What do we know about this problem?
Mortality rates in high perioperative risk populations vary at the present time as a result of diverse characterizations and heterogenous research designs applied to these statistical calculations.
Timely intervention of postoperative mortality risk factors provides opportunities to improve overall perioperative care.
What is new about this study?
Based on specific inclusion criteria, which essentially determine admission to the high perioperative risk program, and using close concurrent and longitudinal follow-up, mortalities were estimated with high validity in a specific population which is the subject of growing research.
Likewise, specific risk factors of high epidemiological weight were identified as a result of painstaking and judicious statistical analysis.
INTRODUCTION
From the perspective of the anesthetist, perioperative risk determination is part of the strategies aimed at reducing disease-related morbidity and mortality, physiological reserve conditions and the burden imposed by surgery 1. Preanesthesia assessment provides the opportunity to formulate individualized perioperative strategies involving the patient, the family and the healthcare team 2.
Historically, the groups with the highest disease burden and/or undergoing higher risk procedures have contributed to mortality to a greater degree. In 2006, Pearse and his team of researchers in the United Kingdom described minority patient groups (12.3%) as accounting for up to 83.4% of deaths. These groups comprised elderly patients, patients with multiple chronic and severe comorbidities, and patients taken to major procedures. Not only was mortality higher than 5%, but these patients were considered as a selected independent factor associated with mortality 3.
From the clinical perspective, several scales for assessing morbidity and mortality risk have been developed. These include the American Society of Anesthesiologists (ASA) physical status classification 4, Lee's revised cardiac risk index 5 and the physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM). The latter was described in 1991 6 and validated for multiple types of surgical procedures 7-10. Nonetheless, there is still a paucity of multidimensional approaches for assessing high risk and studying its effects.
In Colombia, there is very little literature regarding patients in this subgroup. In 2005, Oliveros et al. studied mortality risk factors in high-risk surgical patients admitted to postoperative intensive care 11. In their article they defined at least four domains that identify an increased risk of complications: 1) inherent to patient functional status; 2) inherent to the surgery itself; 3) inherent to the acute disease leading to the procedure; and inherent to the medical and surgical environment in which the surgery takes place. These variables have been useful for defining high risk at a regional scale. However, neither high-risk patients who were not initially admitted to the intensive care unit (ICU) after surgery, nor those who died during surgery were analyzed.
In view of the multiplicity of definitions found until 2008, the Anesthesiology Department of La Samaritana (HUS) University Hospital embraced and standardized various criteria. As of 2009, it defined four domains as criteria for admission to its high risk program: age, functional status, comorbidities and type of procedure. This information is summarized in Table 1 and it is the result of the academic, research and clinical work published by Mena, Pérez and Oliveros in 2013 12.
Table 1 Admission criteria for high perioperative risk patients at HUS.
| Factor | Variable | Reference criterion |
|---|---|---|
| Age | Age (in years) | > 60 years |
| Functional status | ASA (American Society of Anesthesiologists classification) | > III |
| Functional class | < 4 MET | |
| Comorbidities | Cardiovascular
|
Lee index > 2 Severe arrhythmia Severe valve disease |
| Renal | Creatinine > 2 mg %, BUN>40 | |
| Nutritional status | Albumin < 3, BMI < 17 or > 30 | |
| Type of procedure | General surgery | Esophagectomy Gastrectomy Colectomy Pancreatic resection Gastric bypass |
| Thoracic surgery | Pneumonectomy | |
| Vascular surgery | Major vascular surgery | |
| Orthopedics | Major hip reconstructive surgery |
BMI: body mass index; CHF: congestive heart failure; MET: Metabolic equivalents; TIA: transient ischemic attack.
Source: Authors.
Given the lack of consensus regarding a specific and universal definition of high perioperative risk patients, with robust epidemiological support, as well as the lack of effective identification of factors associated with in-hospital perioperative morbidity and mortality, the purpose of this study was to determine postoperative mortality and its associated factors in high perioperative risk patients. The high surgical risk cohort in the high perioperative risk program of the Anesthesiology Department of a high complexity hospital in Colombia was used.
METHODS
Analytical observational study in a cohort of patients admitted to the high perioperative anesthesia risk program of a high complexity hospital in Colombia. For inclusion, patients had to meet at least two high-risk criteria determined in advance, and which are shown in Table 1. All the records of the cases seen and followed between January 2011 and April 2018 were collected and analyzed. No exclusion criteria were established, except for the finding of incomplete records. Sample size was not estimated considering that all valid records within the observation window were included.
The information collected in the High Perioperative Risk database was subjected to a double cross-check, based on data entered by specialists and by medical residents rotating in the program (previously trained), and also revalidated by the research group conducting this research. Demographic, clinical and outcome variables were tabulated in accordance with the protocol and sorted by origin (preoperative, intraoperative and postoperative).
Overall cohort mortality and stratified mortality for high cardiovascular risk were estimated as primary outcomes. For these outcomes, cumulative mortality was defined as every death occurring within the first 7 and 30 postoperative days. Likewise, high cardiovascular risk mortality was defined as deaths occurring in the subgroup of patients with severity criteria for cardiovascular disease (Lee index greater than 2).
Descriptive statistics were used for the demographic description of the population: absolute frequencies and percentages for qualitative variables, and central trend (means/medians) and scatter (standard deviation [SD]/inter-quartile range 25%-75% [IQR]) in accordance with quantitative data distributions. Bivariate analysis was used for mortality, and odds ratios (OR) and 95% confidence intervals (95% CI) were estimated The bivariate analysis for overall and stratified mortality was carried out using Ji2 for qualitative variables. A logistic regression model was then applied to adjust the effect of potential confounding variables and estimate an explanatory model in each group of variables. Finally, overall and stratified survival graphs (Kaplan Meier) were calculated and analyzed by means of contrast hypothesis using the log-rank test. Likewise, a Cox regression model was developed with multiple preoperative variables. The SPSS 25 statistical software package was used for the statistical analysis. Statistically significant differences were considered to exist with a significance of less than 5% (p less than 0.05).
The research protocol was approved by the Graduate Research Subcommittee of La Sabana University Medical School and by the Technical and Ethics Committee of the Samaritana University Hospital Research Center (Minutes 110118 of December 13, 2018).
RESULTS
Overall, 843 records of patients in the high risk program were included. All patients were followed for at least 30 days, as an inclusion criterion; however, the vast majority were followed over several months after the date of the surgery.
The demographic description and the clinical characteristics of the population are shown in Tables 2 and 3. A similar distribution was observed for both genders (female 50.3%), and mean age was 68 years (IQR 25%-75% between 54 and 79), although predominance of records of patients over 60 years (65.4%) was relevant. It is worth noting that the reason for surgery was infection (12.2%), or oncologic disease (16.7%) or an emergency (12.7%). At least one comorbidity was found in 90.4% of cases, and two or more in 77.8%, the most frequent comorbidity being arterial hypertension (69.5%); 15.3% of patients were obese (71.7% of them being morbidly obese).
Table 2 Demographic characteristics*.
| Variable | Values |
|---|---|
| Age (years) | 68 (54-79) |
| Sex (female) | 424 (50.3%) |
| Comorbidities (%) - Two or more |
762 (90.4%) 656 (77.8%) |
| ASA 2 (%) ASA 3-4 (%) ASA 5 (%) |
128 (15.2%) 710 (84.2%) 5 (0.6%) |
| Obesity - Morbid |
129 (15.3 %) 91/129 (71.7 %) |
*(n = 843) Values expressed as medians (and inter-quartile ranges at 25%-75%), or frequencies (and percentages). ASA: American Society of Anesthesiologists Classification.
Source: Authors.
Table 3 Clinical characteristics*.
| Variable | Valores n (%) |
|---|---|
| Comorbidities - Arterial hypertension - Valve disease - Coronary heart disease - Arrhythmia - Moderate-to-severe ventricular dysfunction - Chronic obstructive pulmonary disease - Pulmonary hypertension - Moderate-to-severe pulmonary hypertension - Diabetes mellitus type 2 - Hypothyroidism - Dyslipidemia - Chronic renal disease - Cerebrovascular events |
762 (90.4 %) 586 (69.5 %) 273 (32.4 %) 176 (20.9 %) 162 (19.2 %) 107 (12.7 %) 221 (26.2 %) 194 (23.0 %) 155 (18.4 %) 196 (23.3 %) 99 (11.7 %) 86 (10.2 %) 147 (17.4 %) 84 (10.0 %) |
| Medications - Betablockers - Alpha-2 agonists - Statins |
390 (46.3 %) 88 (10.4 %) 451 (53.5 %) |
| Scales - FC < 4 MET - NYHA-FC III-IV - High surgical risk (Johns Hopkins) - Lee's revised cardiac risk index > 2 |
100 (11.9 %) 116 (13.8 %) 301 (35.7 %) 222 (26.3 %) |
*(n = 843) Values presented as medians (and 25-75% inter-quartile ranges) or frequencies (and percentages).
FC = functional class measured in metabolic equivalents; NYHA-FC = New York Heart Association functional class.
Source: Authors.
Cumulative mortality in the first 7 days was 3.68% (95% CI 2.40-4.95%) and 10.08% at 30 days (95% CI 8.05-12.12%). Likewise, 7-day cumulative mortality for the high cardiovascular risk population was 3.60% (95% CI 1.13-6.07%) and 30-day mortality was 14.86% (95% CI; 10.1519.58%), with significant differences at 30 days as compared to mortality in the group without high cardiovascular risk (8.37%; p = 0.005), but not at 7 days (3.70%; p = 0.56).
No significant differences were found for 7-day cumulative mortality for the period 2011-2014 (3.4%) versus 2015-2018 (3.9%) (p = 0.428). Also, no significant differences were found for 30-day cumulative mortality for the period between 2011-2014 (11.5%) versus 2015-2018 (8.7%) (p = 0.110). Likewise, no significant differences were found when assessing 7-day cumulative mortality for the high cardiovascular risk population in the period between 2011-2014 (2.6%) versus 2015-2018 (4.7%) (p = 0,312); and no significant differences were found either when assessing 30-day cumulative mortality for the period between 2011-2014 (16.4%) versus 2015-2018 (13.2%) (p = 0.318).
In the analyzed cohort, 90.4% of patients had at least one comorbidity, being arterial hypertension and valve disease being the most prevalent (69.5% and 32.4%, respectively); 11.9% of patients had a functional class under 4 MET, and 35.7% of the procedures were considered high surgical risk; 26.3% of the patients were in group II or higher of Lee's revised cardiac risk scale which, at the time of the bivariate analysis (p = 0.006) conferred them a 30-day mortality OR of 1.91 (95% CI; 1.19-3.04), but it was not significant for 7-day mortality (p = 0.94).
Known mortality risk factors were analyzed in the high-risk patient cohort. This was done by means of bivariate analyses developed in accordance with the nature of the factor, its significance and OR (95% CI). Those which were found to have statistical significance were included in Table 4 for preoperative conditions, and in Table 5 for postoperative outcomes. Models were built with manual inclusion (intro) and forward for mortality risk factors (p < 0.1) in the preoperative and postoperative domains. Preoperative modeling resulted in an R2 explanatory model of 17.8% for 7-day mortality and 19.4% for 30-day mortality. Likewise, in the postoperative modeling, a predictive model with explanatory R2 of 16.3% was obtained for 7-day mortality and of 30.7% for 30-day mortality (Table 6).
Table 4 Crude association between preoperative variables and 7 and 30-day mortality*.
| Variable | 7-day mortality OR (95% CI) p value | 30-day mortality OR (95% CI) p value |
|---|---|---|
| Age > 60 years | 3.71 (1.28-10.70) 0.01 | 5.03 (2.48-10.19) < 0.0001 |
| Hip fracture | 3.66 (1.70-7.86) < 0.0001 | 2.43 (1.43-4.14) 0.001 |
| Chronic obstructive pulmonary disease | 4.78 (2.28-10.02) < 0.0001 | 3.15 (2.00-4.99) < 0.0001 |
| Valve disease | 2.30 (1.12-4.73) 0.02 | 1.29 (0.81-2.06) 0.27 |
| Functional class < 4 MET | 4.32 (1.84-10.16) < 0.0001 | 5.24 (2.93-9.35) < 0.0001 |
| Johns Hopkins intermediate surgical risk | 2.28 (1.08-4.82) 0.02 | 1.57 (1.00-2.47) 0.046 |
| ASA-PS > II | 1.045 (1.02-1.06) 0.01 | 8.27 (2.00-34.07) 0.001 |
| Aortic aneurysm | 0.44 (0.05-3.29) 0.41 | 2.24 (1.11-4.52) 0.02 |
| Comorbidities | 3.27 (0.44-24.36) 0.21 | 4.82 (1.16-20.01) 0.017 |
| Obesity | 0.17 (0.02-1.31) 0.057 | 0.18 (0.057-0.59) 0.001 |
| Chronic kidney disease | 1.68 (0.73-3.84) 0.21 | 2.47 (1.50-4.06) < 0.0001 |
| Cerebrovascular event | 2.25 (0.89-5.67) 0.07 | 3.06 (1.73-5.42) < 0.0001 |
| Arterial hypertension | 2.34 (0.89-6.16) 0.07 | 2.90 (1.54-5.45) 0.001 |
| Arrhythmia | 1.48 (0.65-3.38) 0.34 | 2.14 (1.31-3.51) 0.002 |
| Pulmonary hypertension | 1.89 (0.88-4.01) 0.09 | 1.97 (1.22-3.18) 0.005 |
| NYHA - functional class III - IV | 1.42 (0.45-4.51) 0.54 | 3.37 (1.80-6.31) < 0.0001 |
| Betablockers | 1.24 (0.60-2.53) 0.54 | 1.75 (1.11-2.76) 0.014 |
| Lee’s revised cardiac risk index > 2 | 0.97 (0.42-2.20) 0.94 | 1.91 (1.19-3.04) 0.006 |
*(n = 843) Values presented as odds (p), OR (odds ratio) and 95% CI (95% confidence intervals).
Source: Authors.
Table 5 Crude association between postoperative variables and 7 and 30-day mortality*.
| Variable | 7-day mortality OR (95% CI) p value | 30-day mortality OR (95% CI) p value |
|---|---|---|
| ICU readmission | 1.65 (0.21-12.91) 0.62 | 3.88 (1.33-11.31) 0.007 |
| Perioperative myocardial infarction | 2.08 (0.47-9.20) 0.32 | 6.47 (2.92-14.35) < 0.0001 |
| Hypovolemic shock | 3.82 (1.49-9.75) 0.003 | 5.94 (3.22-10.97) < 0.0001 |
| Septic schock | 4.60 (1.97-10.76) < 0.0001 | 6.88 (3.90-12.13) < 0.0001 |
| Cardiogenic shock | 4.14 (1.50-11.42) 0.003 | 10.79 (5.56-20.95) < 0.0001 |
| Multiple organ dysfunction syndrome | 10.00 (3.91-25.57) < 0.0001 | 14.32 (6.67-30.74) < 0.0001 |
| Acute renal failure | 4.98 (2.12-11.69) < 0.0001 | 7.02 (3.93-12.54) < 0.0001 |
| Atrial fibrillation | 3.71 (1.35-10.17) 0.006 | 6.51 (3.39-12.50) < 0.0001 |
| Cerebrovascular event | 21.64 (4.62-101.32) < 0.0001 | 6.89 (1.51-31.34) 0.004 |
| Reintervention | 1.29 (0.38-4.38) 0.67 | 3.35 (1.81-6.21) < 0.0001 |
| Complications | 6.24 (2.94-13.28) < 0.0001 | 12.64 (7.52-21.23) < 0.0001 |
*(n = 843) Values presented as odds (p), OR (odds ratio) and 95% CI (95% confidence intervals).
Source: Authors.
Table 6 Multivariate analysis of preoperative and postoperative factors and their significant association with 7 and 30-day mortality*.
| Variable | 7-day mortality OR (95% CI) p value | 30-day mortality OR (95% CI) p value | |
|---|---|---|---|
| Preoperative variables | Functional class < 4 MET | 2.58 (1.04-6.38) 0.039 | - |
| Chronic obstructive pulmonary disease | 3.99 (1.53-10.40) 0.005 | - | |
| Chronic kidney disease | - | 2.57 (1.10-5.97) 0.028 | |
| Aortic aneurysm | - | 5.06 (1.94-13.18) 0.001 | |
| Postoperative variables | Cerebrovascular event | 14.92 (2.61-85.20) 0.002 | - |
| Multiple organ dysfunction syndrome | 3.92 (1.09-13.98) 0.03 | 3.64 (1.37-9.66) 0.009 | |
| Cardiogenic shock | - | 2.90 (1.35-6.26) 0.006 | |
| Postoperative complications | 5.09 (2.18-11.84) < 0.0001 |
* Values presented as odds (p), OR (odds ratio) and 95% CI (95% confidence intervals).
Source: Authors
It is worth noting that in 7-day mortality modeling of preoperative variables in both modes (intro and forward), chronic obstructive pulmonary disease (COPD) and functional class under 4 MET were statistically and clinically significant. A strong interaction effect was found when evaluating confusion and interaction of functional class under 4 MET as applied to the measurement of COPD impact on 7-day mortality: first, modifying more than 10% of crude ORs with stratified ORs and then finding an important effect increase (close to 2.1 times) and, alternatively, a reduction (of approximately 1.8 times) on the outcome of interest over the observation period.
Likewise, when modeling preoperative variables for 30-day mortality, statistical significance was obtained not only for the variables included in Table 6, but also for age > 60 years and ASA-PS > 2. However, those variables showed a variation of more than 10% between crude and stratified ORs in relation to chronic kidney disease and abdominal aortic aneurysm, which was why these were mainly considered as confounding variables.
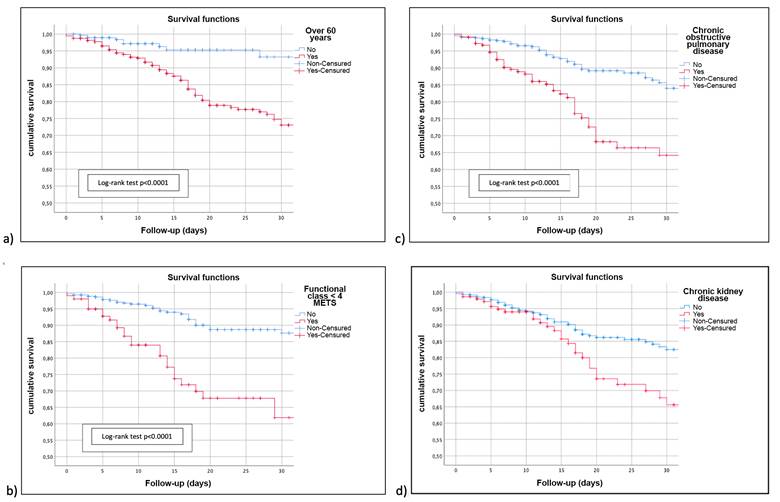
Figure 1 shows 7 and 30-day survival analysis. A Cox regression model was run for multiple factors, confirming the proportional effect of the factors included in the logistic model previously presented for 7-day cumulative mortality: COPD HR = 5.35 (95% CI 1.98-14.41; p = 0.001); functional class under 4 MET HR = 2.39 (95% CI 0.94-6.05; p = 0.065). For 30-day follow-up: chronic kidney disease HR = 2.53 (95% CI 1.59-4.01; p < 0.0001), and aortic aneurysm HR = 2.33 (95% CI 1.24-4.53; p = 0.012).
DISCUSSION
Mortality in high risk
The search for data regarding mortality in populations considered high perioperative risk is controversial because of the varying definitions and characterizations presented in the world literature. Although multiple classifications have been developed based on predicted disease-related complications and their differing degrees of exacerbation, it is only until this century that the perioperative approach has enabled a more in-depth search for risk factors. Even though analyses have been done of various risk factors and their relationship with intra and postoperative outcomes and their association with mortality (particularly from the perspective of cardiovascular risk and its early and late outcomes), few authors have approached this subject from the high-risk anesthetic perspective (perioperative).
Although overall 7-day mortality associated with non-cardiac surgery has been described between 0.5 and 1.2% 13, extreme values of up to 4% have been reported 3. This variability appears to be due to the dissimilar demographic and clinical definitions of high risk patients and, in many cases, to the fact that reporting is voluntary, and retrospective, and inclusion criteria are implemented in secondary databases and not as a result of concurrent and longitudinal follow-up of a consolidated cohort like the one validated in this project. According to Pollard et al., the incidence of overall anesthesia-related mortality is quite low, ranging between 0.509 and 2.29 deaths for every 100,000 patients 14.
In this study, cumulative 7-day (3.68%) and 30-day (10.08%) mortality, and even perioperative mortality in high cardiovascular risk patients in the first 7 days (3.60%) and 30 days (14.86%), are significantly higher than those reported in the world literature, as is to be expected given the characteristics of the subgroup of interest. In Colombia, the only study with a population of similar characteristics reported a mortality of 9.1% (95% CI; 7.411%) 11, a figure which did not include non-ICU admission or deaths occurring in the operating room. According to the world literature, the perioperative mortality rate is lower; however, there are not many studies that include only patients identified as high perioperative risk in their main objective and, in most cases, they are documented as part of secondary outcomes or as part of a subgroup analysis, which is questionable due to their significant connotation for public health 14,15.
In South America, similar mortality statistics have been reported, as is the case in Brazil, with overall mortalities ranging between 13 and 19.5 for every 10,000 anesthesias, attributed to increasing patient age, the severity of the ASA physical status classification, and the performance of urgent or emergent procedures 16. However, these studies have been conducted in the general population and not in high-risk patients. In France, by 1999, an anesthesia-related mortality survey had revealed an overall mortality of 3.16.3 deaths for every 100,000 anesthesias, in other words, one death attributed to anesthesia for every 21,200 surgical procedures. The rate is even higher in elderly patients and in patients with an ASA-PS 3 and 4 functional classification. It is worth noting that the three predominant mechanisms of death were perioperative myocardial ischemia, hypovolemia and gastric content aspiration 17.
Study of associated factors
It is clear that the study of perioperative factors associated with mortality is of critical importance given their potential impact on public health. Among factors analyzed in previous studies, a close association has been found with age extremes (under 1 year or older than 65), the ASA physical status classification, the type of procedure (according to the perioperative risk classification) and urgent procedures 18-20. In fact, this study is the continuation of a research protocol previously published and archived in the repository of La Sabana University School of Medicine, which was designed to outline the potential effect of some variables and their very certain participation in fatality; however, that work did not yield the expected statistical accuracy, given sample limitations at the time 12.
In the world, associations have been shown between mortality and patient age, a history of chronic heart failure, coronary disease, renal disease, emergency procedure, and surgical risk (preoperative conditions) 21,22. Also, associations have been shown with multiple intraoperative factors such as difficult airway, obstructive sleep apnea, opioid-induced respiratory depression, fire in the operating room, and major cardiovascular events (MACE), apart from countless postoperative complications, including delirium, ICU admission, arrhythmias, cardiac arrest, acute myocardial infarction, stroke, pneumonia, reintubation and surgical reintervention 23.
In this work, the impact of preoperative variables associated with mortality was significant: COPD, CKD, functional class and abdominal aortic aneurysm, with nominations supported by individual statisticians, impact factors and epidemiological weight explanatory models. Additionally, some preoperative disease conditions contributed to a relevant increase in mortality. The strong association between postoperative complications and a significant increase in mortality is also worth highlighting. These complications include cerebrovascular events and cardiogenic shock which are potentially preventable and/or reversible and whose perioperative impact could be mitigated by means of early and improved preventive and therapeutic approaches 24-27.
Given that mortality and complications are highly relevant clinical outcomes for public health, they are always documented in patient clinical records. Their reporting is part of the in-hospital clinical process, improving their reliability. However, the variety of surgical procedures, operator-dependent expertise and the academic nature of the institution create a sufficient degree of confusion to enable full determination of their effect.
On the other hand, the results of this study open a window into the research of both preoperative as well as postoperative factors in high-risk patients, who are usually excluded in other cohorts, and into their association with a strong clinical outcome as is mortality. It is advisable to conduct interventional clinical studies for those factors with the aim of not only determining and quantifying their impact, but also of identifying prevention and timely treatment interventions.
ETHICAL RESPONSIBILITIES
Ethics Committee endorsement
The research protocol was approved by the Graduate Research Subcommittee of La Sabana University Medical School and by the Technical and Ethics Committee of La Samaritana University Hospital Research Center (Minutes 1101-18 of December 13, 2018).
Human and animal protection
The authors declare that no human or animal experimentation was conducted for this research. The authors declare that all the procedures were carried out in accordance with the ethical standards of the responsible human experimentation committee and those of the World Medical Association and the Declaration of Helsinki.
Data confidentiality
The authors declare that they followed the protocols of their institution regarding patient data disclosure.
Right to privacy and informed consent
The authors declare that no data linked to the patients are presented in this paper.
The authors declare that, considering the ethical risk classification, the Ethics Committee of La Samaritana University Hospital Research Center did not require informed consent.
ACKNOWLEDGEMENTS
Authors' contributions
VHGC and MJR: Study planning, data collection, interpretation of the results and writing of the article.
YMM and ASS: Study planning, data collection, interpretation of the results and writing of the article.
PNSE: Study planning, data collection, and interpretation of the results.











 text in
text in