INTRODUCTION
SARS-CoV-2 infection is responsible for the current pandemic, which has claimed many lives worldwide 1 given its high level of contagiousness 2. Approximately 14% develop a serious disease that requires hospitalization and oxygen support 3; the most frequent diagnosis in severe patients is severe pneumonia with progression to Acute Respiratory Distress Syndrome (ARDS) in up to 30% of cases 4, which has required management with mechanical ventilation in intensive care units (ICU)5.
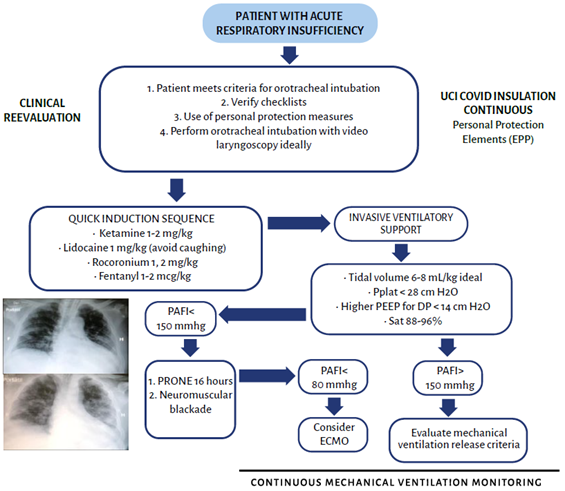
Severe SARS-CoV-2 disease was initially described in China6 where 1099 patients were identified, of whom a small percentage developed acute respiratory distress syndrome (ARDS), septic shock, and multiple organ failure. These patients were treated with invasive / non-invasive mechanical ventilation and extracorporeal membrane oxygenation (ECMO). The cohort study 7 evidenced a high burden of the disease and patients required ICU management because of their age (> 60 years), the presence of comorbidities such as hypertension (31.2% of the cases), cardiovascular disease (14.5%), diabetes (10.1%), inter alia. The SOFA SCORE indicated significant acute physiological dysfunction, with compromised pulmonary function with moderate to severe PAo2/ FIo2, according to the ARDS Berlin classification. However, the behavior of ARDS in SARS-CoV-2 patients is baffling (Image 1), and differs from the established definition. 8 The behavior is atypical by day 8 after the onset of the infection, and up to 50% of the cases exhibit normal pulmonary compliance, which has raised reasonable doubt as to whether we are dealing with atypical ARDS, which increasingly presents in younger patients 9-13.
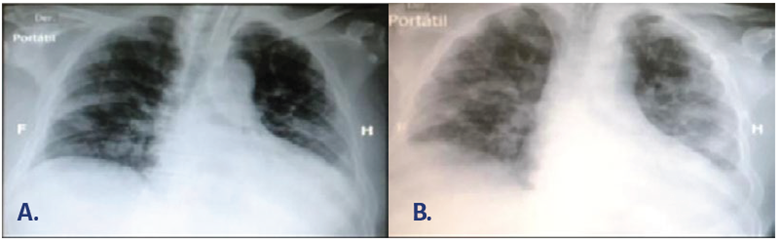
SOURCE: Authors.
IMAGE 1 Patients with acute hypoxemic respiratory failure confirmatory of SARS-CoV2- infection. A. L Phenotype. B. H Phenotype.
From the histopathological perspective, ARDS is a heterogeneous condition. 14,15 Diffuse alveolar damage during the organization phase has been described in the case of SARS-CoV-2 infection 16, in addition to micro and macro thrombosis phenomena associated with the respiratory process produced by the virus, leading to the pathophysiology of hypoxemia. This may also be related to the description of the phenotypes, multisystemic phenomena and proinflammatory processes probably associated with multi-organ dysfunction syndrome and fatal outcomes.17 Dr. Gattinoni describes 2 different phenotypes that may present dynamically in the same patient: a low phenotype, accounting for 70-80% of the cases, characterized by a low V / Q ratio, few opacities in the chest images, low lung weight, and low elastance / high compliance. The other less frequent high phenotype is exactly the opposite, characterized by right-to-left shunt, four-quadrant opacities on chest images - the so called "white lung" -, high elastance / low compliance, and high lung weight. Although the clinical behavior and the pathophysiological phenomena responsible for each phenotype are different, both may present with severe hypoxemia, hence requiring a different therapeutic approach.18,19
WHAT MECHANICAL VENTILATION STRATEGIES ARE AVAILABLE FOR SARS-COV-2 PATIENTS?
The SARS-CoV-2 infection is a new pathology, so the evidence is just being developed and there is not yet a correct therapeutic approach. The principles of mechanical ventilation are to improve gas exchange, decrease the patient's respiratory work, and buy time while re-establishing respiratory and systemic physiology. The decision to ventilate a patient will depend on multiple factors clinicians have to weigh at a certain point in time, such as ICU beds availability, the patient's prognostic factors, and his/her current clinical condition 20 (GRADE - Low level of evidence; conditioned recommendation). Patients with SARS-CoV-2 infection, and critically ill patients in general, experience a dynamic condition that may change abruptly; therefore, any interventions and decisions are constantly changing.
Non-invasive mechanical ventilation (NIV) and high flow nasal cannula (HFNC)
During a pandemic, additional strategies to invasive mechanical ventilation are described. 21 Non-invasive mechanical ventilation is not recommended in the management guidelines for patients with CoVID-19, who are hypoxemic and in respiratory failure, because of the high risk of transmission and particle dispersion22,23; however, a document based on the experience of the CoVID-19 outbreak in China highlights the use of non-invasive mechanical ventilation in patients with ARDS and PAo2/FIo2 > 150 mmHg. 24 This approach should be restricted to units where only suspected or confirmed patients with CoVID-19 are hospitalized, provided there is adequate ventilation or negative pressure, no interface leakage (a full-face mask is mandatory) and the staff in the area should use proper aerosol protection measures. When this is not possible, mechanical ventilation with orotracheal intubation should be preferred. 25
Some studies report the use of high flow cannula (60L/min) for patients with severe pneumonia, wearing a surgical mask over the interface to avoid aerosolization; some articles discuss the low risk of aerosolization and suggest its use in selected cases.26
Several literature reports indicate the use awake pronation in patients with mild to moderate ARDS, and the results have been encouraging in terms of improved oxygenation parameters and lower intubation rates27; however, the evidence to date is not conclusive to support these strategies for widespread management. What is clear is that patients who do not require intubation, should not be intubated early28, nor should intubation be delayed in those patients with the potential to develop complications.29
In some circumstances, HFNC and non-invasive NIV may fail, so early intubation should be considered: 24
Invasive mechanical ventilation
The indications for orotracheal intubation are the same as in patients with respiratory failure from other causes30; in particular, in the SARS-CoV2 patient the decision will depend to a large extent on his/her clinical symptoms. There have been cases of silent hypoxemia 31, rapid hypoxemia and refractory to management with high flow oxygen, without any additional manifestations. It is important to mention that one of the most relevant indications to initiate mechanical ventilation is increased respiratory work, since vigorous respiratory effort in a patient with an established lung injury may lead to the development of P-SILI (Patient-Self-Inflicted Lung Injury). 32
Consider tracheal intubation if the patient has:
Increased respiratory work
Tachypnea> 30 rpm persistent
Refractory hypoxemia: O2 saturation <90% despite supplemental oxygen (FiO2 ≥50%)
Acute respiratory failure
Shock criteria
An altered state of consciousness
If intubation is considered an option, it should be performed as soon as possible, otherwise the patient may experience a rapid decline. 24,33
Mechanical ventilation is not a therapy per se; it is considered a therapeutic strategy aimed at gaining time until the symptoms resolve, and it is part of the management armamentarium that includes conservative and individualized fluid strategy, the use of neuromuscular blockers, sedation, nutrition, glycemic control, steroid use, ECMO, and experimental drug therapies. 29 The use of an individualized mechanical ventilation strategy is recommended. 34,35 Dr. Gattinoni's study, recommends starting with an individualized mechanical ventilation strategy, according to the phenotype. The low phenotype may call for a tidal volume (TV) strategy of 8-9 mL / Kg of ideal weight, PEEP 8-10 cmH2O, use the prone rescue maneuver, use of hemodynamic and ventilatory monitoring, not forgetting those patients with low recruitment and oxygen saturation goals ranging between 92-96%. In contrast, the high phenotype could benefit from a TV 6 mL / Kg, PEEP > 10cmH2O, prone positioning is mandatory; these are patients with a high probability of recruitment and their lung involvement results in lower oxygen saturation, ranging from 88-92%. 18 These are simply some recommendations from the experts in the above-mentioned study, but the evidence is not strong enough. A study published in Lancet in 2019 concluded that the personalized mechanical ventilation strategy according to the type of ARDS, focal or diffuse, made no difference in mortality. Personalizing mechanical ventilation did not decrease mortality in ARDS, possibly due to the misclassification of 21% of the patients in this study. Therefore, further studies are needed in this area. 36 The management of ARDS in the patient with SARS-CoV-2 infection is extrapolated from the ARDS management guidelines for other causes37,38.
WHICH THERAPEUTIC STRATEGIES HAVE THE STRONGEST EVIDENCE IN COVID-19 ARDS PATIENTS ("CARDS")?
The knowledge of the ventilatory strategies for SARS-COV2 infection is mainly extrapolated from the accumulated evidence in ARDS.
Evidence-based treatment of SARS-COV2 infection is still in the works.
Protective mechanical ventilation
Protective mechanical ventilation is defined as ventilation in which the tidal volume is low, that is, 6 mL / Kg of ideal weight, to maintain a plateau pressure (Pplat) <28 cmH20 and a driving pressure (DP) <15 cmH2O 39, (GRADE; Strong recommendation; moderate level of evidence 1B), which impacts mortality in this clinical setting.40 The starting point should be 100% FIO2 and decrease every 20-30 minutes from 5 to 5%, monitoring the patient's clinical condition, avoiding hyperoxia due to the toxic and deleterious effect. 41,42 Tidal volume should be calculated based on ideal weight; the formula for men: 50 + 0.91 (size -152.4); and for women: 45.5 + 0.91 (size -152.4) 43
The goal of protective ventilation is not to correct the blood gas disorder but to lower the risk of ventilator-induced lung injury (VILI). Patients usually do not tolerate such low volumes, so in general, the use of sedation and neuromuscular blockers are necessary to avoid ventilator asynchrony, which can further impair lung damage.44 ventilator
The recommendation is to set the respiratory rate to 20-25 breaths / min, the inspiratory time in the volume-controlled mode should be 0.7 - 0.8 seconds to avoid decreasing the inspiratory flow since they are inversely proportional (Flow = Volume/ time); however, in the pressure-controlled mode it should be around 1 second to ensure that the alveolar pressure at the end of inspiration reaches the programmed pressure and a tidal volume of 6 ml / Kg is delivered, allowing adequate alveolar filling and emptying, taking into account the time constants, to avoid auto-PEEP45
Pressure- controlled versus volume-controlled ventilation
No differences have been reported between volume-controlled versus pressure-controlled mechanical ventilation. 46,47 In the setting of SARS-CoV-2 infection, mechanical ventilation monitoring is recommended to assess the best mode and ventilation strategy. 48,49 Given the need for mechanical ventilation monitoring, the volume-controlled mode with square or constant flow wave is preferable.
No differences were found between pressure-controlled and volume-controlled modes in terms of compliance, gas exchange, hemodynamic variables, respiratory work, mortality, or ICU stay in ventilated patients with acute respiratory distress syndrome 46.
The lack of large randomized trials in SARS-CoV-2 limits our knowledge to decide which ventilation mode should be used and the evidence is still evolving. Initially, patients with severe hypoxemia and average compliance caught our attention, and suggested different phenotypes. Later, as the disease progressed, its similarity to a typical acute respiratory distress syndrome was identified, with different mechanical characteristics explained by the natural course of the disease. The recommendation is to adhere to the scientific evidence showing good results in ARDS patients, providing protective ventilation and positive pressure at the end of individualized expiration regardless of the ventilation mode selected. 50
Considering that the literature does not report superiority of one ventilatory mode over the other, the decision should be made on the basis of different considerations, such as the patient's condition over the natural course of the disease and the specific characteristics of the respiratory system (which are dynamic); the experience of the healthcare staff with a particular mode of ventilation, allowing for appropriate patient-ventilator synchrony, until the lung recovers, with the least possible damage associated with invasive mechanical ventilation programming.
Prone position
Pronation is not recommended for every ARDS patient. The guidelines recommend the use of prone positioning for at least 12 hours per day in moderate/severe ARDS (Pao2/Fio2 <150 mmHg GRADE; Strong recommendation; moderate-high level of evidence 1A-B) 51
The PROSEVA study showed a reduction in mortality with pronation for 16 consecutive hours for 4 days, in moderate/severe ARDS. 52 Several meta-analyses support the pronation in this clinical setting, particularly for more than 12 hours and in association with protective mechanical ventilation strategies. 53,54
The substantial benefit should be considered in the context of the significant risk of occurrence of adverse events (endotracheal tube displacement, pressure ulcers, and loss of venous access), although the evidence was low or very low to support these findings.51
Prone therapy begins with a specific protocol, ideally from 12 to 16 hours and its continuity will depend on the patient's response. There is no standard time for the duration of pronation since the studies have different periods of duration ranging from 4 to 7 days. Others suggest discontinuation based on the response to the number of sessions, which are usually variable. 55,56 According to the literature a favorable response to prone positioning in the first few hours is a predictor for success, but initial non-response does not rule out success. 56
Prone positioning is discontinued in case of a favorable response defined as a PAO2/FIO2 > 150mmHg for at least 4 hours, in the supine position after the last prone session with PEEP < 10cmH2O and FIO2 <60%. 52 In the PROSEVA study, stopping prone therapy should be considered when the patient presents a deterioration in oxygenation (decrease in PAO2/FIO2 > 20% for the supine position if accidental extubation occurs, sustained decrease in oxygenation for 5 minutes (SatO2 < 85% or PaO2 < 55mmHg with FIO2 100 %), hemodynamic instability or cardiorespiratory arrest. 56 In the case of cardiorespiratory arrest in the prone position, there are no specific recommendations on cardiopulmonary-cerebral resuscitation, although some case reports indicate that it is possible to start in the prone position for the first cycles and then proceed to position the patient in the supine position to continue resuscitation 57.
The lack of large randomized trials in SARS-CoV-2 limits our knowledge about prone positioning. Some retrospective studies confirm the benefits of pronation in this subgroup of patients, but more evidence is required. 58-59
High peep versus low peep.
The lack of large randomized trials in SARS-CoV-2 restrict the knowledge of the PEEP. The evidence is of low quality to support the use of higher PEEP strategies in moderate or severe ARDS (conditioned). There are inconsistencies due to the differences in the results of the studies in terms of the heterogeneity of the strategy to establish the level of PEEP, while some trials compared lower tidal volume ventilation as part of a ventilator strategy that included lower levels high PEEP. The recommendation to consider higher PEEP in moderate ARDS is based on data from individual and subgroups of patients. The risk of barotrauma may not be ruled out because it has not been quantified in this population51. A recent study concluded that for ARDS patients who responded to increased PEEP with better oxygenation, hospital and ICU 28-day mortality could be reduced, without increasing the risk of clinically documented barotrauma. 60 The recommendation is to estimate the optimal PEEP to achieve the best compliance. 51 A new expert opinion document indicated that for patients with SARS-CoV-2, PEEP levels should be limited to 8-10 cmH2O, since higher levels will not increase pulmonary compliance and negatively impact the venous return, causing more harm than benefit. Bedside echocardiography may prove to be useful in assessing right heart function while managing PEEP increases.61
According to the Colombian ARDS consensus, the initial approach for PEEP should be guided by the PEEP / FIO2 table (GRADE; Strong recommendation; moderate level of evidence 1B). 62,63 Other titration methods for PEEP include the volume pressure curve, the best compliance, the stress index (=1), transpulmonary pressure, or image-guided (CT, ultrasound) best driving pressure. 61 The consensus suggests the use of driving pressure for PEEP titration (GRADE; Moderate level of evidence; weak recommendation 2B). PEEP should be neither too high (produces overdistension and increased dead space) nor too low (produces de-recruitment and atelectrauma). PEEP titration should avoid increases in plateau pressure, thus ensuring a decrease in driving pressure24.
If available, the use of volumetric capnography for PEEP titration is suggested in moderate to severe ARDS (GRADE; Low level of evidence; very weak recommendation 2C) 63 There is no conclusive evidence on volumetric capnography in COVID-19.
Recruitment maneuvers
There is limited knowledge about recruitment maneuvers due to the lack of large randomized trials in SARS-CoV-2. Alveolar recruitment maneuvers (ARM) should not be used in ARDS routinely (GRADE; Strong of Recommendation Against). 37 In cases of de-recruitment (due to endotracheal aspiration, disconnection) or refractory hypoxemia, despite optimizing therapy, alveolar recruitment maneuvers could be performed. 64 There are multiple alveolar recruitment maneuvers, however, the evidence indicates that there is no one maneuver that is superior to another. 65 Not all patients with ARDS are potentially recruitable or respond to recruitment, and this variability is due to various factors66, such as the cause of ARDS (higher in secondary ARDS or of extrapulmonary origin) 67, the evolutionary phase (early) 68, the position of the patient (higher in pronation, because of increased transpulmonary pressure in the dorsal region and improved gas exchange) 67, vasoactive management 69 changes in cardiac output and pulmonary blood flow distribution theoretically affect the response to the maneuver), thoracic expansion capacity (ineffective in patients with reduced thoracic expansion capacity), and previously programmed ventilator parameters 70,71 (low tidal volume, high PEEP; since ARM are likely to start from a recruited lung). The studies fail to establish specific criteria to define a positive ARM response. According to Grasso 68 maneuver responders are patients in which the PAO2/FIO2 increases at least 50% after the maneuvers, while Villagrá70 and Girgis72 define responders as patient with 20% increase in PAO2/FIO2 . Borges73 reports a positive response when PaO2 / FiO2 > 350, with a collapsed lung tissue mass of less than 5%. The studies define the response in terms of lung mechanics, analyzing the effect of the maneuver on parameters such as lung compliance. 66
The evidence in terms of improvement in clinical outcomes of ARM is controversial. A recent meta-analysis concluded that ARM could improve oxygenation but doesn't seem to improve survival65.
Lung recruitment in SARS-CoV-2 can be assessed at the bedside, even in very constrained environments. An observational study claims that lung recruitability was low in 12 patients with COVID-19 ARDS, and alternating body positioning improved recruitability. A new mechanics-based index to directly quantify the potential for lung recruitment is the recruitment-to-inflation ratio (R/I ratio) ranging from 0 to 2.0; the higher the R/I ratio, the higher the potential for lung recruitment. An R/I ratio of 1.0 suggests a high likelihood of recruitment. These findings do not imply that all patients with SARS-CoV-2-associated ARDS are poorly recruitable, and both the severity and management of these patients can differ remarkably according to the region.74
Clinicians in Wuhan decided to systematically use this recruitment measure in a series of patients with SARS-CoV-2-associated ARDS, and to assess the effect of body positioning. 74 Further randomized studies with larger samples are needed to define the best recruitment maneuver and the specific indications in this group of patients.
Neuromuscular blockers
The ACURASYS study75 showed improved mortality in ARDS with a PaO2 / FIO2 < 150 mmHg with the early use of a 48-hour infusion of cisatracurium and deep sedation versus deep sedation alone. The exact mechanism whereby neuromuscular blockade is beneficial is unclear. The lack of large, randomized trials in SARS-CoV-2 is a limitation to our understanding of neuromuscular blockers.
The ROSE study76 found that there was no significant difference in 90-day mortality between patients who received an early and continuous infusion of cisatracurium. The guidelines do not suggest the use of neuromuscular blockers for all patients with ARDS (GRADE: weakly recommendation against). The use of a 48-hour continuous infusion of cisatracurium besylate is suggested in early moderate/severe ARDS (PAO2/FIO2 <150 mmHg GRADE: weakly recommendation in favor)37. Neuromuscular blockers can decrease barotrauma and hospital stay. 77,78 A 2018 review79 found no difference between the different neuromuscular blocking agents vecuronium versus cisatracurium. Its use is particularly notable in patients with patient-ventilator asynchrony and PAO2/FIO2 <120mmHg80
A multicenter observational study of 407 patients with COVID-19 moderate to severe ARDS, found that NMBA were frequently used beyond the recommended period of time; however, after adjusting for confounders, there was no difference in the proportion of extubation rate according to NMBA length. 81
WHAT RESCUE STRATEGIES HAVE BEEN STUDIED?
Patients with ARDS under a strategy of protective mechanical ventilation may present hypercapnia, which has been identified as having an impact on the clinical outcomes of patients, increasing mortality. 82-85 The knowledge of the ventilatory strategies for SARS-COV2 infection is extrapolated from the accumulated evidence in ARDS. Management is individualized, the strategies may include increasing the volume or respiratory rate according to tolerance, and extracorporeal CO2 removal devices (ECCO2R) in the patient's clinical context86.
ECMO
Veno-venous extracorporeal membrane oxygenation is a rescue therapy in severe ARDS with potentially reversible hypoxemia, but refractory to conventional therapies. 37,87,88. The lack of large, randomized trials in SARS-CoV-2 limits the knowledge of ECMO.
The CESAR STUDY 89 concluded that ECMO therapy in experienced centers could improve survival without increased disability. A new EOLIA TRIAL90 was published in 2018, and their conclusion was that mortality was not significantly lower with ECMO than with a conventional mechanical ventilation strategy. A meta-analysis 87 comparing conventional mechanical ventilation versus venous-venous ECMO concluded that ECMO was associated with reduced 60-day mortality. However, venous-venous ECMO was also associated with a moderate risk of major bleeding. Particularly, in the SARS-CoV-2 infection scenario, the evidence is scarce, but the experience in previous pandemics has provided preliminary guidance for the use of ECMO and the recommendation is to indicate its use in selected patients with refractory hypoxemia and potential PAO2/FIO2 <80mmHg recovery, with no contraindications and in places with extensive ECMO experience.
Data from 213 hospitals worldwide, with 1035 patients with COVID-19 who received ECMO support, provide a generalizable estimate of ECMO mortality in the setting of COVID-19. The Extracorporeal Life Support Organization (ELSO) Registry concluded that in patients with COVID-19 who received ECMO, both estimated mortality 90 days after ECMO and mortality in those with a final disposition of death or discharge were less than 40%. 91
More studies are required to determine the risk-benefit of ECMO therapy in patients with severe SARS-Cov-2 infection.92
Extracorporeal CO2 removal
Extracorporeal CO2 removal devices (ECCO2R) allow CO2 to be extracted from venous blood by passing it through a membrane similar to that used in ECMO, but which uses much lower blood flow rates, and the arterial and venous cannulas are therefore smaller.93 The lack of large randomized trials in SARS-CoV-2 limits the knowledge of ECCO2T.
The Xtravent study 94 compared protective mechanical ventilation versus ultraprotective mechanical ventilation + ECCO2R. In a post hoc analysis of the subgroup of patients with PaO2 / FiO2 <150 mmHg, treatment with ultra-protective mechanical ventilation + ECCO2R was found to significantly reduce the number of days without mechanical ventilation. A systematic review 95 found no overall differences in mortality, days of ICU stay, or days without mechanical ventilation. According to the literature, the role of ECCO2R in clinical practice could be in the subgroup of patients with ARDS with PaO2 / FiO2 > 80mmHg and <150 mmHg, in which conventional support treatment and ventilation has been optimized to the maximum without response, and in those who are required to minimize pulmonary bloating and / or mitigate the effects of hypercapnia and acidosis.93 In the SARS-Cov-2 infection scenario, there is insufficient evidence available. There is currently a study in the recruitment phase, to investigate the efficacy of extracorporeal CO2 elimination for the correction of hypercapnia in ARDS associated with COVID-19 disease (SARS-CoV-2). The results from this study will provide new knowledge in this regard.96
A case report highlights the use of ECCO2R in severe ARDS and refractory hypercapnia associated with COVID19. Future studies are required to further investigate its safety and efficacy. 97,98
What is the evidence-based management and the most appropriate clinical approach?
The management of SARS-CoV-2 associated ARDS requires the expertise of the clinician and quick decision-making, with an individualized approach to ensure the best outcomes. 99 Different ventilatory approaches are needed, depending on the underlying physiology of the SARS-CoV2 infection.100
Table 1 summarizes the available evidence for the management of ARDS and SARS-Cov2 infection. A schematic approach to managing the patient with SARS-CoV-2 acute respiratory failure is described in Figure 1.
TABLE 1 Summary of evidence-based interventions.
| Intervention | ARDS severity | Grade evidence quality | Recommendation level | References |
|---|---|---|---|---|
| Lung protective ventilation | All patients with ARDS COVID-19* | Moderate | Strong | Aoyama et al 2019 39
*Marini et al 2020 100 |
| Prone position | ARDS Severe COVID-19* | Moderate-high | Strong | Guerin et al 2013 52
Fan et al 2017 54 *Elharrar et al 2020 58 *Weiss et al 2020 59 |
| High peep | Moderate-severe ARDS | Moderate | Conditioned | Guo et al 2018 60
Ortiz et al 2020 63 |
| Recruitment maneuvers | Moderate-severe ARDS COVID-19* | Low-Mode-rate | Conditioned | Furyk et al 2017 64
Kang et al 2019 65 *Pan C 2020 74 |
| Neuromuscular blockers | Severe ARDS COVID-19* | Moderate | Weak | Papazian 2010 75
PETAL STUDY 2019 76 Hua Y et al 2020 77 Zheng et al 2020 78 *Courcelle et al 2020 81 |
| Non-invasive mechanical ventilation and high flow cannula | Patients with mild respiratory failure in COVID19 | Low | Conditioned | Patel et al 2020 21 |
| ECMO | Severe ARDS COVID-19* | Does not apply | Does not apply | Munshi et al 2019 87
*Barbaro et al 2020 91 *Cho et al 2020 92 |
SOURCE: Adapted from Fan et al 54.
CONCLUSIONS
SARS-CoV-2 infection gives rise to a pathology of yet unknown clinical behavior, challenging the clinician in the context of the pandemic. ARDS exhibits heterogeneous clinical and histopathological characteristics and defy intensivists when implementing therapeutic strategies. Mechanical ventilation is part of the spectrum of therapeutic measures to "buy time" while the pathophysiological processes are normalized. A better understanding of the phenotypes and the underlying physiology is needed to help define ventilator parameters.
Evidence-based treatment of SARS-CoV-2 infection is still in the works; however, our knowledge from past experience favors a step-wise management approach, without neglecting other joint therapeutic measures to improve the clinical results of a condition with a high risk of mortality.
The current recommendations indicate that patients with severe acute respiratory failure due to SARS-CoV-2 should be managed with protective mechanical ventilation measures. No strong evidence is yet available on the individualization of mechanical ventilation therapy according to phenotypes.
ACKNOWLEDGMENTS
Author Contributions
DAR: Study concept and design, Acquisition, analysis and interpretation of data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Original material and construction of images and tables, Administrative, technical, and material support, Study supervision.
BDGP: Acquisition, analysis and interpretation of data, Drafting of the manuscript, Study supervision.
GS: Study concept and design, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Original material and construction of images and tables, Study supervision.
JFGG: Study concept and design, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Original material and construction of images and tables, Administrative, technical, and material support, Study supervision.
DREP: Study concept and design, Study supervision.
JCGM: Study concept and design, Critical revision of the manuscript for important intellectual content, Original material and construction of images and tables, Study supervision.
MAF: Acquisition, analysis and interpretation of data, Drafting of the manuscript, Administrative, technical, and material support, Study supervision, English translation.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.











 text in
text in