INTRODUCTION
The issue of physicians' attitudes versus the Anticipated Directives Document (ADD) has generated interest in the literature because of its ethical and legal implications. Several problems arise with regards to its fulfillment; notably, the poor implementation of the ADD 1-4 by medical practitioners, in addition to other moral issues such as the lack of respect and compliance with the advanced directives (AD). 5-8
The discussion around the unrestricted enforcement of the AD in clinical practice shall not be divorced from the ethical and moral values of the physician. The principle of respect for prospective autonomy is the bioethical foundation of AD 9 and an important factor in the positive attitudes of the physician towards the ADD. 10 Over the course of fulfilling the AD, the practitioner may express his/her personal conflicts contrary to the wishes, values and moral preferences of patients, and may even be difficult to accept the AD, hence resulting in moral anxiety that may lead to moral distress. 11
End-of-life care results in ethical dilemmas. On one hand, there is the moral obligation of the medical practitioner and the family to respect the AD, pursuant to the principle of respect for autonomy. On the other hand, there is the obligation to do what is considered best for the patient - from the clinical perspective - subject to the principle of beneficence. Moreover, it is mandatory for healthcare practitioners to avoid harm or futile therapies that perpetuate the patient's suffering. This is consistent with the ethical principles from the ethical perspective of Beauchamp and Childress; these principles are hierarchical and therefore, in actual clinical situations, the practitioner may be confronted with ethical dilemmas involving an excessive moral burden that hinders the decision-making process. Furthermore, it is essential to understand the circumstances, the moral considerations of the individuals and the communities facing these dilemmas, in order to identify alternative solutions. The ethical dilemmas regarding the respect for the ADD or for the AD, have not been studied in Colombia, neither the ethical principles and/or moral values supporting the decisions and actions by physicians. The objective of this research is to explore the ethical principles and dilemmas in the discourse of a group of healthcare practitioners who are familiar with end-of-life care based on the ADD.
METHODS
This research is a study within the framework project entitled: "Advanced Directives Document: knowledge and experience of medical practitioners in Colombia" 1, published in the Colombian Journal of Anesthesiology on November 4, 2021, "available at https://www.revcolanest.com.co/index.php/rca/article/view/1012". In summary, "this study concludes that the overall perception of healthcare practitioners about the number of ADDs signed by patients is still the same after Resolution 2665 of 2018 was adopted in Colombia; physicians have a limited knowledge about this topic and currently there are still barriers to the implementation of the ADD."
A qualitative study was designed and structured according to the hermeneutic analysis of Braun and Clark 12. The study sample included practitioners registered in the database of the Colombian Association of Palliative Care, the Association of Palliative Care of Colombia, the Colombian Association of Gerontology and Geriatrics, the Colombian League Against Cancer, the Colombian Society of Anesthesiology and Resuscitation, and the Colombian Association of Critical Medicine and Intensive Care, as of January 3ist, 2021. The text refers to them as medical practitioners involved with end-of-life care. Since the total population was not considered, the sample size was not estimated and a convenience sampling approach was used. The investigators invited each Society to participate and these in turn forwarded the invitation and survey twice via e-mail to all members, with a one-week interval. The survey was developed by the investigators with no pilot test for validation. Each participant answered the survey just once. The response rate was 4.54 %. The work setting of the practitioners included: 34% intensive care units; 15% operating rooms, and 10-13% pain and palliative care units. The mean experience of the participants was 9 years.
The practitioners who answered openly question 9 of the anonymous and voluntary survey was the inclusion criteria. The question presents an ethical conflict between the principles of beneficence and autonomy to explore the arguments of the physician to respect (or to not respect) the ADD. The exploratory question reads as follows: "Are you willing to respect an ADD in an unconscious patient when you think that the patient will benefit otherwise? Out of 533 participants, "86.6% of the practitioners say they respect an ADD, although the patient may benefit otherwise". 1 Only 253 participants answered the research question openly and voluntarily; the open statements of 253 healthcare practitioners regarding whether to respect or not the ADD, are the unit of observation of this study.
Analysis categories
The variables are submitted based on the operationalization of concepts and then an analytical disaggregation process of the main categories of the study. A hermeneutical matrix was developed with the key elements of bioethical principlism which were then contrasted against the discursive structures considered as a unit of analysis. This analysis matrix underwent an in-depth analysis by the investigators, searching for consistency in the hermeneutic approach between the concepts and the discursive indicators, in order to identify foundational and saturation processes which are typical of the analytical proposal of the foundational theory. Finally, the hermeneutical matrix developed enabled a consensus among the analysts based on the judicious implementation of the analytical induction and the constant comparative method; these processes provided a consistent interpretation of the information analyzed. The analysis used the ATLAS.ti v 9 software.
Ethical considerations
This research, under Resolution 8430 of 1993 of the Ministry of Health of Colombia, pursuant to Title II, Article 11, is classified as risk-free for humans because there is no intervention. 13 The use of the source of information was approved under document CEI 2021-02299, dated April 20, 2021 of the Research Ethics Committee (CEI) of Fundación Cardiovascular de Colombia in Bucaramanga. All the participants in the study provided their informed consent. Each of the participating medical societies implemented the confidentiality standards for data management as per their respective bylaws. The data collected were summarized and reported globally, and were used for scientific purposes only.
RESULTS
Overall characteristics of the study population
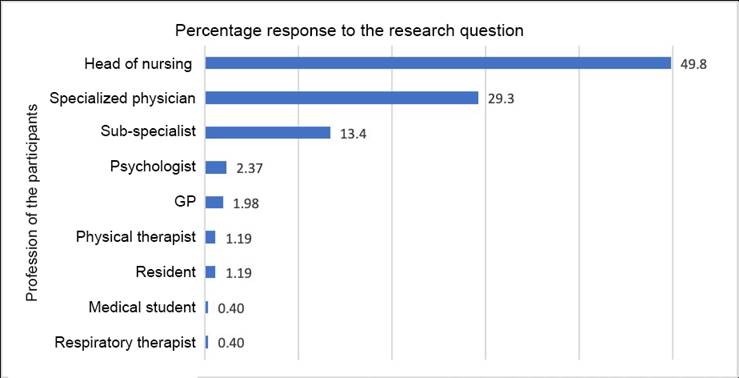
The distribution of the professionals participating in the study was as follows: Heads of nursing (47.83%), specialized physicians (29.25 %) and sub-specialists (13.44%). The miscellaneous category (9.48%) includes: psychologists, GPs, physical therapists, respiratory therapists, residents and medical students (Figure 1). The distribution of open positive or negative answers to the research question is shown in Table 1.
Table 1 Distribution of positive and negative open answers to the research question by profession.
Source: Authors.
The distribution by area of work was: 33.2 % intensive care unit; 14.62% operating rooms; and 8.7% Pain and/or Palliative Care units.
Principles, values, and rights identified in the discourse of healthcare practitioners
Most of the discourse reflects respect for freedom of decision of the human being, followed by the principle of autonomy, beneficence, non-maleficence and the value of dignity (Table 2).
Table 2 Principles, values and rights identified in the discourse of healthcare practitioners.
* Is not part of the ethical theories.
Source: Authors.
In the discourse of healthcare practitioners, the analysis of the principles, values and rights was divided into three ethical theories: Ethics of principlism, Ethics of liberal individualism and Kantian ethics. Most discourses, accounting for 50.92 % of the answers, are arguments that respect the autonomous decisions based on the theory of liberal individualism to respect the ADD (Table 3).
Table 3 Ethical theories in the discourse of healthcare practitioners.
Source: Authors.
Ethical dilemmas identified in the discourse of health practitioners
The author Sandra Realpe 14, in her article "Moral Dilemmas" makes a distinction between conflicts and dilemmas (Table 4). The conflict analysis was divided into apparent moral dilemma and genuine moral dilemma 14 (Tables 5 and 6).
Table 4 Key concepts.
| A moral conflict is any situation in which an agent is confronted with the moral obligation to do A and fulfill the moral obligation to do |
| Moral dilemma: Any situation in which an agent is unable to fulfill both obligations (A and B) because choosing one moral obligations results in overturning the possibility to fulfill the other moral obligation, or the moral agent is forced to adopt each of the moral obligations separately and hence is unable to adopt both simultaneously. |
| Genuine moral dilemma. "Moral conflict based on the impossibility of the agent to solve the conflict because both moral obligations are equally strong and in case of resolution, one agent will experience moral regret (remorse, guilt, contrition, sorrow). An agent faces a situation in which he/she is forced to take action and feel sorrow or regret for not having done something he/she should also have done." |
| Apparent moral dilemma. "The moral conflict is solved and there is no moral regret because the tension existing between moral obligations A and B were only apparent." |
Source: Adapted from Realpe 14.
Table 5 Ethical dilemmas identified in the various discourses of healthcare practitioners.
| Genuine moral dilemma | Apparent moral dilemma |
|---|---|
| Principle of beneficence vs. Principle of respect for autonomy | Reversible clinical conditions |
| Quality of life concept | Family |
| Legibility of the advanced directives | |
| Request for euthanasia in the ADD |
Source: Authors.
Table 6 Moral dilemmas in the discourse of healthcare practitioners.
| Genuine moral dilemmas | Dilemma between the principle of Beneficence and respect for autonomy | "Generally speaking, autonomy shall be respected, but this must be contextualized because if the cause is reversible the situation is different." Subject 329 |
|---|---|---|
| Differences in the physician vs. patient quality of life concept | "It is necessary to understand the idea of what is best for the patient since there may be sociocultural differences with regards to the best option for the practitioner versus the best option for the patient; for instance, a highly educated patient may consider a torture living with cognitive decline, even if it is mild to moderate." Participant 233 "I owe respect to the patient and his/her life decision, even ifI disagree." Participant 412 "...Any sequelae, consequences and outcomes of treatment and the patient's condition at discharge will be experienced by the patient, not me ..." Participant 376 | |
| Apparent moral dilemmas | Request for euthanasia in the ADD | "This request should be honored provided it does not infringe other considerations such as conscientious objection, for instance in case of euthanasia." Participant 63. |
| Patient's reversible clinical condition | "The ADD is a legal document, provided the patient's condition is irrecoverable; the will of the patient should be respected as long as the document was signed when the patient was at 100% of his/her capabilities. If the patient can be recovered but has signed an ADD, this represenst an ethical, legal and moral dilemma which is difficult to elucidate." Participant 29 | |
| Family | "If it is a legal document, I must respect it, unless the family's position is otherwise, since they may cause trouble in the future." Participant 435. | |
| Legibility of the advanced directives | "If the document is sufficiently clear and logical, I respect it." Participant 407 "If it meets the standards, I think I cannot be against it." Participant 429 "If the patient received adequate information from a proper practitioner, yes". Participant 451. |
Source: Authors.
Analysis of the results
Respect for principlism bioethics according to Beauchamp & Childress
The statements of the participants indicate a change in the biologistic and mechanistic model of medicine - defined as the artificial conservation or extension of life 15 - into a humanistic model that considers the right to a dignified death derived from respect of the autonomous agent, or the right to "quality of life" according to the values, convictions and preferences of the patient. Likewise, the practitioner acknowledges: a. the ADD and/or AD is an extension of the informed consent that should be respected and fulfilled; b. the protagonist role of the patient in the doctor - patient relationship, with absolute respect for the individual; and c. the practitioner recognizes his/her role as listener, companion and support to the patient and the family during the end-of-life process. The principle of non-maleficence is practiced by controlling pain and limiting suffering, making treatment changes and delivering palliative care. The healthcare practitioner considers both the patient's and the family's pain and distress. The value of justice is recognized in terms of respecting the decisions of others in order to have your own decisions respected, following the minimum requirement common to all theories on justice: "equals shall be treated equally." 16
Respect for the theory of liberal individualism
Represents respect for the voluntary, free and meditated decisions, aware of the impact on the life and health of the individual; in other words, practitioners respect autonomous decisions. However, "any arguments purely based on rights may change or impoverish our concept of morality; these are not comprehensive morale theories but mere expressions of the basic and mandatory rules that any community and individual shall comply for a respectful relationship with society." 16
Respect for Kantian theory
The various opinions express different meanings of the value of dignity: it may be considered as an essential and intrinsic value to the human being, defined as ontological dignity; it may refer to humanized care 17; and represent the meaning of dignified death of the individual. 1 "This ontological dignity represents an unswerving and untouchable value which does not depend on specific life circumstances, neither is it subordinated to an individual's judgement" 18. The discourses confirm the opinion of the authors Álvarez and Gomezese 1 with regards to "when the individual loses his/her decision-making ability, it makes it more difficult to fulfill the end-of-life wishes and preferences, leading to a violation of the dignified death concept."
Genuine dilemma between the Principle of Beneficence and the Principle of Respect for Autonomy
The majority of the answers given by the participants included respect for autonomous decisions (50.92%), in contrast to the principle of beneficence (10.70%). The discourses evidence the lack of conceptual clarity between the principle of respect for autonomy (autonomous agent) and respect for autonomous decisions. Probably the practitioner recognizes the principle of respect for autonomy above any other ethical principles (according to the principlism theory) or the lack of commitment to make a reflexive and deliberate analysis of the particular moral considerations in particular clinical cases.
Genuine dilemma of the physician-patient quality of life concept
The discourses acknowledge that the patient is not just a human body to be treated or cured. The patient is a human being that understands the psychological, social, cultural and spiritual dimensions 19, and medical decisions affect the future quality of life of the patient.
Apparent dilemma in a request for euthanasia
The discourse shows a potential conflict between the "rights of the patient and the rights of the physician". One of the AD that may be expressed in the ADD is when and under what clinical conditions the patient wishes to end his/her life. 20 Resolution 0971 of 2021 issued by the Ministry of Health of Colombia, under articles 3 and 14, considers the request for euthanasia via an ADD; and Article 16, acknowledges the right to objection or conscientious objection which "may only be stated by the physician required to administer the euthanasia." 21 Therefore, if the patient's AD meets the ethical criterion of accurate adjustment 9, which means that the clinical pathology must be consistent with the situation described in the ADD for euthanasia, the physician shall report to the "Committee to fulfill the right to a dignified death via euthanasia" 21. Hence, the rights of the patient, neither the rights of the physician are infringed.
Apparent dilemma in the patient's reversible condition
There is no moral conflict for the physician when the clinical condition is irreversible. It is an apparent dilemma whenever there is a contradiction between the ethical obligation (principle of beneficence) and a legal obligation (legal document).
The scope of the AD is only applicable to irreversible clinical situations: terminal condition, end-stage condition and persistent vegetative state (Table 7). 22
Table 7 Clinical scenarios to determine the scope of the Advanced Directives.
| Clinical context | Definition |
|---|---|
| Terminal condition | An irreversible condition caused by a lesion, disease or illness with no reasonable medical probability of recovery. |
| End-stage condition | An irreversible condition resulting from a lesion, disease or illness which has led to severe and progressive permanent deterioration, and for which treatment will not be effective. |
| Persistent vegetative state | A permanent and irreversible condition of loss of consciousness with absent voluntary action or cognitive behavior - or any other behavior -and inability to communicate or intentionally interact with the environment. |
Source: The authors, based on Roscoe & Schenck 22.
If the clinical condition is reversible, the AD listed in the document fails to meet the ethical criterion of accuracy of the adjustment; therefore, the physician does not have the moral obligation to comply. Above all, healthcare practitioners shall proceed in accordance with the ethical principles and moral values, over any legal obligations, which are important and deserve consideration, but there is an ethical commitment to the patient.
Apparent family dilemma
There is a potential threat of conflict and legal claims against the practitioner when the ADs of the patient are contrary to the family's wishes or interests. The family should be clearly informed that no one is entitled to change or amend the text of the ADD and that there are legal and ethical criteria for compliance thereof. If the family disagrees, it may be wise to get the assistance of a medical ethics committee, the palliative care group, psychology and social work to clarify the rights of the patient and the rights of the family. It is important for the physician to be knowledgeable about the ethical criteria for decision-making in case of incompetent individuals. 16 The right approach and the moral duty of the physician is to respect the AD expressed in the ADD, regardless of the opinions or decisions of the family. 16
Apparent dilemma in the legibility of advanced directives
The discursive elements show concern for a clear, accurate and consistent drafting according to the patient's condition. ADs may be incomplete or contradictory, may use vague terms, be irrelevant for the particular situation. Consequently, criteria shall be used to judge their ethical validity 9, including: 1. Accuracy of the adjustment 2. Plausibility and/or authenticity 3. Absence of contractions 4. Consistent system of values.
The strength of the ADs may be further emphasized with the use of the Values History as a supplement to protect and promote the autonomy of the patient. Furthermore, it may be helpful to have a proxy or a legal representative to substitute the ADD and the Values History when making decisions involving the right to autonomous choice. Therefore, in clinical situations not considered in the ADD, the proxy "has the moral obligation to follow the preferences expressed by the patient, and clarify his/her believes and values, informing the healthcare team." 16
Courses of action of the practitioners when the Advance Directive is not followed
Out of the total number of participating practitioners, only 14.62% refuse to respect the AD in the presence of reversible medical pathologies because the clinical analysis of the particular patient indicates the prevalence of the principle of beneficence over the principle of respect for autonomy. Similarly, they consult with and make shared decisions with the family, proxy or legal representative. This may be the reason for the physician to necessarily decide to take action for the benefit of the patient - which in cases such as this means acting in the best interest of the patient, in favor of the patient and consistent with Lex Artis.
DISCUSSION
This qualitative study explores the moral values and principles to understand the ethical dilemmas and the potential courses of action faced by healthcare practitioners in the decision-making process involving the ADD. From the discursive elements, it is important to highlight that 90.78% are based on ethical arguments above any legal obligations to respect the ADD (9.22%). Moore et al. reported similar results, where the physicians surveyed believe that the ethical decision is the most important outcome for patients and expressed very little concern for the potential legal consequences if they used a reasonable criteria and if the motivation for not following the plan was to try to do the best for the patient. 6 If may be inferred that practitioners follow the ethical obligations in most of the decisions and actions, although there are doubts and conflicts versus the legal obligations.
Notably, the critical analysis of the discourse elements shows a language of respect for human rights (50.92%) expressed as respect for decision-making, the right to make a choice, the right to self-determination, respect for the personality and the right to freedom of opinion. These results support the respect for the ADD as an exercise of the theory of liberal individualism, an ethical theory based on respect for rights. 16 These data are consistent with other studies such as Feely et al. 23 who believe that ADs are framed within the right of the patient to accept or reject a treatment; or, as stated by Enríquez-Canto 24, the right to have your own and other people's will respected.
Moreover, only 5.53% of the discourses recognize and ponder the respect for the value of human dignity as expressed by Kantian theory. This ethical theory argues that the respect for autonomy derives from the foundation of ontological dignity which is inescapable, constitutive and is universal to every human being. 16 Similarly, the participants in the study by Andrade et al 25 consider that "dignity is the most important principle of bioethics" neglecting the principlism theory. Likewise, Trarieux, et al. 26 report that some people claim "the right to a dignified death." In end-of-life care, the AD poses ethical challenges versus the ethical obligations such as dignity, care, justice, beneficence, non-maleficence and free expression of the personality. 10,27-29. Hence, during the deliberation and end-of-life decision-making process, other moral considerations may be considered from the valid ethical perspectives beyond principlism.
Another important finding was that only 14.39% of healthcare practitioners recognize the principle of respect for autonomy as respect for the autonomous agent; in contrast, the majority appeal to acknowledging autonomous actions and rights (50,92%). Respecting the autonomous person means to acknowledge and reaffirm his/her self-governance ability 16; in other words, the ability to choose what is good or bad for his/ her life, based on their moral values, beliefs, and personal life plans, and being accountable for their own actions or decisions. Along these lines, respecting the ADD and/or the AD is to respect the patient as an autonomous agent.
The exploratory question stated the dilemma between the principle of beneficence and the principle of respect for autonomy; 86% of the answers favored respect for human rights and respect for autonomous decisions. In this regard, it should be highlighted that ethical principles are not absolute, but are based on prima facie and have no hierarchy. 16 The principle of respect for autonomy is not an absolute moral imperative; it may be subject to other obligations such as beneficence, based on the requirement to act in the best interest of the patient. Therefore, it is up to the healthcare practitioner to specify and assess rules and standards in his/her moral judgement for decision-making in the clinical setting, according to the particular patient situation; hence, this provides moral content to the ethical principles; otherwise, it will simply be names, lists, or headings to remember.
It can be noted that only 14.62% of the healthcare practitioners surveyed decided not to respect the ADD and/or the AD in view of the ethical dilemma described in the research question because they feel that when there is a benefit from medical treatment and recovery for the patient, the criterion of the best interest for the patient according to the principle of beneficence shall prevail. Similar results were found by Moore et al. 6; some physicians preferred to follow their clinical criteria consistent with the superior interest of the patient, rather than advocating the patient's autonomy, though others felt obliged to respect the preferences of patients despite this conflict."
In the theoretical and conceptual analysis, the conflict of respect for the ADD in a reversible patient condition and favorable prognosis may be considered an apparent moral dilemma, because the clinical scenarios of AD applicability are well defined. 22 However, this study shows that the healthcare practitioners consider it a genuine moral dilemma. In this regard, Arruda et al. 5 in their systematic narrative review of 25 articles published between 1997 and 2018, found that most physicians will refrain from implementing the AD if the clinical condition of the patient is reversible with medical treatment. Burkle et al. have suggested that medical judgement is more important than complying with an existing directive, based on the clinical condition of the patient. Accordingly, fulfilment of the AD will be more frequent in chronic disease, terminal patients, or individuals suffering; in contrast, in emergency and/or reversible situations, the medical criterion shall prevail. 30
The other genuine moral dilemma - the concept of quality of life - is present when the consequences, impacts or disabilities after an intensive medical treatment ac-cording to the patient as expressed in the ADD, are contrary to the opinion of the physician. There is conflict with moral distress when the physician is required to save the patient's life at all costs (biological life), and when there is disagreement about the social value of the individual (the value of the life of an individual for the rest of the people). Quality of life refers to self-fulfillment, the ability of the individual to relate to and communicate with others. 15 Therefore, the quality of life rationale analyzes the value that life has for the person who has to live it. 16 Quality of life is a personal perception which may only be measured through the opinion of patients. 15 Consequently, it is mandatory for the ADD to enquire about the meaning of quality of life or the values history of patients.
Healthcare practitioners revealed apparent ethical dilemmas such as the request for euthanasia in the ADD, legibility of the ADD and family intervention to refuse to fulfill the AD. In previous studies such as Moore et al., these conflicts are discussed, as well others including: request for irrational or useless treatments and the use of subjective, vague or ambiguous terminology in the ADD. Question the patient's ability to understand the consequences of their preferences; the opposition of the family and time pressure in acute and urgent situations. The concerns about the validity of the AD are raised to justify the annulment of the ADD. 6 The resolution of these and other conflicts may be achieved via continuous education on medical ethics of the practitioners, a recommendation endorsed by multiple investigations, both at the national 1,31,32 and international level. 2-4,6,33,34
The specific contribution of this study to the literature on ADD is the identification of the ethical obligations governing healthcare practitioners involved with end of-life patients, to make decisions vis a vis a particular dilemma, where there is a clear ethical principle such as the respect for prospective autonomy through an ADD, or acting with beneficence in accordance with the particular clinical situation and may be contrary to the statements in the ADD. Recognizing this dilemma and the moral and legal considerations comprised in the decision-making process in this scenario is essential to understand the complexity and moral burden faced by healthcare practitioners when looking after end-of-life patients. Additionally, this analysis showed - as it was the case in other geographies -that the respect (or non-respect) of the ADD by physicians may be driven by apparent dilemmas.
In summary, healthcare practitioners tend to unequivocally solve the moral dilemma discussed in the investigation question by respecting the autonomous decisions and respect for human rights. Only 14.62 % decide to act in the best interest of the patient, based on the respect for the principle of beneficence. A genuine moral dilemma was identified between the principle of respect for autonomy and the principle of beneficence; and, when there is a contradictory view in terms of the quality of life concept of the patient as expressed in the ADD and the opinion of the physician. Most of the conflicts arising from the moral obligation with respect to the ADD and compliance with the AD are apparent moral dilemmas. The results obtained lead us to conclude that most of the participating healthcare practitioners in the study are not familiar with the clinical scenarios for applicability of the ADs 22, the instructions that may or not be recorded in the ADD 7,20 and the ethical validity criteria of the AD 9. This investigation highlights the importance and the need for bioethics education of practitioners resulting in learning of new concepts and development of skills for the ethics deliberation process in decision-making.
STRENGTHS AND LIMITATIONS
The pilot study included the participation of general practitioners, specialists and subspecialists, nursing staff and psychologists associated with the clinical services delivering care to chronic, critical or palliative care patients who could benefit from an ADD. Based on this premise we may then conclude that an interdisciplinary ethical issue was addressed, contributing to strengthening the study. Moreover, this was the first exploratory study intended to identify the moral values, the ethical principles and dilemmas regarding the respect for the ADD and/or the AD, of healthcare practitioners in Colombia.
Among its limitations, the question asked in the survey shall be considered exploratory rather than an in-depth question focusing on a particular dilemma suggested by the investigator, which does not allow for the identification of other dilemmas or issues associated with the ADD; hence the recommendation is to pursue further studies.
For future qualitative studies, the suggestion is to use an interview-based methodology with an in-depth content and approach. It would also be wise to comprise other end-of-life care areas, such as the primary care physicians and home care teams. Likewise, it is important to study the attitudes, experiences and barriers perceived by patients and families in planning for end-of-life care and the applicability of the ADD.
ETHICAL RESPONSIBILITIES
Endorsement by the ethics committee
The study was approved by the Committee of Ethics in Research (CER) of Fundación Cardiovascular de Colombia in Bucaramanga, under file CEI 2021-02299 of April 20, 2021.
Protection of persons and animals
The authors declare that no experiments in human beings or in animals were conducted for this research.
Confidentiality of the data
Each one of the participating medical societies followed the confidentiality standards for the handling of data according to their respective articles of association. The final consolidated information was anonymized. The authors declare that they have followed the protocols of their respective institutions, regarding the publication of patient data.
ACKNOWLEDGEMENTS
Contributions by the authors
AMÁA: Idea for the research and design of the study; analysis of contents and interpretation of the results, critical review and approval of the initial and final draft.
JCRM: Critical review and approval of the initial and final draft.
JLN: Analysis of contents.
OFGR: Idea of the research and study design.











 text in
text in