P-waves represent atrial depolarization and appear upright in electrocardiographic leads I, II and V3-6, when they originate from the sinoatrial-node. New onset inverted P-waves, may result from benign or potentially life-threatening conditions. Anesthesiologists often have to decide if further work up is necessary in such circumstances, especially in symptomatic patients. We present two examples.
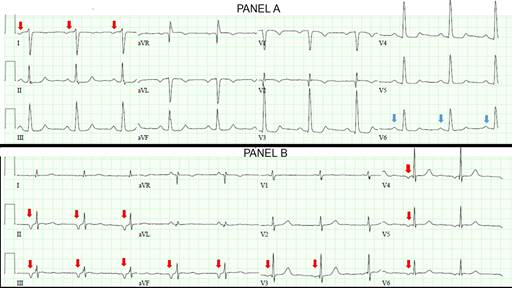
Image A, an electrocardiogram from a patient who developed nausea while recovering in the post-anesthesia-care-unit after undergoing an uneventful cystoscopy, demonstrates inverted P-waves in lead I (red-arrows) and upright P-waves in lead V6 (blue-arrows). As P-wave polarity should be similar in leads I and V6, the inconsistency in Image-A suggests reversal of left-arm and right-arm electrode positions.1 Correct electrode placement rectified P-wave inversion and ondansetron administration ameliorated nausea.
Source: Authors.
Image A: An electrocardiogram from a patient who developed nausea while recovering in the post-anesthesia-care-unit after undergoing an uneventful cystoscopy. Image B. Prominent inverted P-waves in inferior-leads II, III, aVF and precordial-leads V3-6 (red-arrows).
Image B demonstrates prominent inverted P-waves in inferior-leads II, III, aVF and precordial-leads V3-6 (red-arrows). This suggests retrograde atrial depolarization and in conjunction with a heart-rate <70 beats/min, this pattern represents an atrioventricular-junctional-rhythm. Atrioventricular-junctional-rhythm may be a manifestation of sinus-node-dysfunction, myocardial-infarction, or digoxin-toxicity.2 The electrocardiogram presented in Image B is from a patient who endorsed feeling nauseated in the post-anesthesia-care-unit after undergoing an endoscopy under propofol-anesthesia. This patient accidentally continued his oral digoxin therapy while completing a clarithromycin-based Helicobacter-Pylori eradication regimen.
Clarithromycin-induced inhibition of P-glycoprotein, an efflux pump that influences digoxin pharmacokinetics, results in increased gut absorption and decreased renal excretion of digoxin. This drug interaction can potentially precipitate digoxin-toxicity. As patients often present with non-specific symptoms such as nausea, abdominal pain, confusion, headache or dizziness, diagnosis of digoxin-toxicity necessitates a high index of suspicion. Electrocardiographic manifestations include severe bradyarrythmias and ventricular tachyarrhyhtmias. Although digoxin serum levels do not correlate with severity of toxicity, they help corroborate the diagnosis. In addition to atropine administration and institution of inotropic support, symptomatic and hemodynamically unstable digoxin-induced bradyarrhythmias may warrant early administration of digoxin-specific-antibody-fragments.3











 texto en
texto en 



