What do we know about this problem?
Prevention, identification and analysis of adverse events and mitigation of their effects are strategies that help improve safety in healthcare.
The legal claims study (closed claims) serves as a source to identify patient safety-related problems.
International studies show a trend towards an increase in adverse events in non-surgical procedures, and the main events involve the respiratory system and regional anesthesia.
What is new about this study?
The largest number of adverse events was found in association with surgical procedures, mainly in plastic surgery; most frequently involving the cardiovascular system.
AEs were associated with anesthesiologists age over 60 years, failure to adhere to certain standards, and anesthesiologists absence during the event.
INTRODUCTION
Safety is a principle in healthcare, as well as a quality domain 1,2. However, adverse events (AEs) result from care which caused harm unintentionally. With a prevalence of 10%, it is a situation inherent to the provision of healthcare services 3. In Colombia, according to the IBEAS study 3, AE prevalence is 13.1%.
A large proportion of studies on this topic have used AE incidence as an estimate of safety issues and the impact on morbidity and mortality, highlighting AEs as a relevant public health problem. AE prevention, identification and analysis, as well as mitigation of their effects, are strategies that can help increase patient safety 4.
Completed claims or closed claim analysis is one of the methods used to identify near misses and AEs 5. Different projects have been developed using this analysis strategy in the case of anesthesia, the first being the Closed Claims Project of the American Society of Anesthesiology (ASA) 6, whose findings still stand and which was crucial for understanding AEs and anesthesia-related risks 7.
Considering the impact of AEs on the health of our population, the aim of this study was to analyze EAs found in closed medicolegal claims against anesthesiologists affiliated to an insurance fund between 2013-2019, in order to gain insight into the current status of this occurrence and guide the implementation of improvement actions as well as education, promotion, and prevention strategies targeted to healthcare staff in order to help improve safe care.
METHODS
Descriptive observational cross-sectional study. Data were gathered from the records of an insurance fund for the period between January 2013 and July 2019. Convenience non-probabilistic sampling was used, including all closed claims in which the affiliated anesthesiologists were a party to the medicolegal proceedings during the observation period. Cases in which the claim was not related to an AE and those in which the event was not anesthesia-related were excluded.
The information pertaining to the medical intervention and the claim was sent in digital format to two anesthesiologists with more than 20 years of experience who analyzed the cases independently between July and December 2020 and entered the information in a form prepared for that purpose on the Question Pro platform. The variables included were patient-related (age, gender, ASA classification, comorbidities); procedure-related (scheduling modality, specialty, anesthetic technique, time of day, duration); AE-related (place of occurrence, time of occurrence, organ system involved, degree of harm caused to the patient, AE outcome, demonstrable link between the AE and anesthesiologists management, and event preventability) 8; and practitioner and work niche-related (practitioner age, preoperative assessment, clinical record entries, compliance with safety standards, other professionals involved, administrative processes, compliance with standards, guidelines and protocols, coordination, leadership or communication issues among professionals).
For data analysis, qualitative variables were described as absolute and relative frequencies, and quantitative variables were described as central trends and scatter in accordance with their distribution. The STATA v13 software was used for the statistical analysis.
The study protocol was reviewed and approved by the Bioethics Committee of the Universidad de Caldas Health Sciences School, as set forth in Minutes N.° 011 of July 6, 2020.
RESULTS
Claims
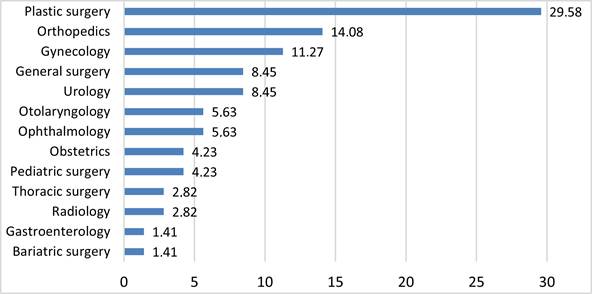
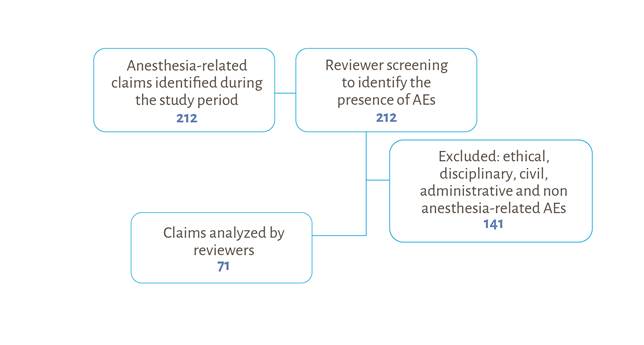
Out of 212 claims filed during the study period, 33.5% (n = 71) that met the selection criteria were included (Figure 1).
Source: Authors.
Figure 1 Diagram of claims identified as anesthesia-related filed against S.C.A.R.E. members between 2013 and 2019.
Table 1 shows claims characterization in terms of patients, procedures, AE, practitioner involved and area of work.
1 Results of the variables of greatest interest in claims associated with AEs.
Source: Authors.
Out of 71 AEs, 78% were elective surgery-related, 71.8% with surgeries performed in the operating room and 81.7% with procedures lasting less than 3 hours; 64.8% were considered preventable and, most often, the degree of harm to the patient was death, in 43.7% of the cases (Table 1).
Figure 2 shows the specialties corresponding to the procedures associated with the claim, plastic surgery being the most frequent at 29.6%.
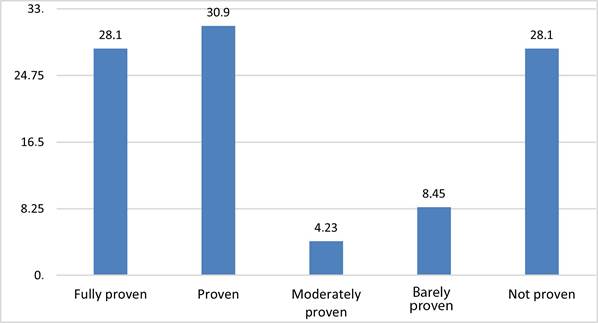
The analysis of frequency of failure to comply with standards, guidelines or protocols (Figure 3) showed "proven" or "fully proven failure" in 30.9% and 28.1% of cases, respectively.
Table 2 summarizes AEs and the system involved, the most frequent being the cardiovascular system, with cardiac arrest. In terms of AE outcomes, 43.7% (n = 31) led to patient death; 28.1% (n = 20) to brain damage; 15.4% (n = 11) to emotional disorders or sequelae; 9.85% (n = 7) to peripheral nervous system injury, and 2.81% (n = 2) to laryngeal dysfunction/ injury. Brain damage was considered to be severe in 85% (n = 17) of cases and peripheral nervous system injury was considered permanent in 28.6% (n = 2). In 64.8% (n = 46) of cases it was found that AEs could have been prevented, and the degree to which the anesthesiologists was implicated in the AE was evident in at least 67.6% (n = 48) of cases.
Table 2 Most frequent adverse events (%).
| Related system | Causes % | |
|---|---|---|
| Cardiovascular system (43%) | Cardiac carrest | 59.4 |
| Severe bradycardia | 15.7 | |
| Hypotension | 4.7 | |
| Pulmonary thromboembolism | 4.7 | |
| Shock | 3.1 | |
| Other* | 12.4 | |
| Respiratory system (23%) | Desaturation (hypoxemia) | 30.1 |
| Respiratory depression | 12.2 | |
| Respiratory distress | 10.2 | |
| Difficult airway/intubation | 10.2 | |
| Pulmonary edema | 10.2 | |
| Pneumothorax | 6.1 | |
| Aspiration | 4.1 | |
| Pulmonary thromboembolism | 4.1 | |
| Airway obstruction | 4.1 | |
| Other** | 8.7 | |
| Central nervous system (13%) | Delayed awakening | 23.1 |
| Seizure | 15.4 | |
| Compromised state of consciousness | 15.4 | |
| Spinal cord injury | 7.7 | |
| Hypoxic encephalopathy | 7.7 | |
| Pontine myelinolysis | 7.7 | |
| Spinal hematoma | 7.7 | |
| Other*** | 15.3 | |
| Medications (7%) | Unsafe administration | 62.5 |
| Adverse reaction | 25.0 | |
| Anaphylaxis | 12.5 | |
| Regional anesthesia (3%) | Peripheral neuropathy | 60.0 |
| Brachial plexus injury | 20.0 | |
| Peripheral nerve injury | 20.0 | |
*Other: massive bleeding, arrhythmia, cardiac dysfunction, hypovolemia, anaphylaxis, collapse, central catheter guidewire loss, syncope.
**Other: orotracheal tube obstruction, monobronchial intubation, inadequate ventilation, fat embolism, laryn-geal foreign body.
***Other: wrong drug administered in the subarachnoid space, hyperthermia, cranial nerve injury, amaurosis.
Source: Authors.
Practitioner and work niche characterization
Anesthesiologists mean ages at the time of the AE was 48.4 years (SD: 12.7). At the time of AE occurrence, 74.6% (n = 53) of the anesthesiologists were between 30 and 60 years of age. When comparing claims in which an AE occurred versus those where there was no AE by age groups, if was found that in 63.3% (n = 14) of the cases in which an adverse event occurred, the anesthesiologists was over 60 years of age.
No preoperative assessment was performed in 18.8% (n = 13) of the cases with AE occurrence; in 59.2% (n = 42) of cases, failures in clinical record entries had been demonstrated or fully demonstrated; and anesthesiologists failure to comply with minimum safety standards was found in 35.2% (n = 25), the most frequent failures being absent informed consent (n = 15; 60%), absent preoperative assessment (n = 13; 52%), absent anesthesiologists at the time of the AE (n = 5; 20%), and insufficient monitoring (n = 5; 20%).
In 52.1% (n = 37) of the cases there were other professionals involved in the AE besides the anesthesiologists: surgeon (n = 28; 61.4%), licensed practical nurse (n = 8; 15.9 %), another anesthesiologists (n = 7; 9%), registered nurse (n = 3; 6.8%).
In terms of factors associated with the work niche, evidence of potential flaws in administrative processes was found in the reviewed documents for 33.8% (n = 24) of cases. Evidence of coordination, leadership or communication issues among professionals was found in 38% (n = 27) of cases.
DISCUSSION
In this characterization of AEs that resulted in medicolegal claims - already closed - filed between 2013 and 2019 against anesthesiologists affiliated to an insurance fund, a substantial number of AEs occurring during elective surgical procedures lasting no more than 3 hours were identified.
Also described is a group of affected patients, most of whom (78.9%) were considered healthy, with an ASA classification of I to II, and relatively young - mainly under 40 years of age (60.6%). It is worth noting that age, comorbidities, ASA classification, the type of surgery (elective or urgent), the length of the procedure and positioning during surgery are all factors related to anesthetic risk 9,10, factors which were not very relevant in the analysis of procedure and patient characteristics. These findings are consistent with those of other studies 11-13 that have found lower attention to care standards when patients and procedures are considered low risk; moreover, it is important to take into account that claims are more frequent in patients in whom no complications or AEs were expected 11,13.
A considerable proportion of AEs occurred in plastic surgery procedures. This high number can be attributed to the boom of plastic surgery in Colombia, compounded by inadequately managed risk factors that contribute to a higher risk of complications or adverse events, including long procedures, several procedures at a time, unidentified or inadequately managed thromboembolic risk factors, patients with a high risk for the type of surgery, failure to comply with standards, guidelines and protocols, particularly those related to preoperatory assessment, lack of training and expertise by the surgeon, and institutions with insufficient resources and protocols for the management of those types of procedures 14,15.
Although AEs continue to be much more frequent in surgical procedures, international studies in recent years show a trend towards significant numbers of cases associated with the management of chronic and acute pain 7,12. In the ASA closed claims study, claim profiles changed as of 1990, when the numbers related to anesthesia in the operating room dropped to 72% while claims associated with acute and chronic pain accounted for 11%. By 2007, claims due to chronic pain management rose to 18%, while claims involving anesthesia in the operating room dropped to 65% 7,13. This trend was not observed in this study, where 95.8% of adverse events were associated with surgical procedures. These findings could be explained by the low number of anesthesiologists working in pain management in Colombia, the small number of invasive procedures associated with acute and chronic pain performed by anesthesiologists, and the fact that as practitioners they are still "operating room anesthesiologists" and not "perioperative physicians".
In this study, the majority of adverse events resulted in death or brain injury, unlike the ASA closed claims study in which, although death continues to be the main complication and the main driver, it only accounts for 26% of cases. In this report, nerve injury accounts for 22% of claims, while the third cause leading to lawsuits was permanent brain damage (9%) 7,13.
Cardiovascular-related events continue to be the most frequent in the claims analyzed, while in other settings the most frequent events are related with regional anesthesia 7,12 or the respiratory system 16. In the most recent closed claims studies conducted by the ASA, the events most commonly resulting in claims due to anesthesia-related injuries or complications involved regional anesthesia, accounting for 20% of the claims. Events involving the respiratory system account for 17% of the claims, while cardiovascular events account for 13% 7,17.
In different studies, the most frequent events related to the cardiovascular system are bleeding, arrhythmia and hemodynamic instability 12,16; in this work, cardiac arrest was the most frequent. This is a source of concern because cardiac arrest may often be attributed to human error as a result of equipment monitoring failures, lack of surveillance and negligence 16. In this study, the most frequent events associated with the respiratory system were hypoxemia, respiratory depression, respiratory distress and pulmonary edema. In contrast, the most frequent events reported in international studies are aspiration, inadequate ventilation and difficult intubation 12,16. Among AEs involving the central nervous system, the most frequent is delayed awakening. Unlike the findings in international studies where intraoperative awakening is a relevant event, no cases of such an event were found in this study 16.
Regarding practitioner characteristics, claims in which anesthesiologists over the age of 60 were involved were related with the presence of an adverse event to a significant proportion. The literature shows that, compared to anesthesiologists under the age of 51 years, anesthesiologists over the age of 65 are involved in 50% more claims-related cases and almost twice the number of cases associated with severe harm to the patients 18.
However, in this study, adverse events related with anesthesiologists between the ages of 30 and 60 predominate. Practitioner-related factors such as the level of training and expertise influence the occurrence of potential errors, but also important are other factors such as fatigue and physical and mental health 19. A study carried out among anesthesiologists reported human error in 82% of cases of preventable AEs, the causes of such errors being practitioner lack of experience, lack of familiarity with the equipment or the material, ineffective communication with the team, urgency in task performance, lack of attention, and fatigue 16,20.
Evidence of non-compliance with standards and anesthesiologists absence during the AE was also found. It is worth noting that despite the existence and relevance of recommendations such as those contained in the S.C.A.R.E.'s Minimum Safety Standards 21, percentages of failed clinical record documentation and non-compliance with the standards are still high in claims cases. Different studies show that the lack of training, the absence of professional monitoring, resistance to the implementation of guidelines and protocols, and poor patient monitoring by the practitioner are critical factors that contribute to AE occurrence 16. These results are similar to those found in the S.C.A.R.E study 11.
Comparing the results described here with those obtained by Bocanegra et al. 11, the main difference is the increase in the number of claims per year: in the 2016 study, the average number of claims was 19.4 per year for the period between 1993 and 2016, while the average for the period between 2013 and 2019 was 35.3 claims/year; also of note is a drop in the percentage of claims involving AEs (75% for 1993-2006 vs. 33% for 2013-2019). This increase is associated with claims involving ethical, disciplinary, administrative and non anesthesia-related AEs, all of which were excluded from the analysis. There is yet another difference in this previous study 11, where the highest number of AEs occurred in association with obstetrics and gynecology, general surgery and orthopedic procedures.
An analysis of the human factors contributing to respiratory system-related AEs included failure to anticipate risks, incorrect decision-making in emergency situations, work environment factors -such as low staff availability and work under pressure - and personal factors such as fatigue and stress 16,22. The fact that in more than 50% of cases there was another healthcare professional involved in the AE speaks to shared responsibility and the need to improve soft skills such as communication and team work. Problems with the exchange of patient information among professionals or with the patient and family, and the lack of teamwork at critical times are factors that contribute to the occurrence of AEs 16. Recent studies highlight the importance of building soft skills such as communication, teamwork, situational awareness and avoidance of biases and cognitive errors in order to improve safety in clinical practice 7,16.
Anesthesia is a complex specialty which requires the development of technical skills and the ability to make decisions in critical situations as well as adequate planning of care by a multidisciplinary team in order to control risk and avoid the occurrence of adverse events 16. Various studies show that AEs in anesthesia are related with human error: active planning or execution errors and latent failures involving organizational structure. The literature shows that failures in anesthesia are due to lack of attention, inadequate care planning, work environment constraints, flawed clinical judgement, late identification of patient changes, failed decision-making, physical and emotional factors such as fatigue and stress 16,23. Environmental factors also affect work performance and these include things like the physical characteristics of the work space, interpersonal relationships among peers, and workplace environment 19.
These conditions that influence work teams do not occur in a vacuum and depend on organizational leadership mandates. They include the economic and regulatory context, relations with external organizations, temporary employment hiring policies, continuing education, training, supervision, and availability of equipment and supplies 19. Organizational factors such as having to perform activities under pressure and achieve greater productivity, as well as long or intense working hours, can contribute to the development of stress and fatigue 19. One study showed that in 28.2% of the cases in which anesthesia-related errors were involved, fatigue was found to be an important cause, as it affects performance and leads to lower quality of care 16,24.
In view of the above, healthcare professionals need support from their organizations in order to improve their performance. Such support involves training and improved working conditions. Education must include training in technical as well as soft skills and the provision of tools designed to enhance the quality and safety of their actions. Working conditions could be improved by creating respectful organizational environments, including the implementation of fatigue management systems and improved communication programs 16.
For S.C.A.R.E, closed claims analysis is a method which, despite its limitations (retrospection bias, information bias, non-standardized data sources), allows to obtain information pertaining to anesthesia-related AEs as it detects latent errors and provides multiple perspectives regarding AEs, particularly when they are not accounted for, as is the case in Colombia, as part of a national anesthesia-related near-miss and adverse event reporting system 25,26. A limitation of this study is that AEs share the essential characteristic of having been identified because of a medicolegal claim. This situation may constitute a bias since there are features or characteristics that distinguish them from those adverse events that did not result in a medicolegal claim; there is a difference which is not random and does not allow adequate causality evaluation due to the inability to identify all adverse events and their associated factors. On the other hand, the incidence and risk of anesthesia-related adverse events are unknown given the absence of a numerator corresponding to the total number of AEs and a denominator corresponding to the total number of anesthetic procedures performed 5,27. Future research will require the use of more diverse sources of information in order to overcome the limitations and biases of this study and evaluate the impact of improvement strategies.
In conclusion, when comparing this study with a prior study conducted by S.C.A.R.E., there is an increase in the number of ethical, disciplinary, and administrative claims not directly related with the practice of anesthesia. The majority of anesthesia-related AEs involve surgical procedures performed in the operating room as well as patients and procedures categorized as low-risk; of these, plastic surgery is the specialty associated with the highest number of AEs. The majority of the events occur in patients and settings considered low risk, which is consistent with what the literature describes and with the results of a previous study conducted by S.C.A.R.E. Most AEs lead to death and permanent brain damage, and the majority involve the cardiovascular system, cardiac arrest being the most frequent. The majority of AEs are considered preventable and this study has found an association between AEs and failure to comply with standards and absent anesthesiologists during the event.
A higher degree of commitment from professionals, institutions and scientific societies is required in terms of developing, tracking and evaluating care guidelines and protocols in order to guide and support practitioner decision-making in daily practice; promoting initiatives designed to develop soft skills that improve the safety culture and institutional processes; and providing education to patients to empower them for self-care and active participation in their care process.
ETHICAL RESPONSIBILITIES
Ethics Committee endorsement
The study received the endorsement from the Bioethics Committee of the Universidad de Caldas Health Sciences School as stated in Minutes N.° 011 of July 6, 2020.
Animal and human protection
The authors declare that no animal or human experiments were carried out as part of this research. The authors declare that the procedures used were in compliance with the ethical standards of the Responsible Human Experimentation Committee, the World Medical Association and the Declaration of Helsinki.
ACKNOWLEDGEMENTS
Authors' contributions
JCBR: Project conception, study planning, research protocol construction, data collection, discussion of the results obtained, writing, review and approval of the final manuscript.
LMGB: Project conception, study planning, research protocol construction, discussion of the results obtained, writing, review and approval of the final manuscript.
NFSB: Study planning, research protocol construction, statistical analysis of the results obtained, discussion of the results obtained, writing, review and approval of the final manuscript.
ACV: Project conception, data collection, writing, review and approval of the final manuscript.











 text in
text in