What do we know about this topic?
• General anesthesia can be administered using two different techniques: balanced anesthesia with halogenated drugs, and total intravenous anesthesia.
• Both techniques provide adequate perioperative conditions and in non-cardiac and non-oncologic surgical models, clinically significant outcomes are similar.
• These techniques require resources, supplies and medical technologies, which points to a differential cost between the two types of techniques. This might result in decisions to use either of the techniques on the basis of the cost alone, without taking into account potential events associated with their use.
What is new about this study?
Although the cost of one technique may be higher, in particular when TCI technologies are used, compared to techniques based on anesthetic gases, this cost is offset by a shorter stay in the postanesthesia care unit (PACU) because of a lower risk of postoperative nausea and vomiting (PONV).
INTRODUCTION
Procedures that have had a significant impact in the setting of the perioperative care of patients taken to surgery have emerged in recent years, improving the quality of care and important clinical outcomes and, consequently, the cost of care 1,2.
It is estimated that close to 402 million procedures are performed under anesthesia every year. In 2015 in Colombia alone, 27,385 procedures were carried out under general anesthesia for every 100,000 inhabitants 3, with the techniques most widely used being inhalational and total intravenous anesthesia. Balanced anesthesia with halogenated drugs consists of the administration of anesthetic gases through a respiratory circuit plus the intravenous administration of an opioid drug during the entire procedure. In contrast, total intravenous anesthesia (TIVA) consists of the intravenous administration of only hypnotics (propofol) and opioids.
In Colombia, according to the latest national survey on anesthetic techniques conducted in 2017, the generalized use of inhalational anesthesia was placed at 58.1% as compared with TIVA which accounted for 30.9% of all general anesthesias administered in the country 4.
In general, multiple studies have documented the results of TIVA over those of inhalational techniques, with no consistent clinical outcomes found between the two techniques in the general, non-oncologic surgical population 5-14. In 2018, Schraang et al. 5 carried out the largest systematic review and meta-analysis ever conducted up to that date, which included more than 200 clinical trials comparing the two anesthetic techniques, and found no clinically or statistically significant differences for the most important outcomes in surgery, except for the lower impact on the risk of postoperative nausea and vomiting (PONV).
However, no strong literature is available on the topic of cost-effectiveness of these technologies in the different surgical settings; the few cost reduction studies were conducted more than 15 years ago and do not assess the impact of the implementation of these techniques on the health systems of the countries where they were conducted 6-14.
In Colombia, this absence of information and pressures for decision-making regarding the introduction of new anesthesia technologies, call for economic studies designed to identify which of the two anesthetic techniques can have the lowest impact on the cost of surgical patient care.
The objective of this study was to determine expected costs based on a case study on the use of an inhalational anesthetic technique versus intravenous anesthetic drugs in adult patients taken to non-cardiac and non-oncologic surgery under general anesthesia.
MATERIALS AND METHODS
Analytical model
A cost minimization analysis from the perspective of the Colombian health system was performed. The population included adult patients taken to non-cardiac and non-oncologic surgery under general anesthesia. The time horizon adopted was the length of stay in the post-anesthesia care unit (PACU) or 6 hours of the immediate postoperative period. This time frame was selected given that this study focused on anesthesia-related costs and not on secondary postoperative outcomes. The options considered were inhalational balanced anesthesia with opioids like remifentanil and total intravenous anesthesia with propofol and remifentanil. In view of this short time horizon, no discount rate was applied.
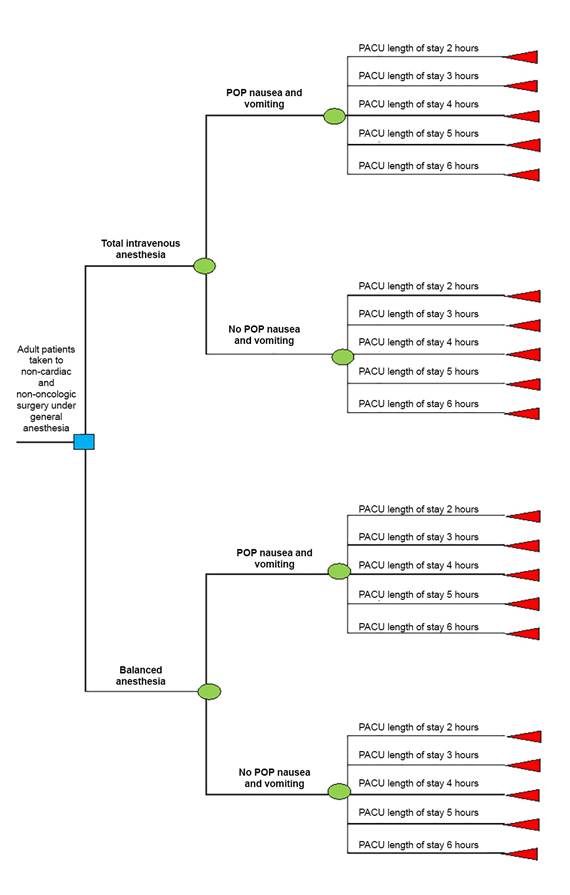
Given the lack of strong evidence in favor of one technique over the other in most surgical models, and given that primary clinical outcomes are not different between the two techniques, the study was designed to assess only the costs related to the use of both techniques. Consequently, for cost estimation, a decision tree was built of the potential pathways for a patient undergoing an anesthetic procedure, in accordance with differential events between both techniques: presence or absence of postoperative nausea and vomiting, and the length of stay in the PACU until discharge. This analysis option led to the creation of a logical structure to approach the problem and to incorporate the evidence of the options under assessment, in order to compare between them (Figure 1).
Transition probabilities
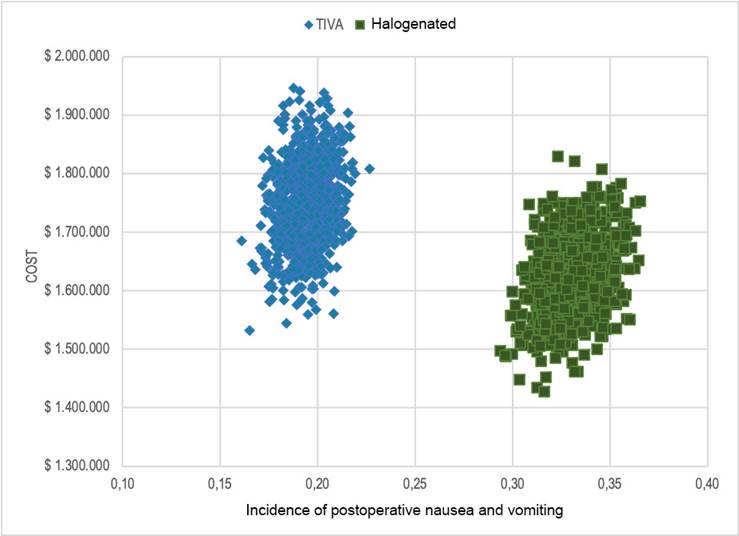
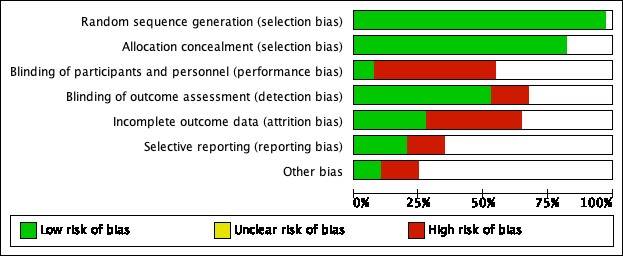
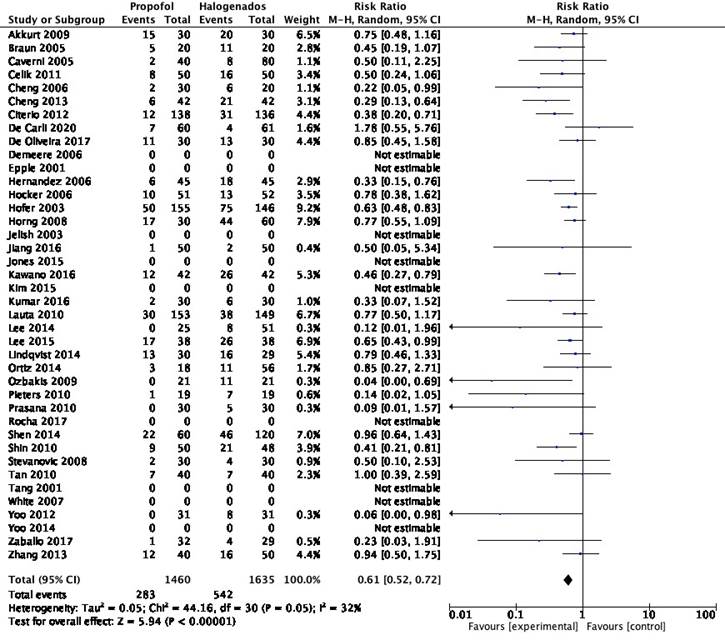
Transition probabilities were derived from a systematic literature review and meta-analysis carried out by the author of this study, analyzing clinical trials found in the most important databases: Medline, Embase and Cochrane Library. The study flowchart, bias analysis and meta-analysis for the risk of PONV are found in the supplemental content.
Based on this review and the meta-analysis that followed, it was found that the risk of PONV in TIVA and inhalational techniques was 0.61, 95% CI [0.52-0.72].
This means that the intravenous technique reduces the risk of this event by 39% as compared with the inhalational technique. The result was consistent regardless of the type of halogenated gases used, the type of surgical intervention or the setting (outpatient or inpatient) (supplemental content).
To determine length of stay in the PACU according to the presence or absence of PONV, the evidence of the clinical trials included in the aforementioned systematic review was analyzed. However, determining length of stay when the groups were divided according to the presence or absence of the PONV event was not possible. This led to a new literature review which found only one large cohort study that evaluated clinical outcomes according to the presence of PONV 15. This was a prospective cohort study that used matching techniques and different surgical models to evaluate not only the time to anesthetic recovery but also the economic costs associated with the presence or absence of PONV. Given that the study was methodologically well conducted and used prospective measurements and comparison with a low risk of bias to assess the economic impact of this event in particular, the PACU length of stay data from that study were used for this one.
Table 1 shows the probability of occurrence of the events modeled in the decision tree, based on the methodological recommendations contained in the economic evaluation manual of the Health Economic Evaluation Institute (IETS) 16 and the recommendations of Gidwai et al. 17 for converting event risks into probability of occurrence of an event based on the meta-analysis carried out by the author for the presence or absence of PONV. It also shows length of stay in the PACU, which was categorized by hours -between 2 and 6 hours of the time horizon. This choice was based on two factors: ease to determine probabilities in terms of 60-minute intervals, and cost of care for patients in the PACU estimated in terms of hours of stay and not in minutes.
Table 1 Parameters (probabilities) included in the decision tree.
| Parameter | Expected value | Sensitivity analysisa | |
|---|---|---|---|
| Minimum | Maximum | ||
| Inhalational anesthesia | |||
| PONV | 0.3315 | 0.3035 | 0.3595 |
| NoPONV | 0.6685 | 0.6405 | 0.6965 |
| Intravenous anesthesia | |||
| PONV | 0.1948 | 0.1745 | 0.2151 |
| NoPONV | 0.8052 | 0.7849 | 0.8255 |
| PACU Length of stay and PONV | |||
| 2 hours | 0.0577 | 0.037 | 0.078 |
| 3 hours | 0.1732 | 0.1412 | 0.2102 |
| 4 hours | 0.3016 | 0.2622 | 0.3403 |
| 5 hours | 0.2832 | 0.2434 | 0.3217 |
| 6 hours | 0.1842 | 0.1535 | 0.2211 |
| PACU Length of stay and no PONV | |||
| 2 hours | 0.1663 | 0.1346 | 0.2018 |
| 3 hours | 0.4016 | 0.3641 | 0.4436 |
| 4 hours | 0.3372 | 0.303 | 0.3821 |
| 5 hours | 0.0878 | 0.0616 | 0.1123 |
| 6 hours | 0.0072 | 0.002 | 0.0233 |
a. Minimum and maximum probability data come from the different 95% confidence intervals for the different estimators. PONV: postoperative nausea and vomiting. Source: Author
Costs
Direct medical cost calculations for each intervention started with the identification, measurement and quantification of consumed expenditure-generating resources. Two costing strategies were used: construction of a case study, and microcosting. The case study was built on the basis of the most widely reported clinical characteristics and surgical model in the clinical studies assessed as part of this study: 40-year-old patient weighing 70 kg, 168 cm tall, taken to laparoscopic cholecystectomy and 2 hours of surgical time. The case was validated by consensus of the three anesthetists with expertise in both techniques. The case assumption was that anesthetic consumption is directly proportional to surgical time in both interventions and that fixed surgical costs are similar in both techniques.
Following their identification, costs were divided into two large groups. The first included fixed costs related to operating room fees, medical fees, surgical material and length of stay in the PACU. The recommendation of the IETS methodological manual was applied for cost quantification and measurement 16, leading to the use of the 2001 rates schedule of the Social Security Institute (ISS), applying a 30% adjustment for 2012; the average consumer price index (CPI) reported by the Colombian National Statistics Department (DANE) for the past 5 years was used to make the 2020 adjustment. A 25% and 45% of the ISS value were used as the minimum and maximum values, respectively.
The other group consisted of variable costs, represented by medications, supplies and technologies used. For identification and quantification, the consensus of three anesthetists with expertise in the management of these techniques, and anesthetic simulators were used: the Gasman® software for the halogenated group 18 and the Rugloop® for TIVA, with the clinical parameters of the case study and the recommendations of the World Federation of Societies of Anesthesiology 2019 (WFSA) 19 for the administration, monitoring and surveillance of the TIVA technique. Medication cost estimates were taken from the Medication Price Information System (SISMED) for the 2020 period. Weightings of the prices for each medication were derived in accordance with the market share, and minimum and maximum prices were obtained for the doses used in the case study. The microcosting strategy was used for measurement and quantification of supplies and technologies for anesthesia administration, using market rates, in which two hospitals in Medellín were included: IPS Universitaria Universidad de Antioquia and Hospital Universitario San Vicente Fundacion. They were included because they are referral centers in the region and have experience with the techniques selected for the analysis.
Econometric model
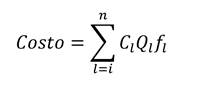
Variable cost weightings for each technique (medications, supplies and technologies) were determined in accordance with the frequency of use of these resources. The frequency was queried and validated by the team of three expert anesthetists. The formula recommended by IETS was used for the final calculation 16:
Where, n is the number of resources used, Cl is the cost of the i-th procedure, Ql is the i-th quantity of consumed resources; and fi is the frequency of use of the i-th expenditure-generating resource.
Uncertainty analysis
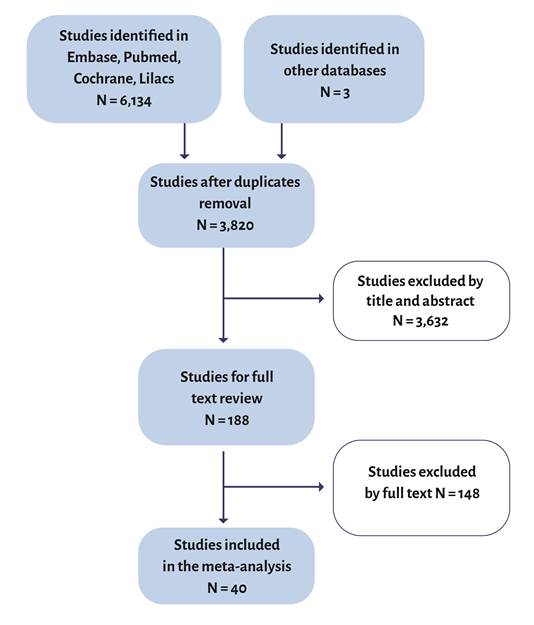
Both deterministic as well as probabilistic sensitivity analyses were carried out. In the deterministic analysis, costs were modified according to the confidence intervals for PONV incidences and PACU length of stay probabilities, as well as the surgical intervention setting: medium and high complexity. Moreover, the setting where the intravenous technique was not carried out using TCI systems but conventional volumetric infusion equipment was also evaluated. The results are shown in a tornado diagram (Figure 2).
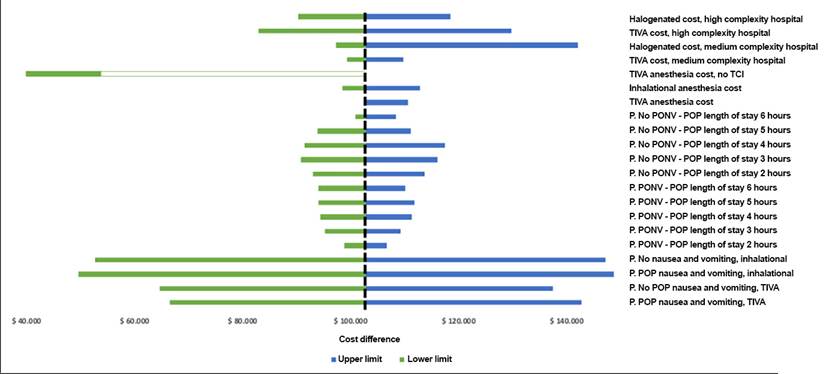
P: probability; PONV: postoperative nausea and vomiting; TCI: target controlled infution; TIVA: total intravenous anesthesia. Source: Author.
Table 2 Tornado diagram: deterministic analysis
A β distribution was assumed for PONV probabilities, with n and N parameters for the construction of the probabilistic analysis. For costs, a y distribution was generated taking the a and (3 values of the costs of each anesthetic intervention. The impact of PONV incidence on the cost of each intervention was analyzed by means of 1,000 Monte Carlo simulations.
Moreover, the incremental cost effectiveness ratio of the TIVA technique to reduce at least one PONV episode was determined by means of the difference ratios between the incidence of PONV and the net cost of both anesthetic techniques, without including the costs associated with the management of PONV and PACU length of stay.
The Microsoft® Excel 2020 software was used for the construction of the decision tree and costing of each intervention. All costs are in Colombian pesos. From the ethical point of view, this study did not use patient data directly and was classified as a low risk study in accordance with the current national regulations.
RESULTS
For the proposed case study, the cost of intravenous anesthesia is $1,811,218, whereas the cost of the inhalational technique is $1,708,500, with an incremental cost per patient receiving TIVA of $102,718. Table 2 shows costs according to each intervention, length of stay in the PACU, and the care level where the procedure is performed.
Table 2 Costs of each intervention.
| PACU length of stay | 2 hours PACU ($) | 3 hours PACU ($) | 4 hours PACU ($) | 5 hours PACU ($) | 6 hours PACU ($) |
|---|---|---|---|---|---|
| Medium complexity hospitals | |||||
| Inhalational | |||||
| Minimum | 1,405,731 | 1,468,542 | 1,531,353 | 1,594,164 | 1,656,974 |
| Base Case | 1,547,254 | 1,615,806 | 1,684,357 | 1,752,909 | 1,821,461 |
| Maximum | 1,619,992 | 1,692,075 | 1,764,159 | 1,836,242 | 1,908,325 |
| TIVA | |||||
| Minimum | 1,508,173 | 1,570,983 | 1,633,794 | 1,696,605 | 1,759,416 |
| Base Case | 1,654,879 | 1,723,430 | 1,791,982 | 1,860,534 | 1,929,085 |
| Maximum | 1,730,590 | 1,802,673 | 1,874,756 | 1,946,839 | 2,018,923 |
| High complexity hospitals | |||||
| Inhalational | |||||
| Minimum | 1,431,064 | 1,506,542 | 1,582,019 | 1,657,496 | 1,732,974 |
| Base Case | 1,574,903 | 1,657,278 | 1,739,654 | 1,822,030 | 1,904,406 |
| Maximum | 1,626,780 | 1,702,258 | 1,777,735 | 1,853,212 | 1,928,690 |
| TIVA | |||||
| Minimum | 1,533,506 | 1,608,983 | 1,684,460 | 1,759,938 | 1,835,415 |
| Base Case | 1,682,527 | 1,764,903 | 1,847,279 | 1,929,655 | 2,012,031 |
| Maximum | 1,759,663 | 1,846,282 | 1,932,902 | 2,019,522 | 2,106,141 |
PACU: postanesthesia care unit; TIVA: total intravenous anesthesia.
Source: Author.
For the deterministic analysis, it was found that the main variable than can impact cost differences between the two techniques is the risk of PONV; therefore, the increased incidence of PONV has a direct impact on the increased cost of care in both interventions. Additionally, it was found that more than 50% of the cost difference in favor of inhalational techniques is explained by the use of TCI technologies in TIVA interventions (Figure 2).
However, the probabilistic analyses found that, in the majority of the simulations, cost differences can be nil when the PONV risk difference between both techniques is large, as happens with the base case (Figure 3).
The incremental cost-effectiveness ratio between TIVA and balanced anesthesia for PONV was $7,687; this means that $7,687 are needed to avoid at least one additional PONV episode when TIVA is used, as compared with inhalational anesthesia.
DISCUSSION
Perioperative management of patients taken to surgery requires the administration of an anesthetic technique that allows to perform the surgical procedure. General anesthesia techniques are traditionally the most widely used to achieve this objective and, among them, inhalational and intravenous techniques are the most common. A recurrent concern among healthcare providers is how to reduce costs and improve efficiency in activities that have a high impact on the expenses of the healthcare organization and, therefore, on the health system itself, as is the case of surgical procedures. From this perspective, one of the most frequent questions in anesthetic practice is, precisely, which of the two anesthetic techniques can have a lower cost in perioperative care, given the belief that an intravenous drug-based technique can result in a higher cost because it requires a greater use of devices and technologies as compared to techniques based on anesthetic gases 4. In fact, this argument has been used to create a barrier to the implementation of a highly versatile anesthesia technique, particularly in elective outpatient procedures.
The aim of this study was to determine and compare the expected cost of administering these two anesthetic techniques, based on the fact that both are highly effective and are associated with a similar risk of anesthesia-related complications. This led to the performance of a cost minimization study.
The results of this study show that the mean incremental cost difference between the two anesthetic techniques is $102,718 for every patient taken to non-cardiac, non-oncologic surgery.
When uncertainty analyses are used to contextualize this result, cost differences for both techniques vary according to the risk of PONV occurrence, where the higher the risk of PONV the greater the cost difference between both techniques, while the lower the risk or probability of PONV in both groups, the more significant the reduction of the cost difference between the two.
However, the stochastic analysis found that, despite high consistency in the incidence of PONV, the variation of the costs associated with each anesthetic technique is very similar between the two. This even results in the cost difference of the interventions analyzed being nil in more than 50% of the simulations, and when the difference in the risk of PONV increases.
It is worth noting that though it is clear that the intravenous technique is potentially cost-effective for the prevention of PONV, with an incremental cost-effectiveness ratio of $7,787, the final cost of the intervention is determined by the time spent in the PACU as a result of this event. This finally explains why, although it is a more costly technique, the additional cost incurred with TIVA administration is offset, in the long run, by the cost savings from shorter length of stay in the PACU, as observed in the analytical model used in this study. Additionally, it was found that no major differences exist between the cost of the interventions when they are carried out in medium and high complexity centers.
Another relevant finding in this analysis was the ability of the target controlled infusion (TCI) systems to substantially affect the cost difference between the two techniques. If the cost of the TCI systems were to be eliminated in TIVA, the cost difference between both techniques would be almost 60% lower. In this regard, it is expected that as the cost of this type of system drops, not only would the use of this technique grow but the cost could be substantially lower than those of generic, inhalational anesthetic techniques.
These results are in stark contrast with the cost reduction studies nested in four clinical trials. To date, there are only four cost minimization studies published on this topic, all of them carried out more than a decade ago 10-13. The four studies not only specify the econometric models applied, but they also report high cost differences between the study techniques in favor of halogenated gases. This can be explained because the introduction of the technologies required for intravenous anesthesia administration and neuromonitoring became massively available only 20 years ago. This resulted in the substantially higher cost of intravenous techniques as compared to inhalational techniques. However, complete economic studies have not be conducted in other countries to allow for direct or indirect cost comparisons between anesthetic techniques or that can serve as a comparison reference with the results reported in these studies.
The probabilities on which the decision model was built are based on controlled clinical studies where the anesthetic techniques, the baseline risks and the prevention of PONV were completely controlled. Therefore, it is probable that this event could be under or overestimated according to individual patient characteristics and the surgical intervention.
There are no national studies to help determine with certainty the average time a patient remains in the PACU and how this time is impacted by the different events affecting recovery. This variable can eventually influence the final cost of one technique over the other.
The model on which the case study was built is based on the assumption that anesthetic administration occurs under the highest standards and in accordance with the relevant recommendations. In that regard, this model does not assess the variability caused by differential administration in terms of dosing, anesthetic drugs and technique used by the different anesthetists. Similarly, the anesthetic quantification for the case was derived from anesthetic simulators because they provided a better approximation of the anesthetic volumes used; however, they may lose accuracy when clinical and technical variables which are not controlled by those simulators are applied.
Costing of anesthetic procedures in Colombia poses a major challenge for several reasons: specific anesthetic rate schedules created by scientific societies (like the Schedule of the Anesthesiology Society of Antioquia) are not a regular part of the service agreements between Benefit Plan Management Organizations (EAPBs) and the various healthcare providers in the country; the vast majority of healthcare providers are unaware of the costs derived from anesthesia administration, other than staff fees. For this reason, the use of microcosting techniques, despite the fact that they can provide a good approximation to the actual cost of an anesthetic technique, can be very limited precisely due to the variability among different healthcare providers. In the case of this study, it may well be that microcosting techniques, based only on two healthcare institutions and market rates, could under or overestimate the total cost of anesthesia.
To conclude, from the perspective of the Colombian health system and under the premise that there are no significant perioperative clinical differences in patients taken to non-cardiac and non-oncologic surgery under general anesthesia, though there may be a slight difference in the average cost of total intravenous anesthesia when compared with inhalational anesthesia in favor of the latter, this difference can be of zero pesos when the difference in the risk of PONV is high and when the cost of the TCI technology is low.
ETHICAL RESPONSIBILITIES
Ethics Committee endorsement
This study was approved by the Ethics Committee of Hospital Universitario San Vicente Fundacion in a meeting held on January 15, 2021, as set forth in minutes No. 02-2021; and by the Ethics Committee of IPS Universitaria in a meeting held on December 15, 2020, as set forth in minutes No. 155.
Human and animal protection
The author declares that no experiments in humans or animals were conducted for this research. The author declares that the procedures applied complied with the ethical standards of the responsible human experimentation committee, the World Medical Association and the Declaration of Helsinki.











 text in
text in