What do we know about this topic?
Even though interscalene block is ideal for shoulder procedures, there are situations in which awake injection is not possible, and injecting under anesthesia demands ultrasound guidance and a unique set of skills. This approach may sometimes be challenging in a resource limited setting.
What does this study contribute?
This is the first study as per authors' knowledge in our population to compare efficacy between intravenous dexmedetomidine and interscalene brachial plexus block in arthroscopic reconstructive shoulder surgeries which was found to have a comparable efficacy. Since dexmedetomidine is being widely used by anesthesiologists across the globe, the message will be broadly disseminated.
INTRODUCTION
Shoulder arthroscopy plays a vital role in the diagnosis and treatment of shoulder joint conditions. The most common causes of high intensity postoperative pain after surgery are direct damage to the shoulder joint muscles or reflex muscle spasm 1.
For shoulder surgery, the interscalene brachial plexus block (ISB) is the preferred regional anesthetic approach used either with sedation or in combination with general anesthesia. The advantages include reduced hemodynamic response resulting in less bleeding, better operating conditions and excellent postoperative analgesia in the immediate postoperative period 2. ISB, on the other hand, is associated with a number of side effects, including phrenic nerve blockade, which causes diaphragmatic paresis and respiratory distress; Horner's syndrome, ipsilateral weakness of the arm and hoarseness of voice. Even though interscalene block is ideal for shoulder procedures, there are situations where awake injection is not possible and administering the block under anesthesia requires ultrasound guidance and a unique set of skills. This approach may sometimes be challenging in a resource limited setting 3.
Dexmedetomidine is a highly selective a2-adrenoceptor agonist with a distinctive mechanism of action and it acts on a2-adrenoceptor in the locus ceruleus inducing sedation, while also inducing analgesia via the spinal cord adrenoceptors, in addition to attenuating the stress response without causing significant respiratory depression. In order to achieve adequate analgesia and anesthesia, Dexmedetomidine reduces the pressor response to surgery, while decreasing the dose of opioids and volatile agents 4-6.
Most of the previous research has combined intravenous (IV) dexmedetomidine with brachial plexus block for arthroscopic shoulder procedures as there is an additive effect in reducing postoperative discomfort, but there are no studies as per the authors' comparing ISB with IV dexmedetomidine 7-9.
Hence we compared the efficacy between IV dexmedetomidine infusion and ultrasound guided ISB in arthroscopic reconstructive shoulder surgery under general anesthesia with respect to intraoperative hemodynamic control using mean arterial pressure (MAP) variations requiring intervention as primary outcome, and immediate postoperative pain, operating conditions, recovery time and overall patient satisfaction as secondary outcomes.
METHODOLOGY
This prospective randomized controlled trial was conducted from March 2014 to September 2015 at a tertiary care hospital, in patients undergoing arthroscopic shoulder surgery under general anesthesia. This study received ethical approval from the institutional ethical committee, Kasturba Medical College, Manipal academy of higher education (IEC 525/2013). This study has been registered with the Clinical Trials Registry of India (CTRI/2018/03/012498).
We included patients aged >18years of either gender with American Society of Anesthesiologists (ASA) physical status I or II, scheduled for elective arthroscopic reconstructive shoulder surgery under general anesthesia. Patients with baseline heart rate of <50 bpm, patients on angiotensin receptor blockers (ARBs), angiotensin converting enzyme inhibitors (ACEIs), beta blockers and patients with known allergy to drugs used in the trial or any known contraindication to brachial plexus block were excluded from this study.
There were two observers in our study. Observer 1 (trainee) was the blinded investigator who performed the preoperative evaluation, explained the procedure, and administered the Visual Analogue Scale (VAS). Observer 1 monitored the patients after the intervention for 24 hours, recorded pain scores, administered rescue analgesia and patient satisfaction score. Observer 2 (Consultant Anesthesiologist) performed the ultrasound guided interscalene block based on the group allotted. Participants and observer 1(Trainee) were blinded.
On the night before surgery and the morning of operation, all patients were given oral pantoprazole 40mg and metoclopramide 10mg. Standard fasting guidelines were followed. Fasting status was confirmed on the day of surgery, and the patient was taken to the operating room. Non-invasive blood pressure (NIBP) cuff was attached to the arm on the non-operating side. Baseline vital parameters were noted. After becoming acquainted with the environment, three NIBP and pulse-oximeter readings were taken at 5-minute intervals and an average of three readings was taken as the baseline blood pressure and heart rate.
The intravenous line was secured under aseptic precautions with suitable gauge intravenous catheter, and a Ringer's lactate infusion was started. General anesthesia was induced with IV fentanyl 2mcg/kg and titrated dose of propofol till loss of response to verbal commands. Neuromuscular blockade was attained with 0.1mg/kg vecuronium and the patient was intubated after 3 minutes once the train of four count was zero.
Following the above, patients were randomized based on 1:1 simple random sampling according to a computer generated table of random numbers. In group DEX, an initial bolus of 0.5mcg/kg IV dexmedetomidine was administered over 20 minutes, followed by a 0.5mcg/kg/hour infusion that was discontinued 30 minutes before the procedure. In group BLOCK, ipsilateral interscalene brachial plexus block was administered with 20ml of 0.25 % bupivacaine using a liner transducer probe and a 5cm block needle 10.
After the intervention, the patient was carefully positioned in the Gross and Fitzgibbon modified lateral decubitus position, ensuring adequate padding of pressure points and avoiding undue traction on the operating limb. 66% nitrous oxide + 33 % oxygen + isoflurane was used to maintain anesthesia during the surgery. A minimum alveolar concentration (MAC) of 1 to 1.5 was maintained throughout the surgery. Throughout the surgery, mean arterial blood pressure and heart rate were monitored every 5 minutes.
Intraoperative hemodynamics were managed based on the following protocol:
Desired hemodynamics: A fall in MAP of 20% from the baseline is considered as desired hemodynamics.
Hypotension: Fall of MAP by >30% from the baseline was regarded as hypotension and treated initially by reducing the isoflurane concentration (by maintaining MAC of not < 1.0), further hypotension was managed by administering 200ml bolus of Ringer's lactate solution and 6mg ephedrine IV bolus doses. In group DEX, the infusion rate of dexmedetomidine was reduced if the blood pressure failed to increase by the above measures.
Bradycardia: A Heart rate of < 40bpm was considered as bradycardia. When the heart rate drop was gradual, IV glycopyrrolate 0.2mg bolus was administered; however a rapid drop or failure to respond to glycopyrrolate, prompted the administration of a 0.6 mg atropine bolus.
At the end of the surgery anesthetic agents were tapered off, with 0.05 mg/kg neostigmine and 0.01 mg/kg glycopyrrolate, residual neuromuscular blockade was reversed, and recovery time was recorded. The time taken for the patient to obey commands from a MAC of 0.6 after discontinuing inhalational agents was taken as recovery time. All patients were extubated on the table and transferred to the recovery room. The surgeon was asked to comment on the operating condition.
In the immediate postoperative period patients were assessed for pain on a standard visual analogue scale (VAS). If the patient complained of pain or the pain score was higher than 4, an IV bolus of nalbuphine 6mg was administered as rescue analgesic. In patients who did not require initial rescue analgesics, the time elapsed until the first demand of rescue analgesic was noted. The sensory and motor recovery of the blocked limb was evaluated 24 hours later, and a patient satisfaction score was recorded. Any adverse effects or complications during the study in either groups were documented.
Study results were analyzed using composite scores (Table 1). To individually assess the overall quality of anesthesia care, a quality assessment (QA) composite score including all of the above outcomes was used: score ≤ 5: ideal, score 6-10: acceptable and score >10 or score of 3 in any parameter: unacceptable.
Table 1 Outcomes scoring system used in the analysis.
| Score | Primary outcome | Secondary outcomes | |||
|---|---|---|---|---|---|
| Intraoperative hemodynamics* | Postoperative pain (VAS score) | Recovery time | Surgeon's opinion | Patient satisfaction | |
| 0 | Desired MAP (20% fall from the baseline) | 0 | <10 min | Excellent | Excellent |
| 1 | 10% variation on either side of desired MAP | 1-3 | 10-15 min | Good | Good |
| 2 | Single intervention to treat hypotension, bradycardia or hypertension | 4-7 | 16-20 min | Fair | Fair |
| 3 | Multiple interventions | >7 | >20 min | Poor | Poor |
* Only pharmacological interventions were considered. MAP: mean arterial pressure; VAS: Visual analogue scale.
Source: Authors.
STATISTICAL ANALYSIS
The sample size was calculated based on the results of the pilot study (n=5) with a mean composite score difference of 1 considered as significant. With the level of significance at 1%, power of study 90%, a total of 48 patients were enrolled. Based on the computer generated randomization table, patients were divided into 2 groups with 24 patients in each group.
All continuous variables are expressed as mean and standard deviation (SD), whereas categorical variables are expressed as percentages. The significance of continuous and categorical variables was investigated using the Student's t test and the Chi-square test, respectively. The significance of the results was determined at a 5% level of significance ('p' 0.05). The data was analyzed using the Statistical Package for the Social Sciences (SPSS) (version 20.0, IBM Corp. 2010 Armonk, NY, USA).
RESULTS
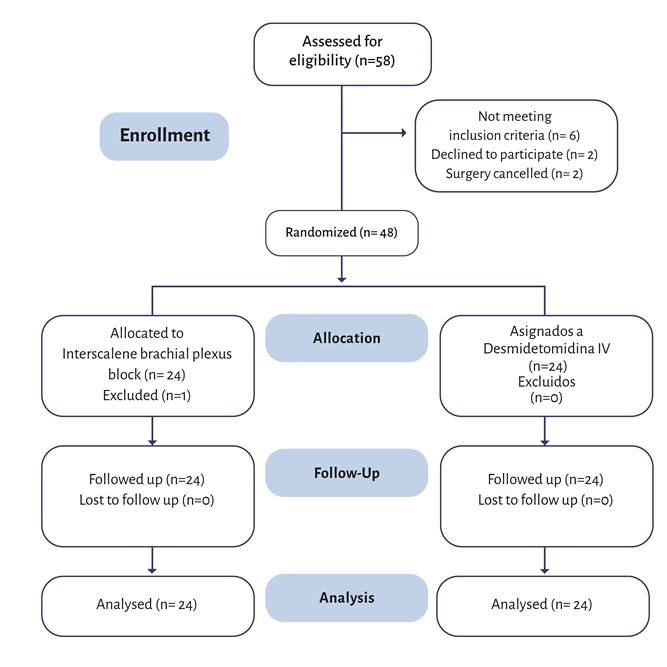
Forty eight patients were enrolled in the study with twenty four patients in each group (Figure 1). Mean age in group BLOCK was 38.95±19 (19-60) years and in group DEX was 38.41±18 (18-57) years. There were 22 males and 2 females in each group. The baseline characteristics were comparable between the groups (Table 2).
Table 2 Baseline characteristics.
| Characteristics | Group BLOCK (n=24) | Group DEX (n=24) |
|---|---|---|
| Age (years) | 38.95±19* | 38.41±18* |
| Gender: | ||
| Males | 22 | 22 |
| Females | 2 | 2 |
*Mean± SD. Source: Authors.
Intraoperative hemodynamics
Assessed in terms of MAP variation during surgery requiring interventions and comparable between the two groups (Table 3). 38 patients (20 in BLOCK and 18 in DEX) had a MAP 10% on either side of the desired level which is acceptable. Three patients in group BLOCK and five patients in group DEX received single dose of 6mg of ephedrine intravenously. One patient in group DEX received multiple doses of 25mcg of intravenous fentanyl as analgesia was found to be inadequate.
Secondary outcomes
Immediate postoperative pain
Table 4 illustrates that all patients except one had no pain in the BLOCK group. Whereas in group DEX only one patient did not complain of pain and eleven patients required immediate rescue analgesia. This was clinically and statistically significant (p = <0.001).
Tabla 4 Desenlaces secundarios.
| Outcomes | Score | Group BLOCK (n=24) | Group DEX (n=24) | p-value* |
|---|---|---|---|---|
| Immediate postoperative pain | 0 | 23 | 1 | <0.001 |
| 1 | 1 | 12 | ||
| 2 | 0 | 11 | ||
| 3 | 0 | 0 | ||
| Surgeon's opinion | 0 | 23 | 19 | 0.2 |
| 1 | 1 | 4 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 1 | ||
| Recovery time | 0 | 21 | 20 | 0.14 |
| 1 | 1 | 4 | ||
| 2 | 2 | 0 | ||
| 3 | 0 | 0 | ||
| Patient satisfaction | 0 | 16 | 1 | <0.001 |
| 1 | 8 | 23 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 0 |
*Fisher's exact test.
Source: Authors.
Surgeon's opinion
Table 4 shows that the operating conditions were scored as excellent in 42 of the cases (23 out of 24 in BLOCK and 19 out of 24 in DEX). One patient in the BLOCK group and four patients in the DEX group were scored as good operating conditions. In one patient, the operating condition was considered poor due to poor vision. This can be attributed to inadequate analgesia leading to poorly controlled blood pressure. This was the same patient who received multiple doses of fentanyl intraoperatively.
Recovery time
As depicted in the above Table 4, most of the patients recovered within 15 minutes and the majority recovered in less than 10 minutes. Contrary to what one would expect, all patients recovered within 15 minutes in group DEX, whereas two patients in group BLOCK required more than 15 minutes to recover; i.e. 16 and 17 minutes.
Patient satisfaction
Table 4 shows that the majority of the patients in group BLOCK (16/24) reported their overall experience as excellent (score 0); the remaining (8/24) patients rated it as good (score 1). In group DEX, one patient rated the overall experience as excellent and the remaining twenty three of the twenty four patients rated the experience as good. Using Fischer's exact test, the p value was <0.001 which is statistically significant; however all of the 48 patients rated the experience as either excellent or good. We consider that clinically both techniques were rated high by the patients.
Total quality assessment score
Table 5 shows that all of the patients in group BLOCK had an ideal score, whereas the majority of the patients (22 out of 24) in group DEX had an ideal score with one case being acceptable and one unacceptable which is statistically insignificant.
Table 5 Total quality assessment score.
| Score | Group BLOCK (n=24) | Group DEX (n=24) | p-value* |
|---|---|---|---|
| 0-5 (Ideal) | 24 | 22 | 0.352 |
| 6-10 (Acceptable) | 0 | 1 | |
| >10 or 3 in any parameter (Unacceptable) | 0 | 1 |
*Fisher's exact test.
Source: Authors.
None of the patients in both groups experienced any untoward events because of the intervention.
DISCUSSION
Diagnostic and surgical arthroscopy of the shoulder has become a common procedure because of a faster convalescence. As anesthesiologists, we have to cater to both surgical and patient demands, including maintaining a stable intraoperative hemodynamics which ensures a clear operating field, thus providing good intraoperative and postoperative analgesia which finally makes the patient comfortable. Regional anesthesia or a combination of regional with general anesthesia will help in achieving these goals 11.
Though there are several studies proving the efficacy of ISB in arthroscopic shoulder surgeries 1-3, the procedure is technically challenging and has to be performed by a skilled anesthesiologist; although dexmedetomidine provides stable hemodynamics and good analgesia as reported in various studies, its usefulness has rarely been studied in shoulder arthroscopy 4-6.
With regards to intraoperative hemodynamics, in this study a MAP 20% below the preoperative baseline was required, to ensure a clearer arthroscopic view. Both the ISB and IV dexmedetomidine pro-vided stable hemodynamics during the intraoperative period with no significant difference. This is similar to the recent ISB studies by Lee et al. 2 and Choi et al. 12 which have reported stable intraoperative hemodynamics and better visual clarity scale in arthroscopic shoulder surgery. Also studies by Patel et al. 13 and Hamid et al. 14 in arthroscopic shoulder surgeries revealed that MAP and heart rate were significantly lower throughout the intraoperative and the early recovery period in patients on dexmedetomidine.
Even though 40% of healthy surgical patients receiving IV dexmedetomidine have reported hypotension and bradycardia, none of the patients in our study had significant hypotension or bradycardia requiring repeated pharmacological intervention. The possible explanation being that the standard recommended dose of dexmedetomidine is 1 ng/kg over 10 min as loading dose during surgery, which accounts for the hemodynamic side effects 14), whereas in this study we used an initial bolus of 0.5mcg/kg given slowly over 20 minutes.
According to some reports, 30-70% of patients experience post-operative pain following arthroscopic shoulder surgery. Pain creates a delay in the healing and regeneration of the operated shoulder because it is such a distressing entity. As a result, post-operative pain control is critical in these procedures 2. The findings in this study showed that the interscalene block provided good postoperative analgesia when compared to IV dexmedetomidine. In patients who received IV dexmedetomidine, 11/24 patients needed immediate rescue analgesic, suggesting that dexmedetomidine alone is not able to provide adequate postoperative analgesia. Our study clearly demonstrates better postoperative analgesia with interscalene block versus dexmedetomidine infusion, similar to the meta-analysis by Abdallah et al. 15 which reported that ISB can offer enough analgesia for up to 8 hours following shoulder surgery, in addition to its opioid-sparing effect, hence preventing opioid-related side effects in the first 12 to 24 hours.
Providing an oligemic surgical field and better visibility during shoulder arthroscopy reduces the duration of surgery, thus decreasing the duration of anesthetic exposure, recovery time and overall cost. The literature review conducted by the authors did not identify any prior studies commenting on the surgeon's review on the operating field; thus this was considered an objective in the study. All of the procedures in this study were performed by the same surgeon, who stated that the operating field was outstanding in the majority of instances in both groups. This is similar to a study by Hamid et al. 14 wherein the efficacy of intraoperative dexmedetomidine infusion was compared to that of fentanyl in arthroscopic shoulder surgery under general anesthesia, and confirmed that patients on dexmedetomidine infusion had better surgical field and visibility.
In our study the recovery profile was comparable between the two groups. Contrary to what one would expect, all patients recovered within 15 min in group DEX but two patients in group BLOCK required 16-17 min which could be attributed to excellent analgesia provided by the block leading to minimal stimulation. This is similar to a study by Bajwa et al. 5 which reported good quality of extubation with dexmedetomidine without delay but they failed to quantify the recovery time, as was also the case in a study by Jung et al. 16 that reported delayed awakening following intraoperative dexmedetomidine infusion in combination with general anesthesia for laparoscopic hysterectomy.
We felt it was important to assess the patient's overall experience and their opinion about the intervention as they consented to participate in the trial. A large prospective study conducted by Singh A et al. 17 in 1319 patients showed that 99.06% of the patients were satisfied with the results of ultrasound guided interscalene block anesthesia for shoulder arthroscopy. Though many studies on dexmedetomidine concluded that it provides high level of patient comfort, none of them have actually taken patients' opinion into consideration 7-9,14 and the results were mostly inferred indirectly from the sedation scores. Our study is different in the sense that we collected the direct opinion of the patient about the overall experience of the perioperative period 24 hours later. Though we found a statistically significant difference between the two study groups as per postoperative analgesia, patients did not perceive such significance when rating their experience 24 hours later. The immediate availability of rescue analgesia may be responsible the high satisfaction ratings by these patients.
Finally, when analyzing the QA score, most of the patients in both groups reported an ideal experience. Consequently, we may conclude that IV dexmedetomidine infusion is a safe and effective alternative to ISB for reconstructive shoulder arthroscopy under general anesthesia.
Strengths of the study
First study comparing IV dexmedetomidine infusion with gold standard ISB, in addition to assessing the surgeon's opinion unlike any previous studies.
Limitations
Single center study, small sample size, and delayed postoperative pain was not assessed.
Implications for practice and/or research
This is the first study as per authors' knowledge in our population to compare efficacy between intravenous dexmedetomidine and interscalene brachial plexus block in arthroscopic reconstructive shoulder surgeries, showing comparable efficacy. Since dexmedetomidine is being widely used by anesthesiologists across the globe, the message will be broadly disseminated.
CONCLUSION
For arthroscopic reconstructive shoulder surgeries under general anesthesia, IV dexmedetomidine is equivalent to ISB in providing stable intraoperative hemodynamics, good operating conditions, post-operative recovery time and overall patient satisfaction. However, ultrasound guided interscalene block provides a better immediate postoperative analgesia. Thus in a resource limited setting, IV dexmedetomidine infusion can be used as an alternative to ISB.
Ethics committee approval
This study received ethical approval from institutional ethical committee Kasturba Medical College, Manipal academy of higher education (IEC 525/2013). This study has been registered with the Clinical Trials Registry of India (CTRI/2018/03/012498).
Protection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
ACKNOWLEDGEMENTS
Authors' contribution
STK: Conception of the original project, study planning, interpretation of results, and final writing and approval of the manuscript
MP and VP: Study planning, data collection, interpretation of results, and initial writing of the manuscript.
NV: Study planning, data collection, interpretation of results, data analysis, and final writing of the manuscript.











 text in
text in