INTRODUCTION
The erector spinae plane (ESP) block is a regional anesthesia technique first described by Forero et al. 1 as a modified interfascial block initially used for patients with chronic neuropathic thoracic pain to provide wide sensory blockade, including the anterior and posterior regions of the chest.
Reports and case series 2-6 have suggested good results, spurring interest in the scientific community and leading to studies designed to assess anatomic and physiologic considerations, as well as the clinical applications of this technique.
The usefulness and safety of the ESP block have been elucidated in different scenarios 1-3. As an analgesic/anesthetic technique, it appears to offer advantages over other regional options such as neuraxial and paravertebral blocks, which pose a higher risk of dural or pleural punctures and other side effects 3.
Although it needs to be highlighted that there are no learning curves for this block so far, it has positioned itself as an innovative technique described as easy to perform in the practice of anesthesia 1-8.
The purpose of this review is to summarize the main indications for the ESP block in the practice of anesthesia, and to document the complications described to this date. A broad literature search was conducted in PubMed, Google Scholar and the Cochrane Library between July 2018 and November 2020. The inclusion criteria were articles on ESP block identified in the search, including letters to the editor, case reports, case series, cadaveric studies, reviews, meta-analyses and clinical trials in both adult and pediatric populations. The exclusion criteria were articles in languages other than Spanish or English, animal studies or articles unrelated to the ESP block. The terms used were Erector Spinae Plane Block, ESP block, and Erector Spinae block.
The full texts of 80 articles were read and data on the surgical model, anatomic site pain, anesthetic dose and type, numerical pain scale, complications and other relevant observations were collected. The most relevant findings are described in Tables 1 and 2.
Table 1 ESP block randomized clinical trials.
| Surgical area | Author/ Year | Study type | Pain | Surgical model/ intervention | Comparison | Sample | Level | Single dose vs. continuous | Laterality | Local anesthetic and dose | Mean NRS* afterwards | Conclusion | Complication | Primary outcome statistical value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Thorax | Barrio 2020 13 | CO | A | Rib fractures. herpes zoster neuritis. thoracostomy and myofascial pain syndrome | 18 | T5-T7 | SD | U | 0.5% B 20 ML | < 2 | 16 patients with pain modulation, mean blocked dermatome extension of 9 (range 8-11) | None | ||
| Ciftci, 2019 28 | RCT | A | Videothoracoscopy | ESP vs. multimodal analgesia | 60 | T5 | SD | U | 0.25% B 20 mL | ESP 1 VS. No ESP 5 | ESP less POP pain and less res-cue opioids. no adverse effects | None | Opioid use in ESP 10.00 ug ± 14.62 ug vs. no esp 47.33 ug ± 16.17 ug, P <0.001 | |
| Gaballah, 2019 29 | RCT | A | Videothoracoscopy | ESP vs. PVB | 60 | T5 | SD | U | 0.25% B 20 mL | ESP 1.13 vs. No ESP 5.13 | ESP less POP pain, longer time to first rescue dose of analgesic, lower opioid use | None | POP in first 4 h lower in ESP group 1.87 ± 0.35 vs. 2.0 ± 0.01, p = 0.04, POP pain at 6 h lower in ESP group 3.33 ± 0.48 vs. 3.73 ± 0.45, p=0.002.time to first analgesia longer in ESP group 379.07±7.78 vs. 296.04 ± 6.62 minutes, p < 0.001 | |
| Chen, 2020 30 | RCT | A | Videothoracoscopy | ESP vs. PVB vs. ICNB | 75 | T5 | SD | U | 0.375% R 20 mL | Three groups < 4 | PPV less POP pain. Greater need for rescue analgesia in ESP Higher morphine use at 24 h in ESP | Hematoma in 4 pvb patients, 5 ICNB, o ESP | Morphine use in PVB 10.5 (9-15) mg; ICNB 18 (13.5-22.1) mg; ESP 22 (15-25.1) mg; p = 0.000 | |
| Cardio | Nagaraja, 2018 34 | RCT | A | Median sternotomy | Bilateral ESP vs. epidural catheter | 50 | T5 | CC | BL | 0.25% B 15 ml in each side and CC (0.125% B 0.1 mL/ kg/h) | First 12 hours ESP 1.68 /10 vs. Epid 1.92/10 /// 24 hours ESP 1.44 /10 vs. Epid 2.08/10 | ESP less POP at 24 hours, with no difference in NSR in first 12 hours, opioid use, spirometry, ICU length of stay. No adverse effects | None | NSR Epid 1.56 ±1.08 vs. ESP 1.04 ± 0.98 P < 0.08 first 12 h // NRS Epid 2 ±1.32 vs. ESP 0.8±0.64 p < 0.0002 after 24 hours |
| Borys, 2020 36 | CO | A | Minimally invasive thoracotomy (mitral valve replacement) | ESP vs. IV analgesia | 44 | T4 | SD | U | 0.375% R 0.2 mL/kg | 3.72 out of 10 | Shorter mechanical ventilation time and shorter ICU stay | None | Oxycodone use in ESP group was 18.26 (95% CI: 15.55-20.98) mg | |
| Krishna, 2019 37 | RCT | A | Median sternotomy | Bilateral ESP vs. tramadol + paracetamol | 106 | T6 | SD | BL | R 0.375 % 3 mg/kg (1.5 mg/ kg each side, 20-25 mL in each side) | < 4 out of 10 first 8 hours | More prolonged pain modulation in ESP group | None | NRS < 4/10 postextubation p = 0.0001 in favor of ESP | |
| Columna | Yayik, 2020 40 | RCT | A | Lumbar spine decompression | ESP vs. control (PCA tramadol) | 60 | L3 | SD | BL | 0.25% B 20 mL in each side | ESP group < 2.4 at rest and < 2.6 dynamic in the first 24 hours | ESP less dynamic and static pain, less tramadol use | None | Higher tramadol use for control group (370.33 ± 73.27 mg and 268.33 ± 71.44 mg, p < 0.001). Static pain ESP 1.93 ± 0.87 vs. 3.83 ±1.18 and dynamic pain 2.30 ± 0.60 vs. 4.63 ±1.10 p < 0.001 |
| Singh, 2020 41 | RCT | A | Major lumbar spine surgery | ESP vs. control | 40 | T10 | SD | BL | 0.5% B 20 mL in each side | ESP group < 3 vs. control group < 4 | ESP less morphine use and lower pain scores than control group | None | Lower morphine consumption (1.4 ± 1.5 vs. 7.2 ± 2.0 mg p < 0.001) ESP | |
| Qiu, 2020 42 | M | A | Lumbar spine surgery | 171 | T8 -L4 | SD + C | BL | B, R, L | Effectiveness and safety of ESP for lumbar spine surgery still controversial | |||||
| Mama | Aksu, 201943 | RCT | A | Breast surgery | ESP + PCA vs. control (PCA) | 50 | T2 and T4 | SD | U | 0.25% B 20 mL (10 mL for T2 and 10 mL for T4) | Both groups < 2 | Morphine use significantly lower in ESP group at 6, 12 and 24 hours POP | None | Morphine use at 24 h lower in ESP 3.02 ± 2.06 mg vs.13.2 ± 4.98 mg in control group, p < 0.001 |
| Swisher, 2020 44 | RCT | A | Breast surgery without uni or bilateral mastectomy | ESP vs. PVB | 100 | T3 or T4 | SD | U o BL | 0.5% R CE 20 mL unilateral or 16 mL/ side for bilateral | ESP group 3 vs. PVB group 0 | Higher pain scores and opioid use in ESP group. Lower POP morphine use for PVB group | None | Pain scores -3.0 a 0 (p = 0.0011) | |
| Gürkan, 2020 45 | RCT | A | Breastcancer surgery | ESP vs. PVB vs. control (opioid only) | 75 | T4 | SD | U | 0.25% B 20 mL vs. 20 mL vs. opioid analgesia | ESP and PVB groups < 2 first 12 h < 5 first 24 h | Opioid use (no difference in ESP and PVB). VAS1 and 6 hours POP (better in PVB than control, but no difference between ESP and control) | None | Morphine use at 24 hours 5.6 ± 3.43 mg in ESP group, 5.64 ± 4.15 mg PVB group and 14.92 ± 7.44 mg in control group, p = 0.001 | |
| Gürkan, 201846 | RCT | A | Breastcancer surgery | ESP vs. control (opioid only) | 50 | T4 | SD | U | 0.25% B 20 mL | < 2 in first 24 h for both groups | Pain modulation no different than control, 65% lower morphine use than in control group | None | Morphine use at 1, 6, 12, 24 hours lower in ESP 5.76 ± 3.8 mg vs. 16.6 ± 6.92 mg in control group, p < 0.05 | |
| Leong, 2020 47 | RS M | A | Breast surgery | ESP vs. no block vs. other blocks | 861 | T4 | SD | U | 0.25% B 20 mL | EPS group lower pain scores vs. no block group. ESP group higher pain scores vs. PNB group in first 12 hours | ESP less pain at 2, 6, 12, 24 h POP. Lower need for morphine and better recovery quality | Pneumothorax 2.6% PVB, 0% ESP | POP pain at 2 hours (-2.97 to -0.29, p = 0.02), at 6 hours (-1.49 to -0.30 p = 0.003), at 12 hours (-0.67 to -0.25 p <0.0001), and at 24 h (-0.70 to -0.30 p <0.00001). Lower morphine requirements for ESP group (-32.57 to -10.52) p = 0.00 | |
| Altiparmak, 201948 | RCT | A | Breast cancer surgery (radical mastectomy) | ESP vs. PEC2 | 38 | T4 | SD | U | 0.25% B ESP 20 ml vs. PEC2 (20 mL between pectoralis minor and serratus + 10 mL between pectoralis major and pectoralis minor) | Similar pain scores (< 1.5) between both groups at 15 and 30 minutes. lower scores in PECS group after 60 min | Pain modulation greater in PEC2 group, lower tramadol use in PEC2 group | POP tramadol use lower in PEC2 group (132.78 ± 22.44) than in ESP group (196 ± 27.03) P=0.001 | ||
| Gad, 2019 49 | RCT | A | Radical mastectomy | ESP vs. PEC2 | 50 | T4 | SD | U | 0.25% L 20 mL | Scores below 20/100 in both groups | Lower opioid use in PECS, better pain modulation and lower POP morphine use | None | Opioid use higher in ESP group (16.7 ± 7.21) vs. (10.7 ± 3.12) p = 0.001 | |
| Sinha, 2019 50 | RCT | A | Modified radical mastectomy | ESP vs. PEC2 | 64 | T4 | SD | U | 0.2% R 20 mL | PECS2 group 2 vs. ESP Group 2.6 | Pop morphine use lower in PEC2 group | Morphine use lower in PEC2 (4.40 ± 0.94 mg) vs. ESP group (6.59 ± 1.35 mg; p = 0.000) | ||
| El Gha mry, 2019 51 | RCT | A | Radical mastectomy | ESP vs. PVB | 70 | T5 | SD | U | 0.25% B 20 mL | ESP group < 3 first 6 h, PVB group < 4 first 6 h | POP morphine use during first 24 hours and time to first analgesia requirement similar between both groups. No difference in the VAS, PONV or intraoperative fentanyl use between the two groups. POP morphine use during 24 hours was similar | 4 Patients in the PVB group developed pneumothorax, o in the ESP group | POP morphine use in ESP group (26.7 ± 2.1) vs. (27.3 ± 2.9) (p = 0.32) | |
| Moustafa, 202052 | RCT | A | Radical mastectomy | ESP vs. PVB | 102 | T4 | SD | U | 0.25% B 20 mL | Not assessed | 100% success rate in ESP vs. 77.8% in PVB. POP morphine use similar between both groups | None | 100% success RATE in ESP vs. 77.8% in PVB (X2=9.11 P = 0.002) | |
| Sharma, 2020 53 | RCT | A | Breastcancer surgery (radical mastectomy + axillary lymph node resection) | ESP vs. control (opioid only) | 60 | T5 | SD | U | 0.5% R 0.4 mL/kg | ESP group < 1, control group < 4 | Pain modulation similar in both groups, lower morphine use in ESP 43% | None | Morphine use in first 24 hours lower in ESP mean differences 2.1 (2.0-2.2), p 0.01 | |
| Singh, 2019 54 | RCT | A | Modified radical mastectomy | ESP vs. control (opioid only) | 40 | T5 | SD | U | 0.5% B 20 mL | ESP group 2.7 vs control group 4.2 | Pain modulation higher and opioid use lower in ESP group | None | Morphine use in ESP (1.95 ± 2.01 mg) vs. control group (9.3 ± 2.36 mg) p = 0.01 | |
| Yao, 20 20 55 | RCT | A | Radical mastectomy | ESP vs. placebo (0.9% NSS) | 82 | T4 | SD | U | 0.5% R 25 mL | ESP group with better overall scores on the QoR-15 24 hours POP, less static and dynamic pain | ESP group better recovery quality and pain modulation | None | Better recovery quality (95% CI: 9 to 12, p < 0.001) | |
| Altiparmak, 2019 56 | RCT | A | Unilateral modified radical mastectomy | ESP with 0.375% B vs. ESP with 0.25% B | 42 | T4 | SD | U | B vs. 0.25 % 20 mL | ESP group with 0.375% B less than 2 vs. ESP group with 0.25% B less than 3.5 in first 12 h | POP tramadol use lower in ESP group with 0.375% B | None | POP tramadol use in ESP with 0.375% B (149.52±25.39mg) vs. ESP group with 0.25% B (199.52±32.78mg) (p = 0.001) | |
| Oksuz, 2019 57 | RCT | A | Reduction mammoplasty | ESP vs. tumescent anesthesia | 44 | T4 | SD | BL | 0.25% B 40 mL (20 mL in each side) | ESP group 4.1 ± 1.4, control group 5.6 ± 1.0 | Pain modulation, opioid use and patient satisfaction better in ESP group | None | Tramadol use 24 hours lower in ESP than tumescent, p < 0.001 | |
| Abdomen | Altiparmak, 2019 59 | RCT | A | Laparoscopic cholecystectomy | ESP vs. OSTAP | 68 | T7 | SD | BL | B 20 mL each side in both groups | ESP group 1.5 vs. OSTAP group 2.2 | Pain modulation and tramadol requirement lower in ESP group | None | Tramadol use lower in ESP (- 72.40 to -48.19 p < 0.001) |
| Tulgar, 2019 60 | RCT | A | Laparoscopic cholecystectomy | ESP vs. OSTAP vs. control group (no block) | 60 | T9 | SD | BL | 0.5 % B 20 mL, L2 10 mL 0.9% NSS 10 mL, 20 mL applied in each side in the block groups | ESP group 1.4 vs. OSTAP group 1.7 vs. control group 2.4 | Pain modulation, need for tramadol and paracetamol analgesia lower in both block groups than in control group | None | NRS in ESP group 1 ± 1.10. OSTAP 1.27 ± 1.41, and control group 2.95 ± 1.81, p < 0.001 | |
| Tulgar, 2018, 61 | RCT | A | Laparoscopic cholecystectomy | ESP vs. control (opioid only) | 30 | T9 | SD | BL | 0.375% B 20 mL (0.375 in each side) | ESP group 1.4 vs. OSTAP group 2.3 | Pain modulation, need for tramadol and paracetamol analgesia lower in ESP than in control group | None | NRS at 0-3 h ESP group 1.00 ± 1.13 vs. control group 2.88 ± 1.79, p < 0.01 | |
| Kwon, 2020 62 | RCT | A | Laparoscopic cholecystectomy | ESP+RSB vs. RSB | 53 | T7 | SD | BL | 0.20% R 20 mL in each side | ESP group + RSB 2 vs. RSB 3 | Lower opioid use, pain scores and remifentanil use in ESP group + RSB | None | Use of analgesic at 6 h POP 41.9Hg (165.1±67.7Hg) in ESP group + RSB vs. 207±45.5Hg in RSB, p=0.012, at 24 h POP, 77.2ug (206.5±82.8ug) in ESP group + RSB vs. 283.7±102.4ug in RSB p = 0.004 |
A: acute; B: bupivacaine; BL: bilateral; C: continuous; CC: continuous catheter; CI: Confidence interval; CO: cohort; Epid: Epidural; ICNB: intercostal nerve block; ICU: Intensive care unit; IV: intravenous; L: lidocaine; M: meta-analysis; NRS: numerical rating scale; OSTAP: oblique subcostal transverse abdominis plane; PCA: patient-controlled analgesia; PECS: pectoralis plane block; PEC2: pectoralis 2 block; PONV: postoperative nausea and vomiting; POP: postoperative; PVB: paravertebral block; QoR-15: quality of recovery; R: ropivacaine; RCT: randomized clinical trial; RSB: rectus sheath block; SD: single dose; SPB: serratus plane block; SR: systematic review; U: unilateral; VAS: visual analog scale; 0.9% NSS: 0.9% saline solution.
Source: Authors.
Table 2 ESP block case series and reports.
| Comprised anatomical site | Author/Year | Pain | Surgical model/Intervention | Sample | Level | SD vs. CC | Laterality | Dose and anesthetic |
|---|---|---|---|---|---|---|---|---|
| Thorax | Forero, 2016 1 | A/C | Oncologic pain/costal fractures/VATS | 4 | T5 | SD + C | U | 0.25% B 20 mL/0.5% R 20 mL/ 1:1 L 2% + 0.5% R 20 mL /0.5% R 20 mL |
| Muñoz, 2017 3 | A | Thoracotomy for costal tumor resection (T11) | 3 | T8 | SD | U | 0.5% B with epinephrine 5 μg/ mL 14 mL | |
| Adhikary, 2018 5 | A | VATS | 1 | T5 | SD + C | U | 0.5% R 20 ML + 0.2% R infusion 8 mL/h | |
| De la Cuadra, 2018 14 | A | Thoracotomy for correction of diaphragmatic paresis | 1 | T9 | C | U | LB 8 mL initial bolus, 0.1% infusion 3 mL/h | |
| Forero, 2017 16 | A | Thoracotomy for lobectomy | 1 | T5 | C | U | 0.5% R 25 mL + infusion 8 mL/h 0.2% R | |
| Wilson, 2018 25 | A | VATS (metastasis for T11 paraspinal thymoma) | 1 | T5 | SD | U | 0.5% R 30 mL | |
| Hu, 2019 26 | A | VATS (bullectomy) | T5 | SD | U | 0.375% R 20 mL | ||
| Navarro, 2018 27 | A | VATS (lung metastases/cystic carcinoma/lobectomy) | 4 | T5 | C | U | 0.5% B 20 mL + continuous infusion of 0.15% R 12 mL/H (first and second patients), 0.15% R at 7-12 mL/h (third patient) and 0.15% R at 12 mL/h (fourth patient) | |
| Raft, 2019 32 | A | Thoracotomy | 1 | T5 | SD + C | U | 0.5% R 20 mL + 0.2% R infusion 8 mL/h | |
| Kelava, 2018 33 | A | Thoracotomy for lung transplant | 1 | T5 | C | U | 0.25% B 15 mL + 0.2% R infusion 10 mL/h, 10 mL boluses every 4 hours while the patient remained intubated and, following extubation, 8 mL/h infusions with boluses of 12 cm3 | |
| Leyva, 2020 35 | A | Minimally invasive thoracotomy (mitral valve replacement) | 1 | T7 | C | U | 0.125% bupivacaine at 7 mL/h | |
| Gaio, 2018 (65) | A | Thoracotomy for paracardiac teratoma resection | 1 | T5 | C | U | 0.2% R 5 mL (0.45 mL/kg) plus continuous infusion of 0.1% R at 2 mL/hour | |
| Nardiello, 2018 66 | A | Sternal reconstruction (pectum excavatum/pectum carinatum) | 2 | T5 | SD | BL | 0.25% B 20 mL on each side | |
| Forero, 201722 | C | Post-thoracotomy chronic pain | 7 | T5-T6 | SD | U | R. Doses varied between 0.25 and 0.50%, and 20-30 mL volume | |
| Hamilton, 2017 17 | A | Costal fractures | 1 | T5 | C | U | 0.125% B 10 mL/h | |
| Ahiskalioglu, 2020 23 | C | Chronic thoracic oncologic pain | 1 | T5 | C | U | 0.25% B 20 mL plus 0.250% B infusion 8 mL/h and 5 mL/h boluses | |
| Ueshima, 2018 21 | A | Acute pain management after postherpetic neuralgia | 1 | T6 | SD | U | 0.25% LB 10 mL | |
| Breast | Bonvicini, 2017 6 | A | Siliconoma excision + breast implant | 1 | T5 | SD | U | R 75 mg + M 20 mg 25 mL |
| Nair, 2018 15 | A | Modified radical mastectomy + lymph node resection | 5 | T4 | SD | U | 0.25% B 30 mL | |
| Ueshima, 2018 73 | A | Radical mastectomy | 1 | T4 | SD | U | 0.25% L 10 mL | |
| Spine | Ueshima, 2017 38 | A | Thoracic vertebral surgery (lumbar stenosis and spinal cord tumor resection) | 2 | T5 | SD | BL | 0.375% L 40 mL (20 mL each side) |
| Canturk, 2019 39 | A | Spondylolisthesis correction | 1 | L1 | SD | BL | 0.25% B 10 mL, 1% P 10 mL | |
| Abdomen and pelvis | Hannig, 2018 7 | A | Laparoscopic cholecystectomy | 3 | T7 | SD | BL | 0.5% R 20 mL |
| Chin, 2017 2 | A | Laparoscopic bariatric surgery | 3 | T7 | SD/SD/C | BL | 1% R 5 mL + 2% L 5 mL + 0.9% NSS 10 mL / 0.5% R 20 mL / 0.5% R 20 mL | |
| Tulgar, 2018 58 | A | Laparoscopic abdominal surgery | 3 | T8 | SD | BL | 0.5% B 10 cm3, 2% L 5 cm3, 0.9% NSS 5 cm3 | |
| Restrepo, 2017 64 | A | Major abdominal surgery (open radical cystoprostatecto my) | 1 | T8 | C | BL | 2% L 3 mL + 0.25% B 10 mL + continuous infusion of 0.1% B at 6 mL/h | |
| Aksu, 2019 67 | A | Laparoscopic cholecystectomy | 3 | T7 | SD | U | 0.25% B at 0.5 mL/kg | |
| Hernández, 2018 68 | A | Inguinal hernia repair (anesthetic) | 1 | T6 | SD | U | 0.4 mL/kg (1:1 solution of 0.25% B and 1% L) | |
| Chin, 2017 18 | A | Ventral hernia repair | 4 | T7 | SD | BL | 0.5% R + adrenaline 5 μg/ mL 20 mL/ 0.5% R + dexamethasone 4 mg 30 mL / 0.5% R + dexamethasone 4 mg 20 mL/R 0,5 % + dexamethasone 4 mg 20 ML | |
| Selvi, 2018 75 | A | Cesarean section | 1 | T11 | SD | BL | 0.5% B 15 ML + 2% L 5 mL+ 0.9% NSS 5 mL | |
| Altinpulluk, 2018 63 | A | Cesarean section | 1 | T9 | SD | BL | 0.25% B 20 mL | |
| Limbs | Forero, 2017 24 | C | Chronic shoulder pain | 1 | T2 | SD | U | 0.5% B 20 mL |
| Tulgar, 2018 69 | A | Hip arthroplasty | 1 | L4 | SD | U | 0.5% B 15 mL, 2% L 5 mL, 0.9% NSS 10 mL | |
| Bugada, 2018 70 | A | Hip replacement/surgical revision of recurrent hip dislocation | 2 | L4 | C | U | 0.75% R 25 mL, PCA infusion 0.5 mL/h + 20 mL bolus every 3 h | |
| Darling, 2018 71 | A | Surgical hip dislocation and femur osteotomy | 1 | T12 | C | U | 0.2% R 10 mL | |
| Balaban, 2019 72 | A | Total knee arthroplasty | 1 | L4 | C | U | 0.375% B 30 mL | |
| Am J Emerg Med., 2019 74 | C | Regional complex syndrome in right ankle and foot | 1 | L4 | SD | U | 0.5% B + 2% L 30 mL |
A: acute; B: bupivacaine; BL: bilateral; C: chronic; CC: continuous catheter; L: lidocaine; LB: levobupivacaine; NSS: 0.9% saline solution; PCA: patient-con-trolled analgesia; R: ropivacaine; 0.9%; SD: single dose; U: unilateral; VATS: video-assisted thoracoscopic surgery.
Source: Authors.
ANATOMY
The thoracolumbar fascia (TLF) 9 is an important structure in the ESP block since it enables distal spread of the local anesthetic (LA) from the site of administration; it consists of fascia layers and aponeurotic tissue which separate paraspinal muscles from the posterior abdominal wall muscles; it extends cephalad, along the thoracic and cervical spine, up to the skull base, and caudal down to the sacroiliac level posteriorly 9-11.
The erector spinae muscles include the iliocostalis, longissimus and spinalis (multifidus); they arise from a common aponeurosis (the three columns of the broad tendon), form at the level of L5 and attach to the posterior inferior iliac crest, the posterior sacrum, the sacroiliac ligaments and the inferior sacral and lumbar spinous processes. Each muscle has its own cephalic insertion point: ribcage and C4-C6 vertebrae; thoracic and cervical transverse processes, mastoid and temporal bones; and upper lumbar and thoracic spinous processes, respectively 9-12.
The thoracic spinal nerves, known as intercostal nerves (T6 to T11) after they emerge from the intervertebral foramen, divide into posterior and anterior branches, innervating muscle structures, joints, pleura, peritoneum and skin of the dorsal and ventral regions of the thorax. Apart from their intercostal course, they have other divisions that traverse the abdomen to provide motor and sensory innervation to the anterior abdominal wall muscles 13.
The ESP block is classified as a block of the fascial plane of the erector spinae muscle. After it is administered, the local anesthetic spreads through the dorsal fascias described above. In the lumbar fascias and the lumbar interfascial triangle, it allows for anterior, posterior, cephalic and caudal spread, involving the ventral and dorsal branches of the spinal nerves, as well as the communicating branches of the sympathetic chain which conduct presynaptic and postsynaptic fibers both in the thoracic as well as the lumbar spine, with the potential of providing visceral and somatic analgesia 1,8,9.
TECHNIQUE
The patient can be sitting or in lateral recumbency 1,14 with the side to be blocked facing superiorly. Several ways to orient the transducer in order to localize the target site have been described. Sagittal paramedian 14,15 and transverse placement 2 using a high-frequency linear probe have been proposed.
In the sagittal paramedian axis, the probe is placed at approximately 3 cm from the midline to localize the transverse process (T5 vertebra for thoracic interventions); it is suggested to begin lateral to medial, initially visualizing the ribs which appear markedly convex with a steeper angle (more rounded or U-shaped); when the transverse process is identified, 3 muscles come into view, namely, trapezius, rhomboid major and erector spinae (Figure 1). The rhomboid major is found only at the T5-T6 level 16. Having localized that view, an "in-plane" injection is performed (Figure 2).
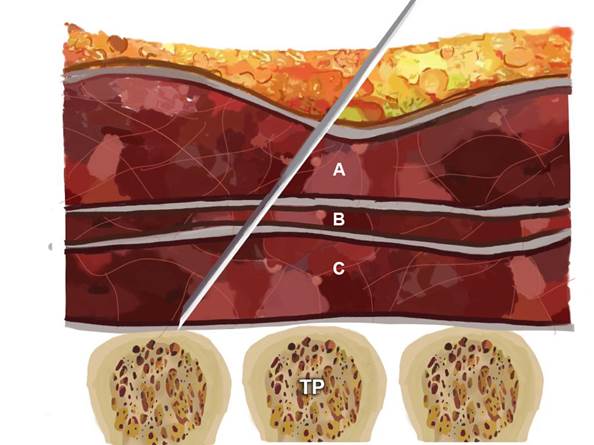
A: trapezius; B: rhomboid major; C: erector spinae plane. TP: transverse process. Source: Authors.
Figure 1 Schematic representation of needle position for the ESP block.
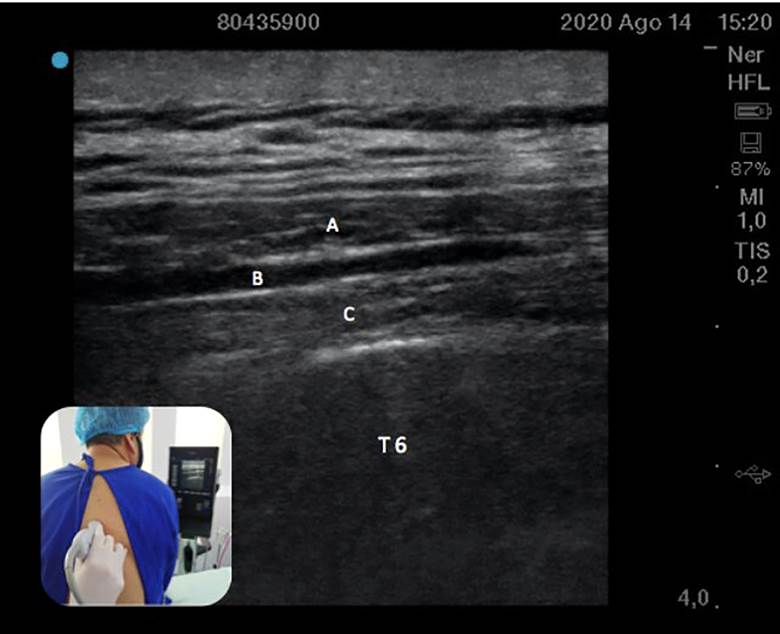
A: trapezius; B: rhomboid major; C: Erector spinae at the level of the transverse process of T6. Source: Authors.
Figure 2 Ultrasound technique and view of the transverse process and the three paraspinal muscles superficial to it, identified from superficial to deep.
The volume of LA varies in the literature. However, in cadaver models, a volume of 20 mL (1,17) to 30 mL 18 has been shown to extend from T2 to T9 when administered on the transverse process of T5 2 (even from C5 to L3)5,18, spanning a mean of 9 dermatomes (range 8-11) in the dorsal area, with 2.2 mL (1.81-2.5 mL) of LA per dermatome required 13; and from T2-T3 to T6-T9 in the anterolateral region, with variable extension to the axillary area and the medial aspect of the arm 19. In children, the use of a volume of 0.6 mL/kg has been reported 14.
CLINICAL APPLICATIONS OF THE ERECTOR SPINAE BLOCK
The technique is apparently safe and easy to implement 4,8; however, there are no studies with large numbers of patients supporting its application in certain conditions. We describe its use in the setting of chronic pain 1-4,18 and cardiac, thoracic, abdominal, breast and limb surgery, with evidence from randomized clinical trials (RCT) in some of these areas 20.
In the original report 1 and in other similar reports 21, the ESP block was performed in adult patients with chronic neuropathic pain (postherpetic neuralgia and chronic neuropathic pain secondary to rib fractures). Later, Forero described a case series in post-thoracotomy chronic neuropathic pain 22, followed by new publications showing favorable results 23, including chronic shoulder pain 24.
In video-assisted thoracic surgery (VATS) for lobectomy, adequate pain modulation has been documented 1. Reports have described the use of this block in cases where epidural analgesia or any other regional technique is more risky 25,26, is contraindicated or is more technically challenging 27. One RCT compared ultrasound-guided ESP block plus intravenous analgesia in 60 patients undergoing VATS. It was found that the use of opioids at 1, 2, 4, 8, 16 and 24 hours, and dynamic and static pain scores at those time points, were statistically lower in the ESP block group (5 patients out of 30) than in the control group (22 patients out of 30) 28. In the latter, the rates of nausea and pruritus were higher and there were no differences between the groups in terms of other adverse effects.
When the serratus plane and the ESP were compared for VATS in 60 adult patients, a significantly lower score for static pain as well as a lower dynamic pain score were found in the ESP group when compared to the serratus plane group 4-6 hours after the intervention. Similarly, the time to first analgesic requirement was longer in the ESP group, with no relevant side effects 29.
Despite its good results, when compared to the paravertebral block (PVB), the ESP block is not as favorable. An RCT published in 2020 30 compared ESP vs. PVB vs. intercostal nerve block (ICNB) in 75 patients undergoing VATS and showed better postoperative pain (POP) control in the PVB group and a higher need for rescue analgesia in the ESP group, with no differences in the comparison between ESP and ICNB. However, pain scores were similar at different POP time points in the three groups.
Thoracotomy for lobectomy
The successful use of this technique as rescue has been reported in cases of failed thoracic peridural analgesia 16. According to some publications, the failure rate of the peridural neuraxial technique ranges between 11.2% 31 and 32% 32; for this reason, the continuous ESP block is an option that offers excellent results in this group of patients. Likewise, the use of this block in two thoracic levels has been described 32, but RCTs showing superiority when compared with single-level injection are needed. Case reports have been described in POP analgesia after thoracotomy for lung transplant 33. In summary, in thoracic surgery, there is support for the use of the ESP block in VATS, thoracotomy for lobectomy, lung transplantation, and as rescue in cases of failed peridural analgesia.
Cardiac surgery
A prospective, randomized study assigned 50 patients to two groups: continuous epidural thoracic analgesia and continuous bilateral ESP block for the management of perioperative pain. Dynamic and static pain scores were similar in both groups at different time points during the first 12 hours; however, after 24 hours and up until 48 hours, pain was lower and statistically significant in the ESP block group when compared to epidural analgesia. There were no differences in ICU length of stay or the need for invasive mechanical ventilation (MV) 34. The ESP block used as part of multimodal analgesia in patients undergoing mitral and/or tricuspid valve repair through right minithoracotomy was analyzed in a case report 35 and also in a cohort study, which found that the time on MV as well as the ICU length of stay were shorter in the ESP block group 36.
An RCT published in 2019 compared bilateral ESP block vs. conventional analgesia in 106 patients undergoing cardiac surgery with by-pass circulation. In the ESP group, ultrasound-guided block at the level of T6 was performed before anesthetic induction. The results showed lower scores on the numerical pain scale (NPS) and longer analgesia duration in the bilateral ESP block group 37.
Spinal surgery
Current evidence is insufficient to support the generalized use of the ESP block; however, cases of its use have been described in spinal cord tumor resection surgery, laminoplasty for spinal canal stenosis 38 and correction of spondylolisthesis, with good results, opioid sparing and no complications 39. To this date, two RCTs 40,41 have been conducted, showing promising analgesic results in lumbar spine surgery, with no adverse effects. Notwithstanding the above, a systematic review carried out in 2020 concluded that the effectiveness and safety of this block for lumbar spine surgery are controversial 42.
Breast surgery
The ESP block has been gaining importance in breast surgery as a result of adequate analgesic response 6 and opioid sparing effect. RCTs comparing the ESP block with other techniques such as PVB 44 or intravenous techniques have been performed in recent years, showing superiority for fascial blocks when compared with intravenous strategies, as well as similar results in terms of pain control and opioid use 45,46.
In radical mastectomy, some RCTs comparing pectoralis nerve block (PECS) vs. ESP block have shown better POP results in the PECS group 47-50. Although no differences have been reported 51 when comparing the ESP and paravertebral blocks in terms of POP opioid use at 24 hours, pain scores, or PONV, shorter localization time by anesthetists with 44 or without 52 experience in regional techniques has been described in the case of the ESP block. Moreover, a comparison between the ESP block and intravenous analgesia 53 showed significantly lower POP morphine use and lower scores on the numerical pain scales in the first 4 hours in patients receiving the ESP block 54.
One RCT 55 compared the quality of POP recovery in patients taken to modified radial mastectomy using LA vs. placebo, with better quality of recovery in the group assigned to the LA technique according to the QoR-15 questionnaire. A systematic review and meta-analysis 47 found that, in this surgical model, the ESP block offers superior analgesia and lower POP oral morphine use when compared to no use of regional techniques, as well as similar analgesic effects as those of the PVB, with absent risk of pneumothorax and other complications. The dose and useful anesthetic concentration are not clear yet; however, a recent RCT 56 compared two anesthetic concentrations in the ESP block, showing that 0.375% bupivacaine concentrations offer better analgesic results than 0.25% concentrations.
In other surgical models such as reduction mastectomy, a double-blind RCT 57 of 44 women comparing tumescent anesthesia vs. ESP block in terms of POP analgesia requirement, pain scores and patient satisfaction showed that the use of tramadol was significantly lower in the ESP block group as was also the case with pain scores at several time points during the first 24 hours and the need for additional analgesia, with improved patient satisfaction.
Considering that the erector spinae muscle extends towards the inferior spinal region, the ESP block at the level of T7-T8 allows the spread of the anesthetic mix to the inferior thoracoabdominal nerves that provide abdominal innervation. Moreover, the mechanism of action includes penetration of the LA into the paravertebral space, with action on the ventral and dorsal branches as well as the communicating branches containing sympathetic nerve fibers, thus providing sensory, somatic and visceral blockade in abdominal surgery 2. Against this backdrop, a report of 3 patients taken to laparoscopic bariatric surgery with adequate analgesic response to the ESP block has been described 2. Lower opioid requirements have been reported in case series 7,58 using this technique in patients undergoing laparoscopic ventral hernia repair 2 and in different laparoscopic surgery models.
Laparoscopic cholecystectomy
Three RCTs have been found: the first 59 with 76 patients, comparing the ESP block vs. transversus abdominis plane (TAP) block, showed that the POP use of tramadol and pain scores were significantly lower in the ESP group. The second study compared the same regional techniques in 72 patients in terms of the NRS score, paracetamol and tramadol consumption and the need for rescue analgesia 60 and it showed that pain intensity was similar between the two groups in the first 3 hours, while the consumption of additional analgesics was comparable. A third RCT 61 with 36 patients compared the ESP block vs. multimodal analgesia and showed that pain on the NRS was lower in the ESP block group during the first 3 hours, with no differences after that time; in turn, tramadol consumption and additional analgesic requirements were lower in the ESP group. These conclusions were also supported by a meta-analysis 62.
Lower abdominal surgery
In lower abdominal surgery, particularly in gynecological surgery for cesarean section, one case of bilateral ESP block for effective and lasting POP analgesia in a patient taken to an emergent procedure under general anesthesia 63 was found. Another case described a male patient taken to major abdominal surgery (open radical cystoprostatectomy) who received continuous analgesia with bilateral ESP block with very good analgesic results 64.
Pediatric patients
In these patients, the ESP block appears to be a safe and effective analgesic option, especially in thoracotomy 3,14,65. In other thoracic surgery models, the use of the ESP block has been described in pediatric patients undergoing pectum excavatum and pectum carinatum correction with scores on the visual analog scale lower than 4 and absence of intraoperative and long-term postoperative opioid requirement 66. Likewise, case series 67 of pediatric patients described laparoscopic cholecystectomy with regional analgesia provided by the ESP block, showing adequate POP pain control and patient satisfaction. Also, a case report 68 described the use of a single-dose ESP block as anesthetic method for inguinal hernia repair in a two-month-old patient (born at 29 weeks of gestation) weighing 2.5 kg, with hemodynamic stability during the 35 minutes of the procedure, oral intake tolerance over the following 6 hours and a pain score of 0 on the FLACC (Face, Legs, Activity, Cry, Consolability) scale over the next 24 hours.
Lower extremities
Finally, in surgery involving the lower limbs, some published case reports show potential analgesic effectiveness of the ESP block, considering LA spread to the lumbar plexus, in surgical models such as hip arthroplasty 69 and knee arthroplasty 72; however, studies of better methodological quality are needed in order to arrive at a conclusion regarding the role of the ESP block in these procedures.
COMPLICATIONS
The ESP block appears to avoid the types of complications that can arise with the use of other regional techniques, including hypotension, permanent spinal cord injury and urinary retention with epidural analgesia, epidural spread, vascular puncture in PVB, and pneumothorax in intercostal nerve blocks and PVB 8,47. However, cases of pneumothorax 73 and priapism 74 have been reported in two patients subjected to the ESP block.
One case of motor blockade was recently described as an unexpected side effect of the ESP block in a patient undergoing cesarean section who refused neuraxial techniques 75. During her stay in the postanesthetic care unit (PACU), bilateral motor weakness and sensory deficit between the T9 and L3 dermatomes were documented. Motor strength began to return after 13 hours, with complete resolution at 16 hours. The authors of this case propose LA infiltration into the lumber plexus as the first explanation, or spread through the epidural space, considering that, on neurological examination, the patient showed weakness of the psoas, iliac and quadriceps muscles, confirming compromise of the spinal nerves at L1, L2 and L3, and of the femoral nerve.
The absence of important blood vessels and neural structures in immediate proximity minimizes concerns regarding the development of clinically significant hematomas. However, until more clinical data are available, caution is recommended in patients with coagulation disorders or who are receiving perioperative anticoagulation 76.
Although complications have been described generally with the in-plane ultrasound-guided approach, the use of the ESP with the out-of-plane approach using the convex transducer for hip (69), shoulder, thoracic, breast and abdominal surgery has shown a similar rate of efficacy and complications 77.
CONCLUSION
The ESP block is presented as an effective analgesic management option in anesthesia and should be considered as part of the multimodal analgesia strategies on the basis of its good analgesic results, low incidence of complications and less side effects when compared with epidural analgesia, and its wide applications in different surgical models. Therefore it may be considered as a safe, simple and optimal analgesic alternative 1,3,8.
Larger studies and more in-depth research are required in order to gain more insight into the mechanism of action, side effects and duration of the effects of this intervention.











 text in
text in 



