INTRODUCTION
Major complications have been recorded in 3 - 17% of patients undergoing surgery that require hospital admission in high income countries, with mortality or permanent disability rates ranging from 0.4 % to 0.8 %. This has led to the worldwide implementation of the campaign "safe surgery saves lives". 1 The World Health Organization (WHO) summarized the basic safety standards that should be followed in the operating room when conducting a procedure, in order to ensure patient safety. 2 This initiative was adopted in Colombia within the framework of the 28th Colombian Congress of Anesthesiology in 2009. 3
The correct use of the surgical safety checklist (SSC) promotes a culture of safety among the entire surgical team. It is extremely important to involve the anesthesiology trainees since they will be the future leaders in patient safety. It has been shown that exposure to a perioperative safety culture from early stages in academic training is effective and persists for up to 15 years after the completion of the residency. 4 Consequently, it is indispensable to learn about the appropriation, perception and implementation from the perspective of the anesthesiology residents.
During the implementation of the checklist, the literature shows the significant benefits in terms of decreased mortality. 5,6 Haynes et al. 7 found that after administering the SSC in hospitals in different cities around the world, the mortality rate dropped from 1.5 % to 0.8 %. A study in Colombia reports an adherence above 90 % with most of the items in the SSC, in addition to a reduction in the number of adverse events since the list has been implemented (from 7.26 % to 3.29 %) 8. A second study found that the SSC was completed in 75.5 % of the surgical cases assessed. 9
Consequently, the purpose of this study was to establish the level of appropriation of the SSC in the training of anesthesiologists in Colombia, and to identify the perception and the level of implementation of such list at the national scale.
METHODS
A survey-type observational, descriptive study was designed with approval of the ethics committee of the Universidad de Caldas. Each participant signed the informed consent.
Anesthesia residents of all the medical schools endorsed by the National Ministry of Education were included. Residents from other medical-surgical specialties, undergraduate medical students, and other healthcare-related professions, as well as anesthesiology residents studying abroad were all excluded.
The researchers designed a digital survey based on the key findings described in the literature with regards to the limitations for the implementation of the SSC. The survey was reviewed and a pilot test was used to assess its performance. The questions were classified into three major domains: appropriation, perception and implementation. The survey was distributed via email and via the personal mobile phone of each of the national residents. The survey was available online through the platform from March 4 through March 18, 2021. The data were collected in a platform-generated database.
STATISTICAL ANALYSIS
The summary of the continuous data was based on medians and interquartile ranges. The answers to the Likert-type questions were analyzed using frequency distribution tables. The information was analyzed using the Stata software version 16.1 in an exploratory approach.
RESULTS
From a total number of 394 residents of anesthesiology in the country, 231 answers were collected. After screening the database, 215 valid answers were included for analysis, which corresponded to 54.6% of the total population. The mean age was 28 years with an interquartile range of 27 to 31 years. The other socio-demographic characteristics of the population are shown in Table 1; all the anesthesiology programs in the country participated in variable proportions (Figure 1).
Table 1 Socio-demographic variables of the participating residents.
| Socio-demographic variables | n | % | |
|---|---|---|---|
| Gender | Male | 93 | 43.2 |
| Female | 122 | 56.8 | |
| Level of residence | First year | 55 | 25.6 |
| Secondyear | 76 | 35.3 | |
| Third year | 72 | 33.5 | |
| Fourth year | 12 | 5.6 | |
| Age | Average | 29.2 years (SD 0.24) | |
| Median | 28 years | ||
| Interquartile range | 27-31 years | ||
SD: Standard deviation.
Source: Authors.
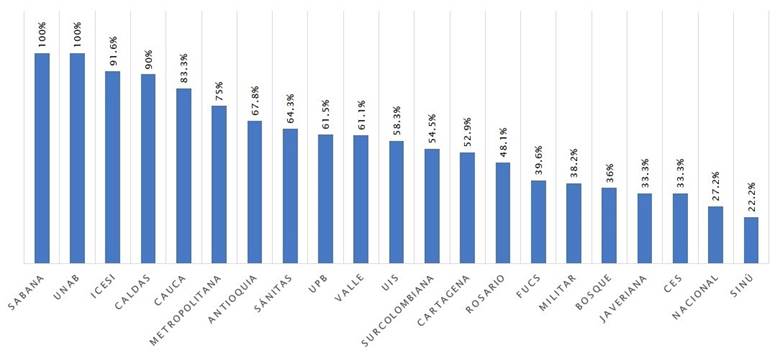
CES: Corporación de Estudios para la Salud; FUCS: Fundación Universitaria de Ciencias de la Salud; UIS: Universidad Industrial de Santander; UNAB: Universidad Autónoma de Bucaramanga; UPB: Universidad Pontificia Bolivariana. Source: Authors.
Figure 1 Participating universities.
Appropriation of the SSC
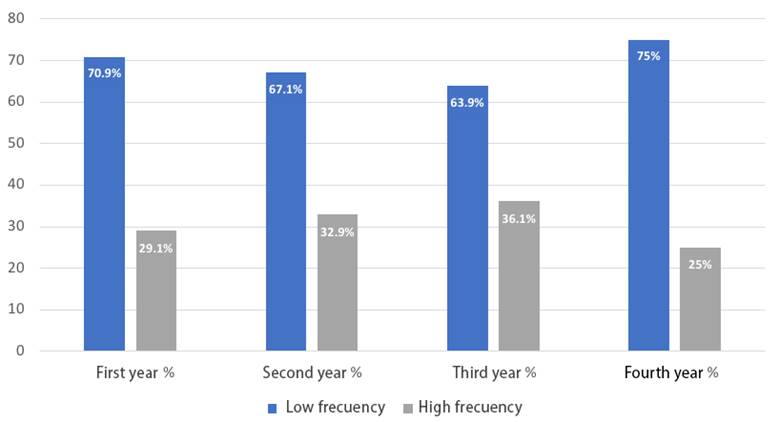
39.1 % of the residents said that they had never or almost never been exposed to any formal training on the SSC and the frequency of reviews does not change as they move forward in their residence year (Table 2 and Figure 2).
Table 2 Appropriation.
| Appropriation | Frequency | n | % |
|---|---|---|---|
| Formal academic reviews | Never | 43 | 20 |
| Almost never | 41 | 19.1 | |
| Occasionally | 61 | 28.4 | |
| Frequently | 37 | 17.2 | |
| Very frequently | 33 | 15.3 | |
| Total | 215 | 100 | |
| The most important moment of the SSC based on the academic reviews | Has not had any reviews | 50 | 23.2 |
| Before the induction of anesthesia | 90 | 41.9 | |
| Before the surgical incision | 12 | 5.6 | |
| Before leaving the operating room | 0 | 0 | |
| At the three moments | 63 | 29.3 | |
| Total | 215 | 100 | |
| Knowledge about the impact on mortality gained from academic reviews | Has not had any reviews | 51 | 23.7 |
| Does not remember | 39 | 18.1 | |
| Has no impact on mortality | 3 | 1.4 | |
| Low mortality impact | 4 | 1.9 | |
| Average mortality impact | 23 | 10.7 | |
| High mortality impact | 95 | 44.2 | |
| Total | 215 | 100 |
Source: Authors.
Perception
97.2 % of the residents considered that the use of the SSC improves the safety of surgical procedures and helps to develop a culture of safety among the team. With regards to the attitude of the anesthesiologists when administering the checklist, 88.3 % perceived a moderate to high acceptance and when asked about the attitude of surgeons, 60 % of the residents felt they had a similar attitude (Table 3).
Table 3 Perception.
| Perception | n | % | |
|---|---|---|---|
| I mproved safety of surgical procedures | Disagrees | 2 | 0.9 |
| Partially agrees | 4 | 1.9 | |
| Totally agrees | 209 | 97.2 | |
| Total | 215 | 100 | |
| Improved surgical team communication | Deteriorates communication | 0 | 0 |
| Has no impact on communication | 3 | 1.4 | |
| Partially agrees | 13 | 6.1 | |
| Totally agrees | 199 | 92.5 | |
| Total | 215 | 100 | |
| Improved safety culture | Deteriorates the safety culture | 0 | 0 |
| Has no impact on safety culture | 1 | 0.5 | |
| Partially agrees | 5 | 2.3 | |
| Totally agrees | 209 | 97.2 | |
| Total | 215 | 100 | |
| Delays the start of the procedure | Disagrees | 179 | 83.3 |
| Partially agrees | 30 | 13.9 | |
| Totally agrees | 6 | 2.8 | |
| Total | 215 | 100 | |
| Easy to administer | Yes | 210 | 97.7 |
| No | 5 | 2.3 | |
| Total | 215 | 100 | |
| If you ever undergo surgery, would like the SSC to be used? | Yes | 215 | 100 |
| No | 0 | 0 | |
| Total | 215 | 100 | |
| Has any significant oversight been prevented with the use of the SSC? | Yes | 183 | 45.1 |
| No | 32 | 14.9 | |
| Total | 215 | 100 | |
| Length of the SSC | Too short | 0 | 0 |
| Short | 4 | 1.9 | |
| Adequate | 173 | 80.5 | |
| Long | 36 | 16.7 | |
| Too long | 2 | 0.9 | |
| Total | 215 | 100 | |
| Dispense with any moment | None | 156 | 72.5 |
| Before the induction of anesthesia | 3 | 1.4 | |
| Before the surgical incision | 24 | 11.2 | |
| Before leaving the operating room | 24 | 11.2 | |
| All | 8 | 3.7 | |
| Total | 215 | 100 | |
| Acceptance by anesthesiologists | Rejection | 1 | 0.5 |
| Indifferent | 10 | 4.7 | |
| Low acceptance | 14 | 6.5 | |
| Moderate acceptance | 71 | 33.0 | |
| High acceptance | 119 | 55.3 | |
| Total | 215 | 100 | |
| Acceptance by surgeons | Rejection | 5 | 2.3 |
| Indiferente | 22 | 10,2 | |
| Baja aceptación | 59 | 27,5 | |
| Moderada aceptación | 71 | 33,0 | |
| Alta aceptación | 58 | 27,0 | |
| Total | 215 | 100 | |
Source: Authors.
Implementation
80.5 % of the residents noticed that the SSC is competed always or almost always.
When inquiring about the presence of the full team at the time of administering the SSC, 40 % said the team was always complete and 88 % of the residents have observed that the form is completed without a proper verification. 40 % has evidenced this behavior always or almost always (Table 4).
Table 4 Implementation.
| Implementation | n | % | |
|---|---|---|---|
| Who administers the SSC? | Anesthesiologist | 129 | 60 |
| Licensed practical nurse | 127 | 59.1 | |
| Anesthesiology resident | 80 | 37.2 | |
| Scrub nurse | 69 | 31.2 | |
| Surgeon | 57 | 26.5 | |
| Head nurse | 46 | 21.4 | |
| Surgical resident | 27 | 12.6 | |
| Have you seen the SSC being implemented? How frequently? | Never | 0 | 0 |
| Almost never | 9 | 4.2 | |
| Some times | 33 | 15.3 | |
| Almost always | 80 | 37.2 | |
| Always | 93 | 43.3 | |
| Total | 215 | 100 | |
| At which moment is the SSC more often administered? | None | 0 | 0 |
| Preinduction of anesthesia | 159 | 74 | |
| Pre-surgical incision | 25 | 11.6 | |
| Before leaving the operating room | 1 | 0.5 | |
| All | 30 | 13.9 | |
| Total | 215 | 100 | |
| How rigorous is the administration of the SSC? | Very low | 2 | 1 |
| Low | 6 | 2.8 | |
| Medium | 65 | 30.2 | |
| High | 114 | 53.0 | |
| Very high | 28 | 13.0 | |
| Total | 215 | 100 | |
| The surgical team in full is present | Never | 1 | 0.5 |
| Some times | 12 | 5.5 | |
| Fifty percent of the times | 26 | 12.1 | |
| Most of the time | 90 | 41.9 | |
| Always | 86 | 40.0 | |
| Total | 215 | 100 | |
| Have you seen that the SSC form is completed without a rigorous verification? | Never | 26 | 12 |
| Very rarely | 53 | 24.7 | |
| Some times | 50 | 23.3 | |
| Almost always | 46 | 21.4 | |
| Always | 40 | 18.8 | |
| Total | 215 | 100 | |
| Have you seen the use of technology tools? | Never | 90 | 41.9 |
| Very rarely | 68 | 31.6 | |
| Some times | 30 | 13.9 | |
| Almost always | 15 | 7.0 | |
| Always | 12 | 5.6 | |
| Total | 215 | 100 | |
Source: Authors.
Discussion
Patient safety associated with the perioperative environment is an ongoing concern and ideally should be mandatory. Enhancing patient safety has been shown to decrease the number of adverse events, improve patient safety and raise the level of satisfaction and confidence of the surgical team to conduct the procedures, particularly when these procedures are not frequently conducted. 10
Patient safety education at the academic institutions responsible for training healthcare human resources is not given the importance it deserves. 11 In this study, 20 % of the residents said they have never been exposed to a formal review on surgical safety checklists, while 80 % said they did, though with varying levels of frequency. This is in contrast with the results of the Accreditation Council for Medical Graduate Education in the United States, in a study conducted between September 2012 and March 2015, which interviewed 297 institutions comprising 8,755 residents and fellows of all the clinical and surgical specialties. This study showed that 96.8 % of the residents had received formal education on patient safety via group discussions and virtual sessions with questions. 4 Additionally, the study found that the primary center where learning takes place has a lasting impact on the professional behavior and conduct of the graduated residents for up to 15 years; therefore, it is important that the institutions that admit residents be even more diligent in the implementation of surgical safety checklists and in their patient safety policy. 4
Patient safety education is considered a "non-major" subject in the curriculum and skills development plan of the anesthesiology program in Colombia, published by the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.) in 2016 12. In this program, the subjects or topics are classified into two domains: "inclusion recommended" and "discussion"; such classification is based on surveys administered to anesthesiologists and by comparisons against universities abroad. The closest subject description in this classification is "safety and anesthesia", which belongs to the discussion domain and is not considered "mandatory" in the anesthesiology curriculum. This situation is most concerning since in the "inclusion recommended" domain there are subjects or situations to which anesthesiologists will be very seldom exposed to, while patient safety and the surgical safety checklist are part of the daily practice of any anesthesiologist. 12
No information has been found on patient safety among postgraduate students at the national level; in contrast, there are review articles and a systematic review of patient safety involving undergraduate students. A significant involvement of nursing programs in patient safety is to be noted. 13 These documents emphasize the importance of teaching patient safety to undergraduate students, since they are more likely to use the knowledge acquired and to practice a culture of safety during their professional lives. 11 It is quite surprising that 23.8 % of the anesthesiology residents feel that one of the three moments in the list could be disregarded; 3.75 % believe that all the three moments may be omitted; moreover, 20 % of them have never experienced any formal reviews on the topic, notwithstanding the evidence that these teachings - even in undergraduate programs - may prove to be effective. 14 This behavior is similar to the situation in Guatemala, where albeit the wide acceptance of the SSC, there is poor implementation and use. 15
Studies such as the one by Haynes et al. 16 suggest that the introduction of the surgical safety checklist generates a change in perception about safety of the surgical team members and this change in perception is associated with improved mortality and morbidity outcomes. In this study, the anesthesiology residents in the country felt that the SSC improves the safety of surgical procedures, enhances communication and strengthens the culture of safety of the perioperative team, with no negative impact on the timely start ofthe procedure. Moreover, their perception is that it is not difficult to use and 85 % have found that the use of the checklist has prevented the occurrence of adverse events. 100 % of the residents expressed their wish to have the SSC implemented if they were to undergo a surgical procedure, although 2.8 % of them doubt that the use of the SSC improves safety.
Russ et al. 17, in their study on barriers and facilitators for the implementation of the SSC in the United Kingdom, unveil the existence of organizational barriers to the implementation of the checklist, in addition to hurdles associated with the team involved and highlight active resistance or passive non-compliance by the surgeon or the anesthesiologist. In this regard, the study found that the attitude of the anesthesiologist tends to be empathetic vis a vis the administration of the checklist, but 40 % of the surgeons tend to reject or show poor acceptance of the checklist.
When asking the residents surveyed about any potential changes to the surgical safety checklist to which they have been exposed, most of them said they would not make any changes. However, when assessing the administration of the checklist, 74 % said that it is used during the first moment and only 13.9 % administer the checklist in full, which has proven to be most effective approach. 18 Therefore, it is yet unclear whether the institutional changes to the SSC improve its applicability or make it longer and more difficult to use and hence those who implement the checklist in their daily practice only use it for the first moment.
While 80 % of the residents expressed that the SSC are always or almost always administered, it is quite concerning that 88 % have seen that the SSC form is completed without conducting a proper timeout; hence, this highly effective tool becomes just one more document attached to the patient's medical record. Moreover, in most cases, it is mostly administered before the induction of anesthesia, and when asked about the presence of all the team members involved with the procedure, only 40 % of the residents said that the surgical team was complete at the time of the administration of the checklist. This proves that strictness if highly variable and this affects the effectiveness of the SSC. 18,19 According to our study, the principal actors responsible for the implementation of the SSC are the anesthesiologists - 60% of the cases - and the licensed practical nurse represents 59.1 %; these data are consistent with previous local studies. 9
According to Stolsky et al. 20, this behavior may be the result of the fact that the institutional changes introduced to the SSC delete the items intended to foster communication or include additional items to try to make the list more comprehensive; however, the result is a list designed to simply check boxes instead of providing an opportunity to identify potential errors. Therefore, further studies are needed to assess barriers and facilitators for the administration of the SSC.
This study may have been subject to selection biases (volunteer effect). To overcome this bias, a broad dissemination of the survey was conducted via email forwarded directly from the Office of Scientific Research of the S.C.A.R.E. Moreover, the anesthesia residents were reached by phone by the heads of the residency program and the postgraduate coordinators of each school.
In conclusion, there is little exposure to SSC education in the anesthesiology postgraduate programs in the country during the residency; a significant proportion of residents complete their career training without a clear understanding of the SSC. The anesthesiology residents in the country have a favorable perception about the value of the SSC and show a positive attitude versus its implementation, hence acknowledging and promoting its proper use.
ETHICAL RESPONSIBILITIES
Endorsed by the Ethics Committee
This study was approved by the Ethics Committee of Universidad de Caldas under code CBCS-090 dated November 23, 2020, in Manizales, Colombia.
Protection of persons and animals
The authors declare that no experiments in humans or animals were conducted for this research project. The authors declare that the procedures followed were consistent with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.











 text in
text in