What do we know about this topic?
Hip fracture is one of the main causes of morbidity and mortality among the elderly population.
Timely surgical treatment before 48 hours improves the success of the intervention in terms of reducing complications and mortality.
There are a number of international scientific associations that collect information about perioperative management for improving the standards of care. However, there is a lack of evidence in the Colombian healthcare institutions.
What does this study contribute with?
This study offers the opportunity to learn about the characteristics of the population with hip fractures at a tertiary healthcare institution in the southwestern region of Colombia.
Spinal anesthesia is the most widely used technique for surgical procedures in this population.
The most frequent outcomes identified in this tertiary care institution are delirium and acute kidney failure.
Four out every five patients undergo surgery before 48 hours, with a low intra-hospital mortality.
INTRODUCTION
Hip fracture (HF) is one of the primary causes of morbidity and mortality among the elderly population and represents a public health problem because of its frequency and high socio-economic cost. 1 The annual incidence in Colombia has been estimated at 8,000 to 10,000 cases. Moreover, there has been an increase among the population over 65 years old, from 7.68% in 2005 to 8.5% in 2020. 2
Timeliness of a surgical treatment over the first 24-48 hours after the diagnosis significantly improves the success of the intervention. 3,4 Perioperative management involves the comprehensive healthcare practice during the surgical procedure. 5 Some of the big perioperative challenges are the choice of the anesthesia technique 6, the pharmacological reversal of anticoagulated patients 7, the anti-platelet therapy 8 and the assessment and optimization of any underlying pathologies prior to the surgical procedure. 9
Notwithstanding the knowledge about multiple factors inherent to the health status, such as old age, the socio-economic condition, history of diseases 10, and the factors associated with the perioperative care of patients with HF, there are few studies in Colombia addressing the socio-demographic and clinical characteristics to strengthen the management protocols, and to allow for improved quality of care and better health outcomes. 11 The purpose of this study is to explain the perioperative management of patients with HF and to document the clinical outcomes observed at a tertiary university hospital in Cali, Colombia.
METHODS
A retrospective, observational, cohort study was conducted in a historical cohort of patients diagnosed with HF and undergoing surgical management.
A non-probability sampling method was used for patients with HF admitted to the emergency department and receiving surgical management between January 2018 and June 2022. Both male and female patients over 18 years old with HF were included; these patients were admitted to the institution according to their diagnosis and underlying pathologies (assessed by the emergency department physician, internal medicine, orthopedics and geriatrics). Pregnant women, patients with a diagnosis of osteogenesis imperfecta, and defined multiple trauma patients (i.e., patients with head and neck trauma, thoraco-abdominal blunt or open trauma) concomitant with the HF at the time of admission, were excluded.
The patients that met the inclusion criteria were selected upon approval of the research protocol. The information was collected by three trained investigators. The information was uploaded into the electronic database available in the institutional digital platform (BDClinic), and the databases were analyzed in order to address each of the specific objectives. 10% of the data were randomly selected to assess the quality of the information, and were compared against the source documents (medical record).
Primary outcomes: The primary outcome was the identification of delirium recorded in the medical record or suspicious of the event during the immediate postoperative period until discharge; acute kidney failure defined as a diuresis < 0.3 cm3/kg/h during 24 hours and/or an increase in serum creatinine of twice the baseline level, and the need for postoperative Intensive Care Unit (ICU) monitoring. Finally, intra-hospital mortality also was taken into account.
Secondary outcomes: these considered the need for anti-fibrinolytics use, vasoactive support requirements, use of intraoperative blood products, ICU length of stay, stroke diagnosis, surgical site infection, diagnosis of pneumonia within 48 hours after hospital admission, and/or pulmonary thromboembolism during hospitalization, diagnosis of acute myocardial infarction and non-fatal cardiac arrest.
Once the quality of the information was ascertained, a univariate analysis was conducted to determine the behavior of the numerical variables. The data on asymmetric quantitative variables were submitted as medians and interquartile ranges. With regards to the categorical variables, absolute and relative frequencies were submitted; contingency tables were developed intended to describe the relationships between the clinical and demographic characteristics and the management of anesthesia against the postoperative outcomes based on the exact Fisher's test or the Pearson Chi square test. In order to compare the average length of hospital stay with the perioperative variables, a Student-t test was conducted for parametric distribution variables.
This study was approved by the Ethics in Biomedical Research Committee of the Fundación Valle del Lili, according to the administrative act No. 17 of August 16, 2022. Because of the retrospective nature of the study and pursuant to Article 11 of Resolution 8430 of 1993 of the Colombian Law, this study was considered "no risk", and hence did not require signing of an informed consent.
RESULTS
235 patients undergoing surgery between January 2018 and June 2022 were included. The demographic and clinical characteristics of the population are shown in Table 1. The mean age was 79 years and 57% (n=134) were males. 7.7% (n=18) of the patients had been receiving anticoagulation therapy and 16.6% (n=39) were taking antiplatelet medication such as aspirin and P2Y12 inhibitors.
Table 1 Socio-demographic and clinical characteristics.
| Variable | Sample size (n = 235) |
|---|---|
| Age and gender | |
| Age ⴕ | 79 (62 - 92) |
| Females ꭞ | 101 (43.0) |
| Males ꭞ | 134 (57.0) |
| ASA Classification | |
| ASA Iꭞ | 29 (12.3) |
| ASA IIꭞ | 89 (37.9) |
| ASA IIIꭞ | 101 (43.0) |
| ASA IVꭞ | 16 (6.8) |
| History | |
| Strokeꭞ | 15 (6.4) |
| Anemiaꭞ | 113 (48.1) |
| Antiplatelet therapyꭞ | 39 (16.6) |
| Anticoagulationꭞ | 18 (7.7) |
| Dementiaꭞ | 54 (23.0) |
| Diabetes mellitus type 2ꭞ | 46 (19.6) |
| Cancer ꭞ | 25 (10.6) |
| Chronic kidney disease ꭞ | 21 (8.9) |
| Hypertensionꭞ | 133 (56.6) |
| CHF* LVEF** < 40 %ꭞ | 5 (2.1) |
| Obesity ꭞ | 21 (8.9) |
| Nursing home ꭞ | 15 (6.5) |
| Type of fracture | |
| Extracapsular ꭞ | 160 (68.1) |
| Intracapsular ꭞ | 75 (31.9) |
| Pre-surgical care | |
| Request for TT ECG *** | 23 (9.8) |
| Pre-surgical assessment by IM **** | 133 (56.6) |
*CHF = Congestive heart Failure, **LVEF = Left ventricular ejection fraction. ***transthoracic ECG, ****IM = Internal medicine, ⴕ Median (interquartile range), ꭞn (%).
Source: Authors.
68.1% (n=160) of the patients experienced an extracapsular fracture. In 83.7% (n=196) of the patients, the time elapsed since admission to the emergency department and the surgery was less than 48 hours, whilst in 64.5% (n=150) less than 48 hours elapsed between the time of the trauma and/or fracture and the surgical procedure. The time elapsed from the moment of the fracture, the admission to the emergency department, and the choice of the anesthetic technique are illustrated in Figure 1 and in Table 2.
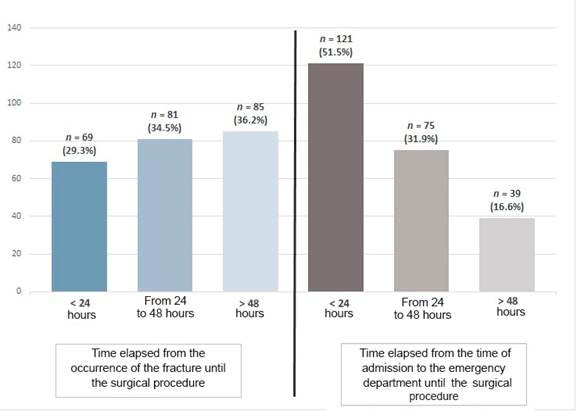
Source: Authors.
Figure 1 Time elapsed from the occurrence of the fracture and admission to the emergency department, until the surgical procedure.
Table 2 Intraoperative characteristics.
* Continuous norepinephrine infusion ꭞ n (%), ᵎ n.
Source: Authors.
31.1% (n = 73) of the patients required a continuous norepinephrine infusion, and 12.8% (n=30) required invasive blood pressure monitoring during the intraoperative period. Tranexamic acid was administered to 23.8% (n = 56) of the patients. Blood products transfusion was administered based on the opinion of the treating anesthesiologist in 5.5% (n=13) of the patients. The intraoperative variables of the patients are shown in Table 2.
22.1% (n=52) of the patients needed to be transferred to the ICU during the postoperative period, with a mean length of stay of 3 days (IQR 2-4) (Table 3). The need for ICU transfer was associated with old age, ASA III-IV classification, a history of cardiovascular disease, chronic kidney disease, dementia, time of patient admission to the emergency department until surgery of more than 48 hours, need for vasoactive support, and use of general anesthesia (Table 4). The mean hospital stay until discharge was 4 days (IQR 3-7).
Table 3 Outcomes during the hospital stay.
* ICU = Intensive care unit, ⴕ Median (interquartile range), ꭞ n ( %).
Source: Authors.
Table 4 Factors associated with the outcomes assessed.
| Variable | Outcome | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Delirium | Kidney failure | ICU* requirement | Intra-hospital mortality | |||||||||
| Yes (n = 42) | No (n = 193) | P value | Yes (n = 16) | No (n = 219) | P value | Yes (n = 52) | No (n = 183) | P value | Yes (n = 6) | No (n = 229) | P value | |
| Age ⴕ | 85 (80 - 90) | 78 (62 - 84) | 0.001 | 90 (80 - 92) | 78 (63 - 85) | 0.001 | 84 (73 - 89) | 78 (63 - 84) | 0.023 | 91 (85 - 92) | 79 (65 - 85) | 0.009 |
| ASA classification | 0.005 | 0.014 | 0.001 | 0.063 | ||||||||
| ASA Iꭞ | 1 (2.4) | 28 (14.5) | - | 0 | 29 (13.2) | - | 2 (3.8) | 27 (14.8) | - | 0 | 29 (12.7) | - |
| ASA IIꭞ | 13 (31.0) | 76 (39.4) | - | 5 (31.2) | 84 (38.4) | - | 9 (17.3) | 80 (43.7) | - | 2 (33.3) | 87 (38.0) | - |
| ASA IIIꭞ | 21 (50.0) | 80 (41.5) | - | 7 (43.8) | 94 (42.9) | - | 31 (59.6) | 70 (38.3) | - | 2 (33.3) | 99 (43.2) | - |
| ASA IVꭞ | 7 (16.7) | 9 (4.7) | - | 4 (25.0) | 12 (5.5) | - | 10 (19.2) | 6 (3.3) | - | 2 (33.3) | 14 (6.1) | - |
| Strokeꭞ | 3 (7.1) | 12 (6.2) | 0.9 | 1 (6.2) | 14 (6.4) | 0.9 | 8 (15.4) | 7 (3.8) | 0.007 | 0 | 15 (6.6) | 0.9 |
| Pre-operative anemia ꭞ | 29 (69.0) | 84 (43.5) | 0.005 | 15 (93.8) | 98 (44.7) | 0.001 | 36 (69.2) | 77 (42.1) | 0.001 | 3 (50.0) | 110 (48.0) | 0.9 |
| Dementiaꭞ | 21 (50.0) | 33 (17.1) | 0.001 | 6 (37.5) | 48 (21.9) | 0.3 | 19 (36.5) | 35 (19.1) | 0.014 | 5 (83.3) | 49 (21.4) | 0.002 |
| Diabetes mellitus type 2ꭞ | 9 (21.4) | 37 (19.2) | 0.9 | 7 (43.8) | 39 (17.8) | 0.028 | 18 (34.6) | 28 (15.3) | 0.004 | 1 (16.7) | 45 (19.7) | 0.9 |
| Chronic kidney diseaseꭞ | 6 (14.3) | 15 (7.8) | 0.3 | 9 (56.2) | 12 (5.5) | 0.001 | 9 (17.3) | 12 (6.6) | 0.034 | 1 (16.7) | 20 (8.7) | 0.9 |
| Hypertension ꭞ | 33 (78.6) | 100 (51.8) | 0.003 | 14 (87.5) | 119 (54.3) | 0.02 | 32 (61.5) | 101 (55.2) | 0.5 | 5 (83.3) | 128 (55.9) | 0.4 |
| CHF** LVEF*** < 40 %ꭞ | 0 | 5 (2.6) | 0.6 | 1 (6.2) | 4 (1.8 %) | 0.8 | 4 (7.7) | 1 (0.5) | 0.009 | 1 (16.7) | 4 (1.7) | 0.3 |
| Time from admission to the emergency department until surgery of more than 48 hours ꭞ | 10 (23.8) | 29 (15.0) | 0.4 | 4 (25.0) | 35 (16.0) | 0.5 | 15 (28.8) | 24 (13.1) | 0.016 | 2 (33.3) | 37 (16.2) | 0.2 |
| Time from the occurrence of fracture until surgery of more than 48 hours ꭞ | 20 (47.6) | 65 (33.7) | 0.2 | 8 (50.0) | 77 (35.2) | 0.2 | 26 (50.0) | 59 (32.2) | 0.059 | 80 (34.9) | 5 (83.3) | 0.046 |
| Anesthetic technique | 0.2 | 0.9 | 0.001 | 0.006 | ||||||||
| General anesthesia ꭞ | 9 (21.4) | 52 (26.9) | - | 4 (25.0) | 57 (26.0) | - | 27 (51.9) | 34 (18.6) | - | 0 | 61 (26.6) | - |
| General + regional anesthesia ꭞ | 2 (4.8) | 16 (8.3) | - | 1 (6.2) | 17 (7.8) | - | 3 (5.8) | 15 (8.2) | - | 0 | 18 (7.9) | - |
| Spinal anesthesia ꭞ | 24 (57.1) | 77 (39.9) | - | 6 (37.5) | 95 (43.4) | - | 13 (25.0) | 88 (48.1) | - | 1 (16.7) | 100 (43.7) | - |
| Spinal + regional anesthesia ꭞ | 7 (16.7) | 48 (24.9) | - | 5 (31.2) | 50 (22.8) | - | 9 (17.3) | 46 (25.1) | - | 5 (83.3) | 50 (21.8) | - |
| Use of antifibrinolytics ꭞ | 8 (19.0) | 48 (24.9) | 0.5 | 2 (12.5) | 54 (24.7) | 0.4 | 7 (13.5) | 49 (26.8) | 0.071 | 0 | 56 (24.5) | 0.4 |
| Invasive blood pressure monitoring ꭞ | 13 (31.0) | 17 (8.8) | 0.001 | 4 (25.0) | 26 (11.9) | 0.3 | 28 (53.8) | 2 (1.1) | 0.001 | 3 (50.0) | 27 (11.8) | 0.032 |
| Need for vasopressor support ꭞ | 18 (42.9) | 55 (28.5) | 0.1 | 3 (18.8) | 70 (32.0) | 0.4 | 28 (53.8) | 45 (24.6) | 0.001 | 3 (50.0) | 70 (30.6) | 0.6 |
*ICU = Intensive Care Unit, **CHF =Congestive Heart Failure, ***LVEF = Left Ventricular Ejection Fraction, ⴕ Median (interquartile range), ꭞ n (%).
Source: Authors.
The intra-hospital mortality was 2.6% (n = 6), and was associated with a history of dementia, more than 48 hours between the occurrence of the fracture and surgery, the use of spinal anesthesia and older age (Table 4). The most frequent outcomes were postoperative delirium diagnosed in 17.9% (n = 42) of the patients, followed by acute kidney failure in 6.8% (n=16). The bivariate analysis showed a statistically significant relationship of these outcomes with older age, ASA III and IV classification, a history of high blood pressure, and preoperative anemia. The analysis of the factors associated with the outcomes assessed are illustrated in Table 4.
DISCUSSION
HF is a frequent pathology among the elderly population. In the world context, the likelihood of a hip fracture increases by 3.1 % in males and by 18.2 % in females over 65 years old. 12 In Colombia, the incidence is estimated at 8,000 and 10,000 cases per year. 2 In this study, an average of 4.3 cases of patients undergoing surgery per month was estimated, which is similar to the average of 4.8 cases per month reported in a tertiary hospital in the study conducted by Caicedo et al., in another city in Colombia. 13
Some of the characteristics of the patients with HF undergoing surgical management in the population herein studied are different from the characteristics described in the literature. The mean age of 79 years is lower than what is reported in a British database which is 83 years 14. This may be due in part to the longer life expectancy in developed countries. Also noteworthy is the gender-based incidence, since according to the literature, women present with hip fractures more often than men because of osteoporosis 15; in this paper, the proportion between males and females was similar.
The high burden of the disease becomes obvious according to the ASA classification, indicating that most of these patients exhibit at least one chronic condition as a comorbidity when they come to receive medical care because of the HF, and this is consistent with literature. 14 This fact is a challenge for the medical team. As shown in the results of this study, some patients require a preoperative assessment by internal medicine to optimize or control their underlying pathologies, as well as a transthoracic ECG to stage the cardiovascular risk of the patient. It should be highlighted that such interventions, particularly the ECG are not recommended on a routine basis, since it has been shown that reducing the time elapsed to administer care not only lowers the morbidity and mortality, but also shortens the hospital stay and improves patient satisfaction 16,17; hence, the ECG is only reserved for patients with a high burden of cardiovascular morbidity, for example in patients with suspicious heart failure, severe valve disease and/or significant decline of the functional class since their last ECG. 18 The current recommendation is to conduct a preoperative ECG pursuant to the medical opinion of the multidisciplinary team, based on institutional protocols developed in accordance with the scientific evidence. 19,20
In 16.6% of the patients there was a delay of more than 48 hours between their admission to the emergency department of the institution and the surgical procedure, which is a shorter time as compared to the time elapsed between admission to the emergency department and surgery as described by Caicedo et al., in a tertiary Colombian hospital, where the mean delay was more than 4 days. 13 In the study by Moran et al., the percentage of patients who experienced a delay of more than 48 hours from the time of admission to the emergency department was 7.9% 21, suggesting a wide variability among the various health centers. Among the probable causes for the delay of surgery there is the acute decompensation of conditions such as hypertension, diabetes mellitus type 2 and congestive heart failure, which require complementary assessments and preoperative management.
The results of this study indicate that 36.2% of the patients underwent surgery after 48 hours of the trauma event, which is consistent with other reports with regards to delays, such as Smektala et al., who reports that 31.6% of the patients has a waiting time of over 48 hours from the time of fracture until the surgical intervention. 22 This paper collected the potential causes for such delay, which included adjournment of the visit to the emergency department and consults with healthcare centers that were unable to deliver comprehensive care and referred the patient to the institution.
The discussion about the selection of the anesthesia technique is extensive and there is no consistency favoring any particular anesthetic approach. Scientific associations such as NYSORA and ASRA tend to favor regional anesthesia in addition to multimodal analgesia for the management of patients with HF. 23,24 The recommendations of the clinical guidelines focus on improving the practice within each technique, which involves adjusting for the appropriate dosing of medications based on age, the joint administration of regional block as part of multimodal analgesia, and a careful intraoperative blood pressure control. 25 In this study, the most frequently used technique was pure spinal anesthesia, or in combination with a regional block as an adjuvant for the management of analgesia, as part of the multimodal analgesia strategy. The criteria regarding the choice of the anesthetic technique was not assessed in the study; however, one may assume that to a large extent, the experience of the anesthesiologist in charge of the case and the patient's comorbidities play a key role.
Among the postoperative outcomes, the most frequent complication was delirium in 17.9% of the patients. This percentage is similar to that described in a multicenter study conducted in the United States and Canada, which compared general anesthesia vs. spinal anesthesia in patients with HF, with an incidence of delirium of around 20%, with no statistical difference between the two groups. 26 Delirium was associated with preoperative anemia, a history of dementia, progressively older patients, and a high burden of morbidities based on the ASA classification.
Kidney failure was the second most frequent complication among the population in this study, with a 6.8%. An incidence between 4.5% and 7.6% of acute kidney failure has been described in patients with HF undergoing surgery 26, which is consistent with the results herein discussed. Furthermore, the percentage obtained in similar to the 8.1 % reported in a study conducted on the incidence of acute kidney failure in major surgery. 27
The frequency of surgical site infection described in the literature is of 0.3% 26. This complication was not present in this study during the study period. Although having cero surgical site infections is encouraging, the compliance with the protocols of asepsis and antisepsis, and the standardized use of antibiotic prophylaxis during the observation period, could have had an impact.
Another aspect that has given rise to a significant controversy in the perioperative management of patients with HF is the anticoagulation and antiplatelet therapy. In accordance with the current evidence, it is clear that there is no need to adjourn surgery in patients with HF receiving antiplatelet therapy as monotherapy or dual anti-aggregation with aspirin plus a P2Y12 receptor inhibitor such as clopidogrel, prasugrel and ticagrelor. 28,29 In patients anticoagulated with warfarin or direct oral anticoagulants, the surgical procedure should not be deferred for more than 48 hours, individualizing the approach for each patient. 30,31 No significant statistical relationship was found in this study between the history of anticoagulation and/or antiplatelet therapy with the outcomes assessed. One of the causes for a longer than 48-hour delay between the time of fracture and surgery was the referral of patients with dual antiplatelet therapy or anticoagulated from other healthcare institutions.
Occasionally, patients may require ICU monitoring after surgery. 32 Consequently, some management guidelines recommend having an ICU available in the institutions that take care of patients with HF. 33 In this study, 22.1% of the patients required postoperative ICU monitoring, which contrasts with a multicenter study conducted in the United States and Canada where the postoperative ICU requirement was 2.3% and 3.7%, respectively. 26 This difference may be due to differences in the level of complexity of the institutions where the studies were conducted, and to the high burden of morbidity of the patients, since in this case we were dealing with a referral center in the southwestern region of Colombia.
When comparing the number of hospitalized days, an average of 4 days (IQR 3-7) was identified in the institution, similar to the length of stay described in the study from the United States with a mean of 3 days (IQR 2-5) and 6 days (IQR 4-9) in the centers in Canada. According to the authors, the difference between the two countries reflects the differences in clinical practice. 26
The mortality until hospital discharge for the population in this study was 2.6%, as compared to the 5% documented in a study by Nurmi et al., in Finland, early in 2000. 34 This difference in intrahospital mortality is probably due to the improved healthcare protocols, the technological progress with regards to monitoring and the safe use of medications in the anesthetic techniques, since the population characteristics in terms of age and ASA classification are similar in both studies.
The bivariate analysis of the intrahospital mortality outcome showed raw associations with a history of dementia and with the time elapsed since the occurrence of the fracture until the surgical procedure which exceeded 48 hours; this is consistent with the literature. 10 Furthermore, a significant relationship was established with the spinal anesthesia technique, which could probably be explained based on the intent of the anesthesiologist to avoid general anesthesia in elderly patients, with a history of dementia and increased morbidity. None of these associations has a causal interpretation.
In terms of the limitations, this study was conducted in a single center in the city; however, the institution is a referral center for lower level hospitals in the southwestern region of the country. Multiple trauma was considered to extend the hospital stay and affected decision-making vis a vis the management of the hip fracture; hence, this exclusion criteria also reduced the size of the sample of the population. Moreover, due to the nature of the study, no further follow-up was conducted after discharge and hence mortality and outcomes were only considered until the patient's discharge. Finally, in contrast to a study conducted at the San Ignacio University Hospital in Bogotá, where malnutrition and functional disability were considered as independent variables for morbidity and mortality in patients with HF 35, these variables were not measured in the study herein discussed.
The results enable the characterization of the population with hip fracture in a tertiary healthcare institution in the southwestern region of Colombia, emphasizing that most of these patients are elderly individuals with a high burden of morbidity as evidenced by the ASA III and IV classification; these characteristics have been described as independent factors for morbidity and mortality. Moreover, they allow for the identification of opportunities for improvement in care, such as improving timeliness of surgery. The expectation is that this study may contribute to the development of protocols and/or clinical management guidelines based on scientific evidence, to lower the incidence of unfavorable outcomes in patients.
ETHICAL RESPONSIBILITIES
Ethics Committee approval
This study was approved by the Ethics in Biomedical Research Committee of Fundación Valle del Lili, through administrative Act 17 of August 16, 2022.
Protection of Humans and Animals
The authors declare that no experiments in human beings or animals were conducted for this research project. The authors declare that the procedures followed were consistent with the ethical standards of the responsible human experimentation ethics committee and pursuant to the World Medical Association and the Declaration of Helsinki.
Confidentiality of the data
The authors declare that they followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent
The authors declare that no patient data are disclosed in this article. Given the retrospective nature of the study, and in accordance with Article 11 of Resolution 8430 of 1993 of the Colombian Law, this study was considered "no risk", hence voiding the requirement for a signed informed consent.
ACKNOWLEDGEMENTS
Contributions of the authors
IFQC, GACS, ESBV and MM: Planning of the study, interpretation of the results and drafting of the manuscript.
JJCR: Planning of the study, data collection, interpretation of the results and drafting of the manuscript.
DFVC: Data collection, interpretation of the results and drafting of the manuscript.
AAS: Planning of the study, data collection, interpretation of the results.











 texto en
texto en 



