them received multimodal anesthesia with laryngeal mask, and all the procedures were completed. There were no reports of hypoxemia or hypotension in any of the cases. Three of the patients presented some complication in the immediate postoperative period, in at least one of the sessions, for a total of 3/12 sessions with complications (25 %). None of the patients experienced any complications during the 7 days after the procedure.
TABLE 1 Characteristics of patients undergoing bronchial thermoplasty.
| Patient | Age (years) | Sex | BMI Category | Comorbidities | ASA | Smoking | Number of procedures | Number of procedures with complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 60 | F | Overweight | Hypertension | III | No | 3 | 0 |
| 2 | 37 | F | Overweight | Sleep apnea GERD} Cushing's syndrome |
II | No | 3 | 1 |
| 3 | 55 | M | Overweight | Osteoporosis | III | No | 3 | 1 |
| 4 | 54 | F | Overweight | Hypothyroidism | II | No | 3 | 1 |
BMI: Body Mass Index, GERD: Gastroesophageal reflux disease.
SOURCE: Authors.
Following is a description of some of the patient characteristics.
Patient 1
Patient with overweight, history of hypertension, cooks with firewood, and chronic sinusitis. Paucigranulocytic asthma phenotype, and management included tiotropium inhaler, salmeterol/fluticasone inhaler, montelukast, ipratropium bromide, salbutamol and intermittent prednisone. The patient received the three sessions of thermoplasty with no complications.
Patient 2
Morbidly obese patient with a history of Cushing's syndrome, hiatal hernia, gastroesophageal reflux, as well as multiple ICU admissions requiring orotracheal intubation. Eosinophilic asthma phenotype associated with obesity. The patient's management included formoterol, ipratropium bromide, tiotropium, montelukast and intermittent prednisone. The first two procedures were uneventful, the third one presented an episode of severe bronchospasm. Bronchodilator therapy was initiated in the recovery room with partial response; the patient was transferred to the ICU, did not require orotracheal intubation or mechanical ventilation, with satisfactory evolution and subsequent home management.
Patient 3
Patient with overweight and osteoporosis. Allergic phenotype asthma. The information of the medications the patient was taking were not recorded in the medical record. During the first procedure the patient experienced a moderate bronchospasm crisis and respiratory distress requiring management in the recovery room for 7 hours; then the patient was discharged home. The other two procedures developed uneventfully.
Patient 4
Obese patient with a history of hypothyroidism. Allergic phenotype asthma; management included tiotropium inhaler, salmeterol/fluticasone inhaler, montelukast, salbutamol, budesonide, ipratropium bromide and intermittent prednisone. This patient presented with laryngeal stridor and severe bronchospasm after the first procedure and had to be transferred to the emergency department where she was managed with inhalers and respiratory therapy for 12 hours and was subsequently discharged. In the rest of the procedures the patient experienced mild bronchospasm which was managed in the recovery room with inhaled therapy and was discharged for home in less than four hours.
DISCUSSION
In this case series, all thermoplasty sessions were conducted under general anesthesia, with laryngeal mask, with no complications during the procedure. In three of the twelve sessions there was at least one acute event of post-thermoplasty bronchospasm requiring in-hospital management and only one patient had to be admitted for management beyond 24 hours.
The safety and efficacy of the thermoplasty procedure has been assessed in a number of studies 2,4. The RISA clinical trial assessed the occurrence of adverse events and found that the most frequent were bronchospasm and coughing; most of them developed in the first day post-bronchoscopy and resolved in average one week later (9). In 2018, Aizawa et al. described in a case series the use of general anesthesia with good results 4. Thermoplasty is an option for patients with severe asthma; adequate selection of candidates is essential, in addition to a rigorous pre-anesthesia assessment, since most of these patients are ASA II y III. It should be highlighted that in all the procedures in this study, a laryngeal mask was used and there was no need for orotracheal intubation. This technique offered adequate manipulation of the bronchoscope and patient sedation, with no hypoxic events.
The use of the laryngeal mask in thermoplasty offers several advantages over orotracheal intubation. The largest internal diameter of the laryngeal mask facilitates the manipulation of the bronchoscope and since no muscle relaxants are used, spontaneous ventilation can be maintained. Whilst the use of muscle relaxants allows for improved airway control for induction and maintenance, in addition to improved precision for placement of the thermoplasty catheter 8, it also involves some disadvantages. For instance, the use of the depolarizing relaxant may cause myalgia and the non-depolarizing relaxant reversal agents may increase nausea, bradycardia and secretions 9. Furthermore, the use of the laryngeal mask also has some disadvantages to consider. Since it does not provide a total laryngeal seal, it may allow for the passage of gastric contents into the bronchopulmonary region, air leak or inhaled agent leaks into the environment, and prevents achieving high airway pressures.
The use of inhaled agents poses some theoretical disadvantages in the thermoplasty procedure, since the constant airway suction during the bronchoscopy hinders the determination of the concentration delivered to the patient, which increases the risk of an inadequate depth of anesthesia and contamination of the procedure room 10. The induction period may also be slower, with a higher incidence of coughing, tachycardia, and laryngospasm. However, considering that this was a case series, there was no randomized distribution of the anesthetic method and it is impossible to draw any conclusions in this regard.
One of the characteristics of the patients in this case series was overweight or obesity. Although the pathophysiology is unclear, some studies have shown that obesity affects the incidence and severity of asthma, increases bronchial hyperreactivity, increases up to five-fold the frequency of crises and exhibits worse treatment response 11. Additionally, obesity or overweight is a well-known risk factor for anesthetic complications. This makes the search for anesthesia strategies that minimize complications even more relevant, including intubation. Keeping in mind the limited sample size, our experience suggests that thermoplasty may be performed without the need for orotracheal intubation, using the technique herein described. Further studies are needed to confirm these findings, in addition to long-term follow-up of patients to describe the effectiveness of the procedure.
ETHICAL RESPONSIBILITIES
Endorsement of the ethics committee
This study was approved by the Ethics Committee of the institution, as shown under Minutes CEI-431-2020.
Human and Animal Protection
The authors declare that no experiments in humans or animals were conducted in this research. The authors declare that the procedures herein followed were pursuant to the ethical standards of the responsible human experimentation committee and pursuant to the World Medical Association and the Declaration of Helsinki.
ACKNOWLEDGEMENTS
Authors' contributions
- CFSB, IP and CEO: planning of the study, interpretation of the data, interpretation of the results, writing of the manuscript, and final version review.
- ÁMFT: planning of the study, data collection, interpretation of the results and writing of the manuscript and final version review.











 text in
text in