INTRODUCTION
Multiple pterygium syndrome, whose non-lethal variant corresponds to Escobar syndrome, is a rare, autosomal recessive disease of unknown incidence. It is characterized by multiple skeletal, genitourinary and orofacial anomalies 1. Contracture bands (pterygium) around the joints is the of cause restricted mobility in these patients which, added to the association with cleft palate, ankyloglossia, syngnathia, micrognathia, restricted mouth opening and spinal anomalies, among others2,3, constitute a challenge for the anesthesia care team, especially as concerns airway management. There are few reports in the literature and it is worth highlighting this clinical case of consecutive anesthesia interventions in the same patient with evidence of progression of the disease which required an individualized approach to the airway, adaptation of the current algorithms in accordance with the clinical stage of the patient 4,5, and use of devices such as videolaryngoscope and laryngeal mask (LMA) for intubation, not previously described in patients with this pathology.
CLINICAL CASE
This is the case of an ii-month-old female patient diagnosed with Escobar syndrome, weighing 6,200 g and measuring 50 cm, scheduled for endoscopic gastrostomy and bilateral inguinal hernia repair.
The pre-operative assessment found a nasogastric tube used since birth for feeding, barrel chest, clubfoot, arthrogryposis, spinal dysraphism and joint flexion contractures causing limited mobility.
Airway examination showed micrognathia, cleft palate, decreased mouth opening and cervical stiffness due to pterygium (Figure 1).

Source. Authors.
Figure 1 First intervention at 11 months of age. Profile view of the patient in neutral supine position showing barrel chest, cervical pterygium, micrognathia and low-set ears.
The echocardiographic study showed a 3.5 mm patent foramen ovale; renal ultrasound, hematological and coagulation studies were normal.
On the day of surgery and due to the diagnosis of an anticipated difficult airway, the assistance of an otolaryngologist (ENT) was coordinated for airway management in case an emergency infraglottic approach was needed. The operating room was prepared for the management of a difficult airway, including all the devices planned in accordance with the proposed management plans.
The patient was brought into the operating room without premedication. Non-invasive monitoring was instituted, inhalational induction was given with 100% O2 and sevofluorane titration up to 7%, maintaining spontaneous ventilation. After adequate anesthetic depth was achieved, a peripheral venous access was installed.
Atropine 20 µg/kg, lidocaine 1 mg/kg, ketamine 2 mg/kg and remifentanil infusion of 0.2 µg/kg/min were administered once adequate face mask ventilation was confirmed.
Diagnostic nasofibroscopy was performed by the ENT specialist with the patient on spontaneous ventilation; nasopharyngeal access using a 2.8 mm nasofibroscope to visualize the glottis was difficult, requiring mandibular traction maneuvers.
Diagnostic videolaryngoscopy was then performed with CMAC® using a hyperangulated pediatric D-Blade (Karl Storz, Model 8403 ZX, Germany), which was difficult to introduce, but allowed to visualize a Cormack-Lehane 2 glottis, after patient repositioning and external laryngeal mobilization. Intubation with a 3.5 mm endotracheal tube (ETT) with balloon and conductor was attempted without success in passing the vocal cords. On second attempt, intubation was achieved with a 3.0 mm ETT with balloon and conductor.
The surgery was performed without difficulty. For postoperative analgesia, a bilateral ultrasound-guided TAP block was used. Extubation was performed in the operating room uneventfully and the patient was transferred to post-anesthesia recovery.
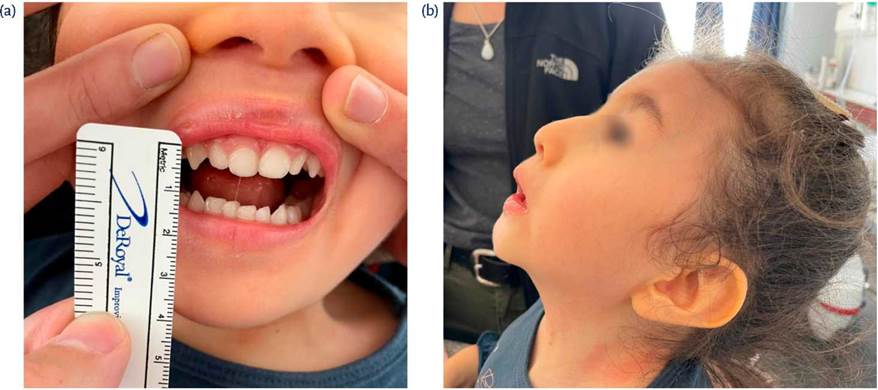
The patient was readmitted at 2 years of age for gastrostomy replacement. Weight 7,500 g and height 53 cm. The physical exam focused on the airway showed similar characteristics but found a more restricted 12 mm inter-incisor distance (mouth opening) (Figure 2).
The operating room was prepared in a similar way in anticipation of a difficult airway, with the ENT specialist in the room in case an emergency infraglottic approach was required. The patient was brought into the operating room without premedication, and non-invasive monitoring was installed. Inhalational induction was given with sevofluorane and 100% FiO2, maintaining spontaneous ventilation and confirming adequate face mask ventilation. A peripheral venous line was established and ketamine 2 mg/kg, lidocaine 1.3 mg/kg and propofol 2.5 mg/kg (fractionated) were administered.
The videolaryngoscope blade could not be introduced due to restricted mouth opening, requiring the use of fiberoptic bronchoscope-guided intubation through the LMA. The AirQ® #1.5 LMA was introduced, although with some difficulty. Adequate ventilation was confirmed. A 3.0 mm FIVE® (Karl Stoz) fiberoptic bronchoscope was introduced with a 3.5 mm ETT with no threaded balloon.
Once the glottis was visualized, the ETT was advanced through the fiberoptic bronchoscope, observing the trachea along the way. The ETT was connected to capnography for verification. The LMA mask was withdrawn with the help of a stylet after pushing the ETT. Capnography was verified and connection to mechanical ventilation was established. Anesthesia was maintained with sevoflurane and 50% FiO2. The procedure was carried out with no difficulty.
The patient was extubated in the operating room uneventfully and then transferred to the recovery room.
At 4 years of age, the patient was reassessed for a new intervention, with a finding on physical examination of a more restricted mouth opening (< 10 mm) as well as more restricted neck mobility (Figures 3a and 3b).
DISCUSSION
Escobar syndrome was described for the first time in 1902 by Bussiere and Fowley; however, in 1978, Victor Escobar provided a comprehensive description of the clinical features 6,7. Although the pathogenesis of the disease is unknown, a mutation of the CHRNG gene, involved in the formation of the gamma subunit of the acetylcholine receptor, has been found. This receptor is essential for nerve-muscle signaling, so altered nerve transmission results in fetal akinesis or hypokinesis and subsequent pterygium formation and limb contractures 2. Muscle weakness or myasthenic symptoms during development have not been described in these patients 8.
Clinical features vary, the most prominent being cervical (95% of cases), axillary, antecubital fossa, popliteal and intercrural pterygium, and syndactyly. Patients may also present growth retardation, ankyloglossia (adhesions between the tongue and palate), syngnathia (congenital bands of tissue between the maxilla and mandible), cleft palate, lumbar lordosis and scoliosis 7.
The main challenge for the anesthesiologist is airway management, as well as potentially difficult venous access, both central and peripheral, due to limb stiffness and contracture resulting in malpositioning. These patients may also have some degree of pulmonary hypoplasia and restrictive lung disease secondary to kyphoscoliosis, the severity of which increases with age 3.
Pre-anesthesia assessment should therefore be focused on the active search for factors that may hinder ventilation with face mask, supraglottic device, intubation or surgical access to the airway. In the case described in this article, micrognathia, cleft palate, reduced oral opening and cervical stiffness are prominent features. In the first intervention there was no history of surgical or anesthetic interventions.
Plans for difficult airway management were prepared and reviewed by the entire team. The Difficult Airway Society (DAS) 9 considers three sections for the management of the unexpected difficult airway: (A) Oxygenation, (B) Intubation, (C) Rescue. In this case, despite the anticipated difficult airway, we tried to follow the same logical order proposed by the DAS. During the first anesthesia intervention, spontaneous ventilation was maintained for oxygenation; once it was determined that the patient could be ventilated with a face mask, diagnostic nasofibroscopy and videolaryngoscopy with CMAC® hyperangulated pediatric D-Blade were performed before proceeding with intubation, which was achieved on the second attempt. This is the first case described using this device as the first option. The use of LMA was considered as plan B in the event adequate ventilation could not be achieved with a face mask. In case ventilation was achieved but intubation failed, a second intubation attempt was considered, optimizing the position and technique. If this was not possible, intubation through a fiberoptic bronchoscope-guided LMA was considered as plan C. In case of failure to ventilate or intubate, an emergency infraglottic approach by the ENT specialist was planned.
There are reviews in the literature of pediatric patients in whom an LMA not designed for intubation was installed following a failed intubation attempt with awake fiberoptic bronchoscopy, advancing an ETT by means of fiberoptic bronchoscopy and securing both devices as a single unit 10. This strategy has been described by other authors 3; similarly, there is a report of intubation with direct laryngoscopy 9 and airway management with LMA 2. The availability of new airway devices allowed the use of elements not described in previous studies, such as videolaryngoscopy with hyperangulated pediatric D-Blade® and AirQ® LMA for intubation; these are already included in newer pediatric airway management algorithms 4,5.
There are reports of awake intubation in adult patients using fiberoptic bronchoscopy as first choice 6,11, a technique described in anticipated difficult airway management. This is not applicable in pediatric patients due to their physiological characteristics and lack of collaboration, added to procedures that require intubation, which emphasizes the challenge for the anesthesia care team. Other studies consider LMA ventilation as a reasonable option when intubation is not necessary for surgery 2.
These patients may require multiple interventions during their lives and, unlike other congenital syndromes in which airway management becomes easier with age, in these cases difficulty is progressive due to increased joint stiffness and contractures 10. One study describes two cases of increasing airway management difficulty in subsequent interventions. In both cases, the use of the same management strategy that worked in the first intervention was used the second time, but anesthesia proved to be more difficult the second time around 10. In the case described in this article, the use of fiberoptic bronchoscope-guided LMA was anticipated for the second intervention due to the position of the chest and a more restricted mouth opening, added to the physical characteristics of the hyperangulated D-Blade®, which was impossible to insert due to its larger angle. These are all considerations in patients with Escobar syndrome because the progression of the disease may require a new management approach with each anesthesia intervention, and given that a device that worked once may not work afterwards, as was the case in our patient.
Regarding the association between this syndrome and malignant hyperthermia, there is one study on the use of halothane 12; however, in all other cases described, halogenated agents were used, with no adverse events reported 2,13,14. Also, no adverse events associated with the use of neuromuscular blockers have been reported 3,15.
CONCLUSIONS
In summary, patients with Escobar syndrome pose a challenge for the anesthesia team. Airway management must be carefully planned, clear plans must be put in place, roles must be assigned in advance, and all the team must be familiar with the sequence that will be followed. These patients may require multiple interventions and an airway which is progressively more difficult to manage will mean that different approaches must be considered for subsequent anesthesia interventions.
ETHICAL RESPONSIBILITIES
Human and animal protection
The authors declare that no experiments on humans or animals were performed for this research. The authors declare that the procedures followed were in compliance with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality
The authors declare that they have followed the protocols of their center pertaining to patient data disclosure.
Right to privacy and informed consent
The authors declare that no patient data appear in this article. The legal representative of our patient has given her written consent for publication of this article, collection of medical records and use of photographs, safeguarding the patient's privacy. This document is in the possession of the corresponding author.
ACKNOWLEDGMENTS
Authors' contribution
ALQ: literature search, article design, initial and final drafting of the manuscript, final approval of the manuscript.
NLJ: data collection, literature search, final drafting of the manuscript, final approval of the manuscript.
VMM: data collection, final drafting of the manuscript, final approval of the manuscript.











 texto en
texto en