INTRODUCTION
Hypertension (HT) is a global problem that affects patients undergoing surgery, predominantly the elderly, African Americans, and males. 1,2 In the surgical setting, 1 in 4 patients has HT 3 and despite its high prevalence, there are no current guidelines for a perioperative approach and course of action.
Several prospective and retrospective studies have been published to elucidate the relationship between HT and cardiovascular risk in the perioperative setting, with conflicting results. For example, Goldman et al. did not find statistically significant differences in perioperative cardiac risk when comparing hypertensive versus non-hypertensive patients. 2,3 Likewise, Howell et al. found no association between systolic and diastolic blood pressure (stage 1 and 2 according to JNC 8), surgery admission, and death from cardiovascular ethiologies when comparing controlled versus uncontrolled hypertensive patients. 4 In contrast, Prys-Roberts et al. showed an association between uncontrolled hypertension and intra-operative myocardial ischemia and arrhythmias. 5
Additionally, Sanders et al. assessed 414,895 patients undergoing primary arthroplasty (164,380 with HT). They found that perioperative HT was a risk factor for a prolonged hospital stay, readmission, and mortality. While in 14,524 patients undergoing an abdominal aneurysm repair (7,970 hypertensives), HT impacted hospital stay and readmission but not mortality. 6 Likewise, the 2014 ACC/AHA guidelines state that hypertensive patients undergoing surgery have a higher risk of operative death and surgical morbidity, including arrhythmias, myocardial ischemia, AMI, stroke, and impaired kidney function. 7
As a result of inconsistencies in literature, the association between HT and poor surgical outcomes is unclear and cut-off values to delay surgery have not been established. 4,8 This review of the current literature and its applicability is intended to offer some guidance for the perioperative management of HT.
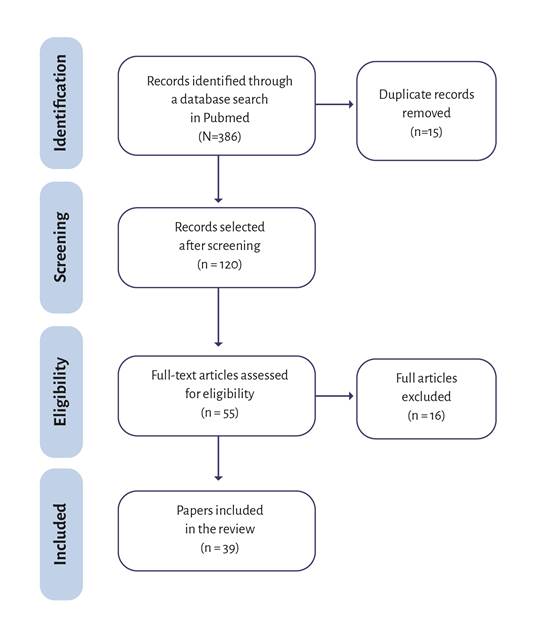
Three hundred and eighty-six articles were found in Pubmed using the keywords: "hypertension" and "perioperative period". 120 papers were eligible by screening the title and abstract. 55 papers were selected for full-text eligibility and 16 were excluded, for a total of 39 articles (Figure 1).
DEFINITION OF TERMS
According to the 2017 ACC/AHA/AAPA/ABC Guideline for the Prevention, detection, and management of hypertension in adults, a list of recommendations and management algorithms were included (See Tables 1, 2, 3). 9
Table 1 Definition of hypertension during medical consultation or outside the office and treatment goal.
| Medición | SBP | DBP | ||
|---|---|---|---|---|
| Blood pressure during medical consultation | >=140 | and/or | >=90 | |
| Ambulatory blood pressure | ||||
| Day | >=135 | and/or | >=85 | |
| Night | >=120 | and/or | >=70 | |
| 24 hours | >=130 | and/or | >=80 | |
| Blood pressure at home | >=135 | and/or | >=85 | |
| Goals of treatment | ||||
| General population | With diabetes | With chronic kidney disease | ||
| Age (Years) | >60 | 18-59 | >=18 | >=18 |
| Blood pressure goals (mmHg) | <150/90 | <140/90 | <140/90 | <140/90 |
Source: Adapted from 25.
Authorization: AMERICAN MEDICAL ASOCCIATION LICENSE NO. 3726800471301. OCT 12, 2015. Licensed content publication JAMA. https://s100.copyright.com/CustomerAdmin/PLF.jsp?ref=9d74c3dd-231a-45cd-bbd2-74abdfdcf0f
Table 2 Antihypertensive drugs.
| General population | With diabetes | With chronic kidney disease | ||||
|---|---|---|---|---|---|---|
| Race | Non African American | African American | Non African American | African American | Non African American | African American |
| Initial drug | ACEI, ARB II, CCB or diuretics. | BB or diuretics | ACEI, ARB II, BB or diuretic | BB or diuretics | ACEI or ARB II | ACEI or ARB II |
| Lifestyle modifications should be introduced during treatment, including a low sodium diet, physical activity, and weight loss. | ||||||
ACEI = Angiotensin-converting enzyme inhibitor, ARB II = Angiotensin receptor blocker, BB = Beta-blockers, CCB = Calcium channel blockers.
Source: Authors.
Table 3 Which antihypertensive to start with?
++ Start antihypertensive therapy, preferably once a day.
ACEI = Angiotensin-converting enzyme inhibitor, ARB II = Angiotensin receptor blocker, BB = beta-blockers, CCB = calcium channel blockers.
Source: 26.
Authorization: BMJ PUBLISHING GROUP LTD. LICENSE NO. 3847880222323. Apr 14, 2016. Licensed Content Publisher BMJ Publishing Group Ltd.
Arterial hypertension
Defined as systolic blood pressure (SPB) 130 mmHg and/or diastolic blood pressure (DBP) ≥ 80 mmHg 9.
Stage I refers to a SBP between 130139 or a DBP of 80-89, including values in an ambulatory blood pressure monitoring (ABPM) setting. Stage II is defined as a SBP ≥140 or a DBP ≥ 90 9.
Hypertensive crisis (HTC)
Defined as a SBP > 180 mmHg or DBP > 120 mmHg, with or without target organ damage (TOD), clusters the terms hypertensive urgency and emergency 9.
Hypertensive emergency
A SBP > 180 mmHg or DBP > 120 mmHg with evidence of TOD. Under acute conditions, SBP/DPB > 220/140 mmHg will result in severe deterioration and organ damage if not managed promptly. 10
EPIDEMIOLOGY
According to the World Health Organization (WHO), the prevalence of HT increases with age, and it is estimated that 1/3 of the world's population has this condition. Despite medication, 1/3 of these people do not achieve target blood pressure levels. 11 HT increases the risk of coronary, renal, peripheral, vascular, and cerebrovascular illness, accounting for more than 15% of all cardiovascular deaths worldwide (9.4 million). 11,12 Perioperative HT can vary depending on a patient's characteristics and type of surgery. For instance, Sanders et al. found an HT incidence of 15% in cardiac and carotid surgery, 55% in abdominal aortic surgery, 40% in primary joint arthroplasty, and 29% in peripheral vascular surgery. 6
PATHOPHYSIOLOGY
The pathogenesis of HT is multifactorial, interrelated, can be overlapping, and is not fully understood. Genetic polymorphisms contribute to 30-50% of blood pressure changes. 13 Disturbances in humoral, (adrenomedullin, dopamine, renin, angiotensin II) 14,15, inflammatory (metalloproteinases, tumoral necrosis factor (TNF), "C-reactive protein," nuclear Kappa factor) 15, and renal mediators (three mechanisms: 1. Decreased glomerular filtration rate, limiting sodium excretion, 2-increased sodium reabsorption in the distal nephron, 3. Renal ischemia due to oxidative stress and/or pro-inflammatory states) contribute to the development of the disease. 16
HT results from increased systemic vascular resistance (SVR). Due to arteriole contraction, SVR increases, and becomes permanent when associated with endothelial damage secondary to a biomolecular imbalance between vasodilators such as nitric oxide and endothelium-derived vasoconstrictors. 17 This situation leads to microcirculatory dysfunction, arteriole remodeling, and decreased vascular compliance, eventually leading to complications if left untreated such as retinopathy, vascular dementia, nephropathy, cardiac hypertrophy, and ventricular dysfunction. 18
Blumenfield et al. recommend a stratification of chronic HT based on the underlying mechanism: 1- Increase in plasma renin (≥0.65 ng/ml/h), and 2. volume-dependent HT, called type V HT. The first group shows better therapeutic effects with angiotensin-converting-enzyme inhibitors (ACEIs and Beta-blockers, R drugs), and the second group shows better therapeutic effects with diuretics, aldosterone antagonists, calcium channel blockers (CCBs) and alpha-adrenergic blockers (type V drugs). 19
Systolic, diastolic, mean, or pulse pressure
Blood pressure (BP) comprises the pressure fluctuation during the cardiac cycle; SBP and DBP reflect extreme values of continuous variations in differential pressure. Diastolic pressure reflects the trend of arterial resistance and mean arterial pressure (MAP), which is crucial in diagnosing and managing HT. The SBP is related to BP pulse variations (given by the difference between systolic and diastolic) and is influenced by the left ventricular ejection fraction and by the pulse wave reflection. 20
The walls of the aorta and the large elastic arteries stiffen with age due to senile degenerative phenomena, resulting in a poorly distended wall during systole and, therefore, an increase in SBP and pulse pressure (PP). These physiological changes make it challenging to determine whether SBP, DBP, MAP, or PP has greater clinical significance in developing HT associated with cardiovascular complications. Gasowski et al. analyzed seven randomized clinical trials involving hypertensive and stroke patients and found an independent association between hypertension and having a 10 mmHg PP variation with an increased risk (6-7%) of dying from cardiovascular complications. 21 Likewise, PP elevations are more significant in fatal coronary events than changes in MAP. The increase in PP was not associated with an increase in stroke events, but as age increased, a relationship was seen. 21
SBP increases with age, while DBP peaks around the fifth decade of life, decreasing thereafter. This phenomenon makes DBP one of the best predictors of cardiovascular risk in young adults (<50 years). On the other hand, PP, SBP, and DBP are good predictors for patients aged 50-59, but PP is the best predictor in patients over 60 years old. 22
HT IN PRE-ANESTHESIA CONSULTATION
Diagnostic criteria for HT should be assessed in a patient with high blood pressure: assess TOD (retinopathy, left ventricular hypertrophy, albuminuria); assess cardiovascular risk due to comorbidities; rule out secondary causes and define the relevance of anesthesia. 23
Patient without a previous diagnosis of HT
BP should be measured under the best possible conditions: patient sitting 2-3 minutes before the reading, measurement in both arms, record results in supine decubitus, and standing to detect orthostasis. In patients with a blood pressure ≥140 / 90 mmHg, 8th/9th, a second measurement should be performed and the lower value used to determine further action. A diagnosis of HT should be made after two or three measurements taken at least two weeks apart. 9,24
In patients without a history of HT and with blood pressure values above the threshold (JNC 8th/9th), it is recommended to request laboratory tests to rule out TOD: urinalysis, electrolytes, serum creatinine, fasting blood glucose, complete lipid panel, and echocardiogram to rule out left ventricular hypertrophy; if this is the case, the patient should be referred for evaluation by internal medicine. Pharmacologic treatment may be started simultaneously (Table 3), while continuing to prepare the patient for surgery. 9,24
Out-of-office blood pressure measurement (Table 1)
Home Blood Pressure Monitoring (HBPM) is the BP self-measurement, known as "fine-tuning blood pressure", measured by the patient at home or with visits to a health center twice a week, in the morning, before having breakfast or taking medication. Usually, these values are lower than those registered in the doctor's office. 23
Ambulatory blood pressure monitoring (ABPM): Automatic devices for continuous measurement of BP during 24-48 hours in the patient's environment. The indications for ABPM are: suspected white coat HT or masked HT; variability in BP measurements; drug-induced HT; postprandial, autonomic, or postural hypotension; when there is a need to identify real and false resistant HT; suspected nocturnal HT and in patients with sleep apnea, chronic kidney disease, or diabetes. 23,24
Initial approach of preoperative hypertension.
This is applicable to patients with recently diagnosed HT, considering: blood pressure values before treatment, age, race, and comorbidities. Pharmacologic treatment should be guided by patient characteristics (Tables 2, 3 and 4).
Table 4 Antihypertensive drug dose.
| Antihypertensive medication | Initial dose (mg) | Dose range according to response (mg) | Number of doses per day |
|---|---|---|---|
| Thiazide diuretics | |||
| Hydrochlorothiazide | 12.5-25 | 25-100 | 1-2 |
| Indapamide | 1.25 | 1.25-2.5 | 1 |
| Angiotensin Receptor Antagonist | |||
| Candesartan | 4 | 12-32 | 1 |
| Losartan | 50 | 100 | 1-2 |
| Valsartan | 40-80 | 160-320 | 1 |
| Irbesartan | 75 | 300 | 1 |
| Angiotensin-Converting Enzyme Inhibitors | |||
| Captopril | 50 | 150-200 | 2 |
| Enalapril | J_5 | 20 | 1-2 |
| Lisinopril | 10 | 40 | 1 |
| Calcium Channel Blockers | |||
| Amlodipine | J_2.5 | 10 | 1 |
| Extended-release diltiazem | 120-180 | 360 | 1 |
| Nitrendipino | 10 | 20 | 1-2 |
| Beta-Blockers | |||
| Atenolol | J_25-50 | 100 | 1 |
| Metoprolol | 50 | 100-200 | 1-2 |
Source: 25.
Authorization: AMERICAN MEDICAL ASOCCIATION LICENSE NO. 3726800471301. OCT 12, 2015. Licensed content publication JAMA. https://s100.copyright.com/CustomerAdmin/PLF.jsp?ref=9d74c3dd-231a-45cd-bbd2-74abdfdcf0f3.
People under 40 years of age with no evidence of target organ damage, cardiovascular disease, chronic kidney disease (CKD), or diabetes mellitus (DM), should suspect secondary HT and reassess surgical urgency, until the patient is examined by an internal medicine specialist. Secondary HT should be suspected in the presence of fast clinical worsening (functional class deterioration, evidence of TOD), accelerated HT (> 180/110 with signs of papilledema and/ or retinal hemorrhage), or poor response to treatment. The most common cause is CKD; other causes are renovascular HT, pheochromocytoma, Cushing's syndrome, and primary hyperaldosteronism. All patients with suspected secondary de novo HT should adjourn surgery and be referred to a specialist for appropriate perioperative management and diagnosis. 27
Patients with severe HT and signs of papilledema, retinal hemorrhage, or suspected pheochromocytoma should immediately be referred to the emergency department. Regardless of anesthesiologist decision to initiate pharmacotherapy, all patients with a recent diagnosis or suspected HT require an internal medicine assessment and further evaluation if TOD is present. Data shows that patients with Whitecoat HT (Normal Ambulatory BP, in clinical HT), do not have an increased cardiovascular risk and exposure to aensthesia is not contraindicated. 27
Indication for management of perioperative arterial hypertension
A perioperative blood pressure target of SBP <180 mmHg and DBP <110 mmHg has been suggested as a cut-off value to take a patient to elective surgery. However, recent evidence suggests that the cut-off value for SBP could be 200 mmHg, with the caveat that a TOD represents a higher risk and should be actively identified (ischemic heart disease, heart failure, kidney failure, and stroke). 3,27
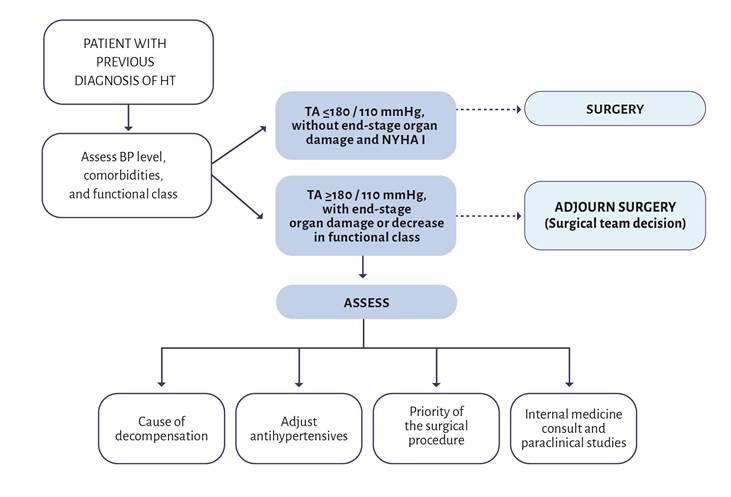
Based on this definition, the patient may be classified into the following categories (Figures 2 and 3):
First scenario: patient with controlled HT that presents SBP <180 (200) mmHg and a DBP <110 mmHg on the day of surgery. There are no contraindications for surgical intervention. These blood pressure values do not represent a risk factor for perioperative cardiovascular complications in non-cardiac surgery therefore, postponing the procedure is unnecessary. 27
Second scenario: patient with SBP ≥ 180 mmHg and/or DBP ≥ 110 mmHg. Search for common causes such as missing a dose of the antihypertensive medication. In this case, consider acute control of HT, and administer the medication or a comparable intravenous antihypertensive. A small dose of midazolam can also be administered. Differ surgery while waiting for the drugs to have an effect. 27.
Third scenario: patient with HT that presents on the day of surgery with SBP ≥ 180 mmHg and/or DBP ≥ 110 mmHg, the cause is not skiping a dose of medication and does not improve with midazolam. The available evidence is inconclusive: consider the benefit of surgery versus the risk of cardiovascular complications. 27 To proceed with surgery despite these blood pressure levels requires extreme caution; according to the 2017 American College of Cardiology, these values are in the category of hypertensive crisis. If the SBP is 200 mmHg or above, it is advisable to adjourn the surgery if possible. A large retrospective study showed that preoperative patients with a SBP above 200 mmHg had more than twice the risk of elevated troponin or death. 27
Medications before surgery
- Alpha-2 agonists: Its routine use is not recommended in non-cardiac surgical patients (Class III recommendation, level of evidence B). 28 The POISE 2 study showed that the de novo use of low-dose clonidine failed to decrease the death rate or the number of non-fatal acute myocardial infarction (AMI) in adults undergoing noncardiac surgery. However, there was an increased incidence of bradycardia, cardiac arrest, and hypotension. 29 Some studies in cardiac and vascular surgery did show that clonidine was associated with lower mortality and less myocardial infraction. 30 Therefore, the use of alpha-2-agonists in cardiac surgery is still debated.
- Beta-blockers (BB): Starting a perioperative BB is helpful in patients with an intermediate or high risk of myocardial ischemia in stratification tests (IIb, C). It is preferable to start the medication 2 to 7 days before surgery. 7 However, according to the guidelines of the European Society of Cardiology, a beta-blocker treatment is recommended at least 1 week before surgery (Level of evidence C). Initiating treatment shortly before surgery (< 24 hours) may increase the risk of side effects because of the aggressive nature of the treatment and tolerability is not assured. 31
- Calcium channel blockers (CCB): In non-cardiac surgery, CCBs have been associated with a decrease in myocardial ischemia, supraventricular tachycardia, and death, particularly with diltiazem. Dihydropyridines and verapamil did not decrease the incidence of myocardial ischemia. However, verapamil decreased the incidence of supraventricular tachycardia. 7
- ACE inhibitors and ARB II: Data is limited to observational studies, and there are contradictory positions regarding their perioperative use. The European guidelines recommended suspending medication on the day of surgery and restarting it postoperatively after fluid replacement has been assured. 32 However, the 2014 ACC/AHA guidelines suggest that the continuation of these medications is reasonable (IIa, B). A meta-analysis revealed that patients taking ACE inhibitors or ARB II had no change in cardiovascular outcomes or mortality, but there was an increased risk of hypotension. 33 Moreover, the continuous use of these drugs in patients with heart failure and hypertension is strongly supported. 34 If the medications are discontinued before surgery, patients should restart as soon as possible after the procedure (IIa, C). 7
- Diuretics: The recommendation is to avoid diuretics on the day of surgery due to the potential interaction with fluid depletion during the procedure. However, in heart failure patients, diuretics whould be administered up to the day of surgery, resumed intravenously perioperatively, and continued orally after the procedure (I, C). 32
The use of antihypertensive drugs should be individualized according to the circumstances of each case. The guidelines in this review were established based on the recommendations from the available evidence.
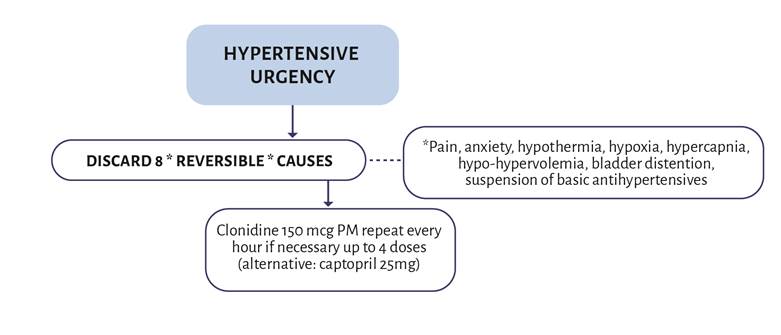
TREATMENT AND CONTROL
The first step is to rule out any reversible causes before starting antihypertensive treatment: pain, anxiety, hypothermia, hypoxia, hypercapnia, hypo-hypervolemia, bladder distention, suspension of antihypertensives (restart antihypertensives depending on the clinical scenario). Other less common causes are AMI, intracranial hypertension, pulmonary thromboembolism, anticholinergics, sympathomimetic agents, and monoamine oxidase inhibitors (MAOIs). 27
PERIOPERATIVE PHARMACOLOGICAL TREATMENT
Sodium nitroprusside
Onset of action: seconds, biological half-life: 1 - 2 minutes.
Infusión rate: start with 0.25 to 0.5 mcg/ kg/min. Treatment should be as short as possible and the infusion rate should not exceed 2 mcg/kg/min.
Adverse effect: cyanate poisoning with doses > 5 mcg/kg/min, extended dosing, kidney and liver failure. 3
Venous and arterial vasodilators reduce the preload and the afterload. Their primary advantage is their rapid onset of action, short duration, and little impact on heart rate (HR). The powerful and labile antihypertensive effect requires careful monitoring, preferably with the use of an arterial catheter. 35.
Despite their pharmacokinetic benefits, there are also some disadvantages: tachycardia, nausea, vomiting, abrupt BP drop, decreased renal blood flow, myocardial ischemia, thiocyanate toxicity, imbalance in pulmonary ventilation/ perfusion, worsening of hypoxemia (caution in patients with Chronic Obstructive Pulmonary Disease, Acute Respiratory Distress Syndrome, and severe pneumonia). Myocardial ischemia may occur secondary to an excessive reduction in blood pressure and loss of coronary perfusion pressure, reflex tachycardia that increases myocardial oxygen demand, or a redistribution of coronary blood flow (coronary steal syndrome). 36 It can also cause an abrupt increase in intracranial pressure (ICP) with decreased cerebral blood flow, which becomes a disadvantage in post-craniotomy procedures. 35 For these reasons, the recommendation is to use vasodilators only as a second or third treatment option when other intravenous antihypertensive agents are unavailable, in patients with normal kidney and adequate liver function. 3,32
Signs of cyanide poisoning include central nervous system (CNS) impairment with headache, anxiety, confusion, lethargy, and coma. Other manifestations like cardiovascular instability with atrioventricular (AV) block, cardiac ischemia, arrhythmias, and changes in oxygenation and pH, can also occur. Poisoning could be prevented with the co-administration of sodium thiosulfate (unavailable in several hospitals around the country). 36
Nitroglycerine
Onset of action: 2 - 5 minutes. Start with 5 mcg/min increasing by 5 mcg/min every 5 to 10 minutes, up to a maximum of 200 mcg/min.
A venous vasodilator increases the capacitance and decreases the preload with subsequent reflex tachycardia. Low doses (<60 mg/min) can be used as a co-adjuvant or as a single therapy if there is an adequate response in blood pressure reduction. Nitroglycerine acts as a coronary vasodilator, and is indicated as a first-line therapy in hypertensive angina or concomitant myocardial ischemia. It is also an option in patients with compromised oxygenation since it can be better tolerated than nitroprusside due to hypoxic pulmonary vasoconstriction and less pulmonary shunts. 3 However, prophylactic nitroglycerine is not effective in reducing myocardial ischemia and is not recommended in patients undergoing noncardiac surgery. 7
Tachyphylaxis is the major adverse effect and develops 48-72 hours of infusion; it is a compensatory mechanisms (mediated by baroreceptors and hormones) in response to blood pressure drop and the decrease in the sulfhydryl donors necessary for the metabolism of nitrates to nitric oxide. It should be used with caution in patients with left ventricular dysfunction since it can lead to a marked decrease in Cardiac Output (CO), depending on blood volume levels. In critical aortic stenosis, the output depends on the preload; if possible, avoid its use. It may also cause headaches, vomiting, and methemoglobinemia. 37
Beta-blockers
BBs are used to control both HR and BP (esmolol, bisoprolol) or BP alone (metoprolol and labetalol) in the perioperative period. It is recommended to start treatment either with metoprolol (daily dose of 50 mg) or bisoprolol (daily dose of 2.5 mg). Adjust the dose to achieve a resting heart rate of between 60 and 70 heartbeats per minute and a systolic blood pressure of > 100 mmHg. 32
Labetalol
The onset of action starts after 2 to 5 minutes and has a half-life of 2 to 4 hours.
Starting dose: 5 - 20 mg, and then double the dose every 10 minutes. Build up until achieveing the target BP or up to 40 mg. The infusion rate should be between 1 - 2 mg / min titrating. Additional 10-20 mg doses may be administered during infusion while achieving BP goals. The maximum dose is 300 mg in 24 hours. 3
Labetalol is a selective a1 beta-blocker and non-selective (3-blocker with an alpha/beta ratio of 1:7, hypotensive effect secondary to (3 blockade, decreases MAP, SBP, HR, CO, and has little effect on SVR (a1 blockade prevents SVR increase). In pre-existing cardiovascular disease, Labetalol reduces the perioperative ischemia by balancing the oxygen consumption and demand. It prevents ventricular arrhythmias and attenuates perioperative inflammatory markers and free radicals associated with acute coronary events. 3
The most common adverse effects are excessive blood pressure drop, bradycardia, AV conduction disturbances, left ventricular dysfunction, and bronchospasm. It is contraindicated in major AV block, cardiogenic shock, or CHF. 3
Esmolol
The onset of action is 6-10 min with a half-life of 10 - 20 min.
The starting dose is 0.5 mg/kg in bolus, continuing with 0.05 to 0.2 mg/kg/min in infusion. Increase 0.05 mg/kg/min every 5 min according to response and repeat bolus every 5 min. Maximum dose: 300 mcg/kg/ min.
It is a very short-acting cardioselective BB with an effect similar to labetalol. It decreases SBP and MAP, affects HR, CO, and stroke volume, decreases the left ventricular work and oxygen consumption, and has minimal effects on SVR. It has been used to manage perioperative HT after cardiac surgery and neurosurgery, particularly in patients with tachycardia. 3
Adverse effects: bradycardia, left ventricular dysfunction, bronchospasm, and excessive BP drop. Do not administer in patients with poor cardiac function or bronchospasm. 3
Calcium channel blockers (CCBs)
Although they are strong vasodilators, verapamil, diltiazem, nifedipine, nicardipine, and clevidipine are used in the perioperative period. Their half-lives vary from 1 minute for clevidipine, 50 min for nicardipine, 2-5 hours for verapamil, and 3-4 hours for diltiazem. Dihydropyridines bind to the L-type calcium channels in vascular smooth muscle, causing vasodilation and lowering of blood pressure. In contrast, non-dihydropyridines act on the L-type calcium channels of the myocardium and, to a lesser extend, on the vascular smooth muscle. 3 CCBs are associated with negative chronotropic effects and decreased sympathetic nervous system activity. 30
The ECLIPSE study compared the safety and efficacy of Clevidipine (a recent CCB currently unavailable in Colombia) with nitroglycerin, sodium nitroprusside, and nicardipine for the treatment of acute perioperative hypertension in cardiac surgery. Mortality was significantly lower with clevidipine when compared against sodium nitroprusside (1.7% vs. 4.7%, p = 0.04), but there were no significant differences in mortality with clevidipine vs. nitroglycerin or nicardipine. 35
Oral antihypertensives in perioperative HT
Nifedipine: capsules for sublingual use are not recommended due to their erratic absorption and exaggerated BP drop. The same results have been obtained with oral antihypertensives and therefore nifedipine is not recommended for the management of perioperative HT. 38
ACE inhibitors: 12.5-25 mg of sublingual captopril has a long duration of action. The short duration of perioperative HT suggests that doses should not be repeated in this context. Its effects include vasodilation, decreased sympathetic response, and vasodilation of the renal efferent arteriole with decreased sodium absorption leading to hemodynamic effects such as decreased MAP, SBP, DBP, and preload with little effect on CO and no reflex tachycardia. The potential adverse effects include prolonged hypotension (much more severe in hypovolemic patients), decreased renal function, hyperkalemia, and rarely angioedema. 38
Due to their cardiovascular effects, ACE inhibitors represent an alternative to Clonidine in perioperative HT. However, due to their prolonged time of action, caution should be exercised when using repeated doses (considered as an alternative). 38
Clonidine: 0.15 mg per mouth, repeat the dose every hour if necessary, maximum dose 0.6 mg. It is an a2 central acting agonist that reduces the activity of the central sympathetic nervous system with a decrease in BP and HR. It also has a sedative effect, which makes it an option for the perioperative period. The most common adverse effects are sedation and dry mouth. 39
Hypertensive crisis management
Urgent considerations: (Figure 4)
GOAL: BP <160/100 mmHg (the goal may vary depending on the patient's history and the cause of the HT). The patient may be discharged with recommendations for outpatient management and an appointment with the treating physician. Avoid IV antihypertensive drugs as much as possible.
Considerations in a hypertensive emergency: (Figure 4)
If there are no signs of fluid overload, consider a 10-20 ml/kg crystalloid bolus before pharmacological management.
GOAL: reducing the BP by 20% in the first hour; achieve 160/100 mmHg over the first 6 hours (more aggressive management can aggravate hypoperfusion and exacerbate TOD). Continuous monitoring of vital signs, including urinary output.
Special conditions
Cardiothoracic surgery BP goal: <140/90 and MAP: 105 mmHg.
Thyroidectomy: initiate antihypertensive management with SBP ≥150 mmHg.
Patients with coronary artery disease, high risk of pulmonary edema, or established edema, consider nitroglycerin as an adjunct in the management of hypertensive crisis. Labetalol is considered the antihypertensive of choice in AMI, aortic dissection, ischemic stroke, and hypertensive encephalopathy. 3
CONCLUSION
HT is a frequent pathology in the surgical environment. The existence of TOD and the type of surgery must always be considered. If surgery is an option, it is essential to avoid BP fluctuations and to actively treat any potetial causes. Patients with a BP <160/100mmHg could receive outpatient management during the postoperative period if the other clinical conditions are favorable.
ACKNOWLEGMENTS
Contributions by the authors
JDLPdL, JHMM, CACM, LJLE and GACS: Conception, work design, literature search and review, analysis and interpretation of the data; drafting of the document, critical revision, final approval. AAS: Drafting of the document, critical revision, and final approval.











 text in
text in