What do we know about this problem?
Invasive ventilation support is one of the three major causes of ICU admission.
Self-extubation is an adverse outcome; around 50% of the patients need to be re-intubated.
The key documented risk factors include: male, severity of the disease leading to ICU admission, poisoning, level of awareness, use of sedatives and physical restraint.
INTRODUCTION
Since 1953, when the Danish anesthesiologist Bjorn Ibsen developed positive pressure ventilation for the treatment of the polio epidemic in Copenhagen to this day, acute respiratory failure continues to be one of the three main causes of admission to the intensive care unit (ICU). 1,2 As such, the conditions associated with intubation and mechanical ventilation, as well as the pitfalls involved, are highly relevant. Self-extubation is a growing concern, with incidence rates reported to range between 7% to 11% in medical ICUs and around 4% in surgical ICUs 3,4. Self-extubation may lead to adverse outcomes for the patient, such as aspiration pneumonia, bronchospasm, dysrhythmias, respiratory arrest, and longer hospital stays, in addition to increased healthcare costs 5. Laryngeal injuries are also frequent in self-extubated patients. 6
Furthermore, it is estimated that up to 50% of patients with self-extubation require re-intubation due to progressive respiratory distress and an inability to maintain adequate airway patency. 4) Therefore, ascertaining the risk factors for self-extubation is of paramount importance.
Some of the reported determinants include higher agitation scores 7, delirium, higher APACHE scores 8, male sex, midazolam use 9, higher Glasgow scores 10, and use of physical restraints (PR) 11,12. The use of PR showed a 3.11 fold increased risk. 3 Also, patients infected with COVID-19 seem to have greater rates of unplanned extubation requiring re-intubation as compared to those with non-Coronavirus disease. 13
Our study was intended to assess for determinants (risk factors) of self-extubation and mortality in the ICU, using a generalized estimation equation model (GEE).
METHODS
Data was collected using a retrospective cohort design including all patients above the age of 16 admitted to the ICU, between March 1st, 2017, and February 29th, 2020. An analysis of the records revealed that some records were for the same patient requiring re-intubation or admitted more than once during the study period. All patients requiring mechanical ventilation for more than 24 hours were included. Patients transferred to other institutions for continuation of treatment in ICUs, or those deceased within less than 24 hours from admission were excluded. No patients diagnosed with COVID-19 were included in this study; the first case was diagnosed in Bogotá (Colombia) on March 6, 2020; this was a young woman traveling from abroad. 14
Data were collected retrospectively from electronic health records. Independent medical researchers, not involved in patient care, collected the variables of interest. Any disagreements found while classifying the data were solved by consensus.
The following variables were collected from each subject: Age, gender, diagnosis at admission, diagnosis of chronic conditions, medications used during the hospital stay, pain (assessed through visual and numeric analog scales), whether a companion was present, report of delirium (assessed through the CAM-ICU scale) and the severity of disease (assessed through the APACHE IV score). The selection process for these variables was based on factors reported in the existing world literature; additionally, any variables considered to be relevant in terms of their association with the outcomes of interest were also included. Statistical criteria were used for the inclusion of the variables in the models (Wald Test and LR Test). Further information on the collected variables is available in Table 1. The operational definitions of the outcome variables were as follows: Self-extubation: deliberate removal of the endotracheal airway tube by the patient or as an unintended result of care by health personnel. Extubation: Final process of withdrawal of mechanical ventilation supervised by the staff in charge. Tracheostomy: Securing a surgical airway with a closed or open technique, and death.
Table 1 Characteristics of the patients included (n=857).
CNS: Central Nervous System; COPD: Chronic Obstructive Pulmonary Disease; HIV: Human immunodeficiency virus; RRT: Renal replacement therapy.
Source: Authors.
Selection biases were controlled with statistical rigor upon admission to the ICU by verifying the inclusion and exclusion criteria. Measurement biases were controlled based on the retrospective nature of the study, in addition to a homogeneous patient care process, regardless of the occurrence of any of the four outcomes described above. The statistical tool used was designed with data entry controls to avoid including errors. Finally, with the complete database, the plausibility of the included data was evaluated.
Repeated measurements of the variables were performed on the same subject in the morning, afternoon, and evening sessions during the weekdays. On weekends and holidays, day and night measurements were taken, from the time of admission to the ICU until one of the four study outcomes was reached (scheduled extubation, self-extubation, tracheostomy, or death). Finally, the data was stored in an EXCEL sheet.
STATISTICAL ANALYSIS
Univariate (mean, standard deviations for the quantitative variables, and percentages for the qualitative variables) and bivariate (Chi-square for the different variables vs the outcomes) analyzes were conducted to compare the time of occurrence of the outcomes between patients with delirium vs. non-delirium; Student's t-test was obtained. In longitudinal studies such as this one, a dependence is generated among same-subject observations. A suitable data analysis tool was introduced by Liang and Zeger (1986), based on the so-called generalized estimating equations (GEE), which is used to predict the risk of self-extubation and mortality. 15 The GEE model calculated an OR with 95%CI for each variable included, and the goodness of fit of the model was evaluated with the Hosmer-Lemeshow test. The GEE model was chosen because it allows for the analysis of repeated measurements of a subject over time for dichotomous outcomes, which is the case in the intensive care unit. About the size of the sample, all patients who met the inclusion criteria in the period established in the institution were included. Data were analyzed using STATA 14.
The study was approved by the local Ethics Committee protocol, Minutes FMCIE0136-19, at a discussion held on March 29, 2019.
RESULTS
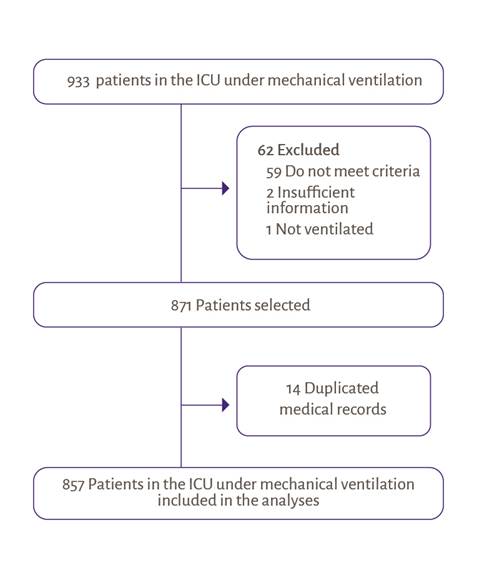
A total of 933 patients were screened; 62 were excluded, 59 failed to meet the inclusion criteria, 2 had insufficient information, and the last one was not ventilated. Additionally, 14 duplicate records were found, so finally 857 patients were analyzed (Figure 1).
Finally, 975 records corresponding to 857 patients meeting inclusion criteria were analyzed. The majority were males 538 (55.2%). The mean age was 60.5 +/- 17.8 years, and the mean body mass index (BMI) was 22 +/- 3.4 kg/m2. The mean APACHE IV score upon admission to the ICU was 59 +/- 22.1. Self-extubation was reported in 45 patients (4.7%), while 615 (63.1%) were extubated in a programmed manner and 83 (8.5%) required a tracheostomy. 224 patients (23%) died, eight patients were referred to a different facility due to insurance-related issues (Tables 1 and 2).
Table 2 Frequency of occurrence of outcomes under study.
| Outcomes | ||
|---|---|---|
| n | % | |
| Self-extubation | 45 | 4.6 |
| Programmed extubation | 615 | 63.1 |
| Death | 224 | 23.0 |
| Referrals | 8 | 0.8 |
| Tracheostomy | 83 | 8.5 |
Source: Authors.
Comorbidities are presented in Table 1. The most frequent diagnosis on admission to the ICU was pulmonary disease in 440 patients (45%), followed by central nervous system pathology in 186 (19%), hematological conditions in 65 (6%), and finally 45 patients (4%) in major trauma (Table 1). During sedation, 98 patients (10%) were exposed to benzodiazepines. Deep neuromuscular blockade with rocuronium or cisatracurium infused over a period of 48 hours (Dose range 9-12 mcg/ kg/min and 2-3.5 mcg/kg/min respectively) was used in 54 patients (5%). Of these, 16 (29%) were treated with rocuronium, and 38 (70%) were treated with cisatracurium.
A comparison of the time to outcome among patients, with and without delirium (assessed using the CAM-ICU scale), showed that tracheostomy was a significant differentiator for patients with delirium. Programmed or self-extubation and dead did not show any differences (Table 3).
Table 3 Bivariate analysis. Comparison of time to outcome among with and without delirium (assessed through the CAM-ICU scale).
| Outcome | Time to outcome (mean +/- DSD) | ||||
|---|---|---|---|---|---|
| n = 975 | Total | Delirium (n) | No delirium (n) | p-value | |
| Tracheostomy | 83 | 8.4 +/- 4.86 | 4.37 +/- 1.92 | 8.76 +/- 4.9 | 0.02 |
| Death | 224 | 5.55 +/- 4.89 | 4.83 +/- 3.51 | 5.67 +/- 5.28 | 0.52 |
| Programmed extubation | 615 | 4.14 +/- 2.81 | 4.42 +/- 2.55 | 3.83 +/- 2.51 | 0.14 |
| Self-extubation | 45 | 2.98 +/- 2.94 | 2 +/- 1.73 | 3.54 +/- 4.18 | 0.316 |
Source: Authors.
GEE MODEL FOR THE PREDICTION OF SELF-EXTUBATION
An 8.99-fold risk (95%CI 3.83-21.1, p<0.01) was identified in patients with a Richmond Sedation Scale (RASS) score greater than 2 points versus a score of 0 or -3. Delirium was assessed using the CAM-ICU scale, with a 4.55-fold increased risk (95%CI 1.7911.24, p<0.01) in patients who developed delirium. The estimates of the GEE model are presented in Table 4. The use of physical restraints was not found to have an association with self-extubation OR 1.38 (95%CI 0.76-2.51, p=0.294).
Table 4 Estimates of the GEE model for the prediction of self-extubation.
| Self-extubation | n = 45 | OR | p-value | CI 95% |
|---|---|---|---|---|
| Neuromuscular blockade | 6 | 3.37 | 0.01 | 1.31 - 8.68 |
| RASS score (agitation vs score < -3) | 32 | 8.99 | 0.00 | 3.83 - 21.1 |
| CAM-ICU (delirium vs no delirium) | 17 | 4.55 | 0.00 | 1.79 - 11.24 |
| Sex (male vs female) | 32 vs 17 | 2.02 | 0.03 | 1.06 - 3.98 |
| Physical restraints | 28 | 1.38 | 0.294 | 0.76 - 2.51 |
Goodness of fit Hosmer-Lemeshow p-value = 0.35
Source: Authors.
GEE MODEL FOR PREDICTING MORTALITY
APACHE IV score, age, and cancer were associated with an increased risk of death (Table 5). Additionally, a RASS score of 0 (alert) is protective against a score of less than 3 (moderate sedation) (OR = 0.57; IC 95% 0.38 - 0.83, p<0.001).
Table 5 Estimates of the GEE model for predicting of mortality.
| Mortality | n = 224 | OR | p-value | CI 95% |
|---|---|---|---|---|
| Age >60 years old | 156 | 1.02 | 0.016 | 1.002 - 1.027 |
| RASS (0 to -2) vs (-3) | (183) vs (123) | 0.57 | 0.004 | 0.38 - 0.83 |
| Benzodiazepines | 32 | 0.44 | 0.004 | 0.25 - 0.78 |
| Cancer | 59 | 1.72 | 0.014 | 1.12 - 2.64 |
| APACHE IV score >60 | 159 | 1.02 | 0 | 1.01 - 1.03 |
| Physical restraints | 136 | 0.65 | 0.009 | 0.47 - 0.9 |
Goodness of fit Hosmer-Lemeshow P-value = 0.09
Source: Authors.
DISCUSSION
An increased risk of self-extubation was identified in patients with agitation. This is similar to the findings from previous studies reporting higher agitation scores in association with self-extubation cases 7. Patients with moderate to severe Acute Respiratory Distress Syndrome (ARDS), defined as a ratio of the partial arterial oxygen pressure to fraction of inspired oxygen of < 150 mmHg (PaO2/ FiO2) may benefit from an infusion of neuromuscular blockade. 16 Our study found higher rates of self-extubation in subjects exposed to infusion of neuromuscular blockade. The latter differs from previous reports stating that the use of neuromuscular blockade may facilitate mechanical ventilation by improving patient-ventilation synchrony, instead of being associated with self-extubation. We believe this discrepancy may be explained by the lack of standardized measures for assessing our patients' adequate degree of neuromuscular blockade. Regarding mortality, as expected, APACHE IV score, age, and cancer were associated with an increased risk of death, while being alert as opposed to sedated, was found to reduce the risk of mortality. This may be explained by the fact that alert patients are usually in a better clinical state than those requiring sedation.
Physical restraint (PR) is used in critical care around the world in many ways with varying rates between 0 to 100%; the highest rates are reported in the USA and Canada, ranging from 87% to 76%, surgical and general ICU respectively. France is in the middle with 50%, while lower rates are reported by Norway ICU (14.4%) and Germany general ICU (11%), and Australia is the lowest (7%). 17 No association was identified in our study between the use of physical restraints (PR) and self-extubation, in contrast to what is reported in the world literature that the use of PR increased by 3.11 times the risk of self-extubation 3. Additionally, PR generates a negative physical impact on patients like pressure ulcers, edema, and bruising. In terms of mental health, fear, depression, and loneliness are very common. 18,19 Moreover, the use of PR results in a negative emotional impact for nurses with feelings of guilt and sadness, similar to the feelings experienced by healthcare workers during the COVID-19 pandemic 19.
Therapeutic alternatives to PR should be considered in the ICU. While our study found a decreased risk of mortality in restrained patients, it is important to note that these results should not be interpreted as if the use of PR alone decreases mortality. 20 This fact highlights the importance of individualizing patient care, since the cause for requiring mechanical ventilation may also impact the frequency of self-extubation and the role of PR.
Furthermore, it is important to note that pain assessment through self-report becomes impossible in patients undergoing neuromuscular relaxation. As such, we consider that different tools for assessing the degree of muscular blockade, such as the Train of Four (TOF) originally used in anesthesia, may be useful in ICU settings. 21 Moreover, the use of the Critical Care Pain Observation Tool (CPOT) and the Behavioral Pain Scale (BPS) could result in improved accuracy to detect pain, as compared to scales used in an isolated fashion 22.
Regarding patients with and without delirium and the time to reach the four outcomes of interest (tracheostomy, extubation, self-extubation, and mortality), an association was only found between delirium and the shorter time of performing tracheostomy. It is probably due to the difficulty of performing the extubation prediction tests added to the evaluation of swallowing in this population, which would lead the medical team to request early tracheostomy.
There are a few limitations in this study. The results presented correspond to a single center, which may not be representative of patients with several critical conditions. Additionally, physical restriction and exposure to benzodiazepines are associated with protection against mortality in the analysis (GEE model), but should be interpreted with caution. Moreover, the retrospective data collection may result in information biases. However, to the best of our knowledge, this is the first study to report neuromuscular relaxation as a risk factor for self-extubation in Colombia. Furthermore, this retrospective cohort includes patients before the COVID-19 pandemic.
Adequate sedation, pain control, and timely follow-up, particularly in patients requiring neuromuscular relaxation are paramount. The control of risk factors for the development of delirium should always be considered. Our study includes patients undergoing mechanical ventilation due to different causes, without COVID-19. Nonetheless, future studies should assess whether the determinants of self-extubation change in a subgroup analysis including only patients with ARDS due to COVID-19.
The primary self-extubation-associated factors include: agitation, delirium, and exposure to infusion of neuromuscular blockade. Adequate management of sedation, pain control, and real-time followup is of great importance, particularly in patients requiring neuromuscular relaxation. The use of physical restraints was not associated with the outcome of interest.
ETHICAL DISCLOSURES
Ethics committee approval
The study was approved by the local Ethics Committee protocol, Minutes n. FMCIE0136-19, at a discussion held on March 29, 2019.
Protection of human and animal subjects
The authors declare that no experiments were conducted on humans or animals for this study. The authors declare that the procedures followed were in accordance with the relevant clinical regulations of the research ethics committee and of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Right to privacy and informed consent
The retrospective cohort study shall adhere to the standards of good clinical practice; patients shall not be subject to additional studies, nor will additional tests or medication be indicated. The data will be kept completely confidential. This study does not represent any risk to the participants, hence no informed consent shall be required.











 texto em
texto em