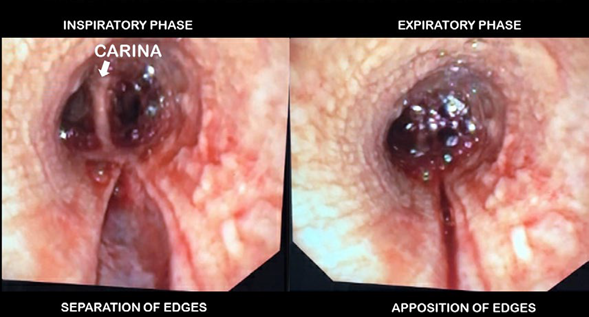
Iatrogenic tracheal injuries including submucosal tears, are more likely to occur during emergent endotracheal intubations. 1,3 Tracheal inflammation, elderly status and female sex are additional risk factors. The accompanying images are from a 70-year-old woman with Wegener's Granulomatosis who was emergently intubated in view of bowel-perforation. Delivery of positive-pressure-ventilation proximal to the tear was pressurizing the injury, leading to separation of wound margins during inhalation and apposition during exhalation (Image A). As this increased her risk of developing complete tracheal wall rupture, the existing endotracheal-tube was exchanged for a 6mm-microlaryngeal-tube with the aid of an airway-exchange-catheter and then maneuvered into the left-mainstem-bronchus under bronchoscopic guidance (Image B left). Pre-existing right-mainstem-bronchial stenosis due to Wegener's Granulomatosis necessitated placement of a 5mmmicrolaryngeal-tube. Bronchial stenosis obviated the need for cuff inflation (Image B right).
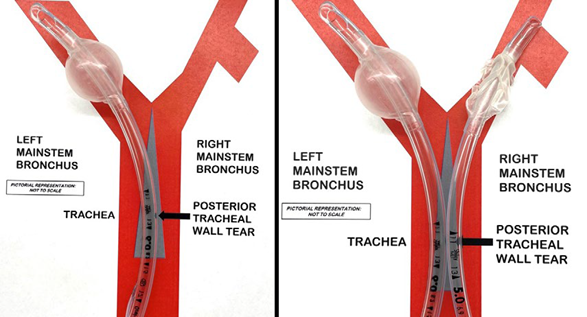
IMACE B Placement of two separate microlaryngeal tubes helps prevent pressurizing the distal tracheal submucosal injury.
Post-intubation development of subcutaneous emphysema, pneumothorax, pneumomediastinum or bloody tracheal secretions should prompt a bronchoscopy to rule out iatrogenic tracheal wall injury. Failure to recognize a submucosal tracheal tear and delivery of positive-pressure-ventilation proximal to the tear, can precipitate complete wall rupture and a 'cannot ventilate, cannot oxygenate" circumstance.
When positive-pressure-ventilation is desired for surgery completion in patients with proximal submucosal tears, the endotracheal-tube cuff is positioned distal to the tear and proximal to the carina. This allows for delivery of positive-pressure-ventilation without disrupting the tear.1,2 Presence of distal tracheal injury precludes this approach and may necessitate placement of 2 separate microlaryngeal-tubes as shown in Image B.
Early consultation with interventional pulmonologists is prudent as it helps in determining need for airway stenting and/ or surgical repair. In clinically stable patients with submucosal tracheal tears, return to spontaneous ventilation is encouraged as negative-intrathoracic-pressure maintains apposition of the edges of the tracheal tear, minimizing further injury.1-3 Employing a remifentanil infusion to minimize coughing during emergence and extubation may help mitigate additional stress on the membranous tear.











 text in
text in