What is known about this problem?
In Colombia there is an open debate regarding the length of the anesthesia specialization program.
The number of cases or procedures a resident must perform during training has not been defined.
ASCOFAME, in an academic consensus, has suggested minimum numbers; however, it is uncertain whether they are consistent with the reality of residents in the country.
INTRODUCTION
A debate is open regarding the ideal duration of graduate anesthesia programs, which currently ranges between three and four years in Colombia. It is argued that an additional year allows for in-depth, higher-complexity practice consistent with the development of the specialty 1,2, as well as higher exposure to areas such a trauma and neonatal anesthesia. On the other hand, government regulations in Colombia prevent a resident physician from doing more than 66 hours of clinical work 3, impacting the number of practice cases and learning quality, and leading to the assumption that three years would be insufficient for adequate training.
The learning model in the world has been shifting for years towards a competency-based model 4,5. It is clear that case numbers and time are no guarantee that the individual will acquire the competencies of the speciality 6, but they are an indicator of the opportunities offered by the programs to ensure such acquisition 7.
However, there is no information in Colombia about the minimum number or the type of surgeries that the anesthesia resident must perform. Some groups have proposed the use of learning curve cumulative summation, but this method only allows to determine the minimum number of attempts the student has to make in order to acquire a specific psychomotor competency 8. In 2016, the Colombian Association of Medical Schools 1 published some suggested numbers; however, they are not a binding standard and education institutions are autonomous when it comes to setting numbers 9, making the standardization process and the assessment of graduate programs even more challenging. In contrast, programs in other countries, as is the case of the United States, are clearer in establishing these thresholds 10.
The objective of this study was to describe exposure to procedures performed by resident physicians attending a three-year anesthesia specialization program in Colombia between 2015 and 2020, and to compare with the standards proposed by ASCOFAME and ACGME.
METHODS
Cross-sectional study approved by the Ethics Committee of Universidad del Rosario under entry DVO005 953-CV1129 of the 6th of November, 2019. Anesthesia logs of the residents who completed the three years of training in the anesthesia program of Universidad del Rosario under the Fundacion Cardioinfantil (Bogota, D.C.) curriculum were reviewed.
The population and the sample consisted of 16 resident physicians who documented 11,711 procedures during the study period. No sample size was calculated and no sampling method was used. Residents with completed anesthesia records for the entire three years of training during the period between January 1, 2015, and January 30, 2020, were included as study subjects. Log entries with consistent information reflecting direct resident involvement in the case during more than 75% of the time were considered valid.
The log used in the study was consistent with the official form of the Anesthesiology Department (FCI 2.0 Log Book available at: http://www.ddhsoftware.com/gallery.html?show=number&record=4856).
The information was collected in the HanDbase v4.9.079 2018 DDH Software LLC and completed by each of the residents in their mobile devices. The validity of the information was assumed to be higher if data entry was a mandatory requirement for the award of the specialist degree by the University.
Log data were edited to remove all information that could identify the patients, before they were exported and merged in a Microsoft Excel worksheet. Sociodemographic variables associated with patient age and complexity were included; patients were classified - based on the American Society of Anesthesiologists (ASA) anesthetic risk -according to the type of surgical procedure, surgical specialty, anesthesia technique, type of vascular access, invasive monitoring and airway approach. A descriptive analysis of the information was carried out, and frequencies and percentages of each of the procedures performed by the individual residents were presented, taking into account medians and interquartile ranges (IQR) for the total number of cases. To compare the results with the minimum numbers established by ASCOFAME 1 and ACGME (10), data were grouped according to surgical specialty, anesthetic risk and type of vascular access and then reviewed against estimated median values for each category using the criteria established by both organizations. Finally, proportions descriptively meeting the criteria were estimated.
RESULTS
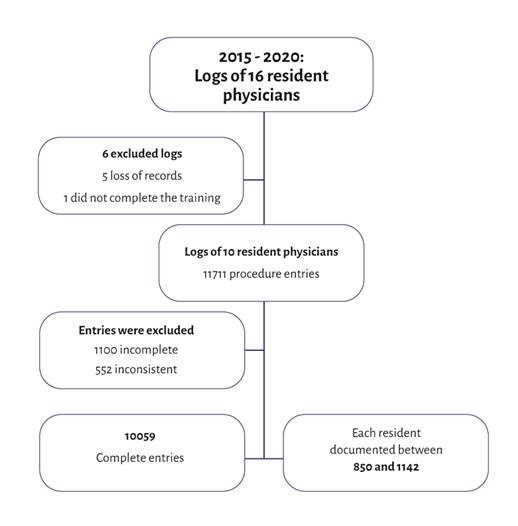
During the study period (between January 1, 2015, and January 30, 2020) 6 out of the 16 residents were excluded because of incomplete records resulting from partial or total loss of cases. The records of the 10 residents included in the study yielded 11,711 anesthesia procedures; of these, 1,100 were considered incomplete and 552 were inconsistent and were excluded from individual resident analyses. Overall, 10,059 procedures that met the inclusion criteria were analyzed (Figure 1).
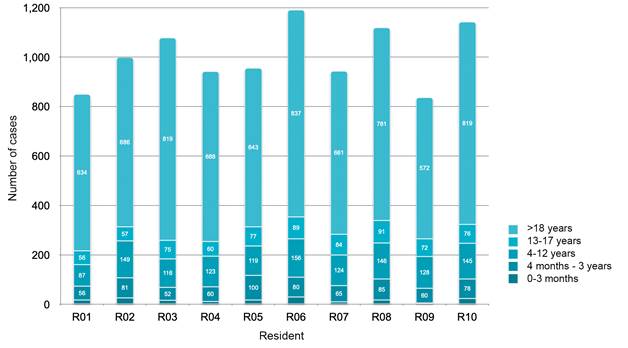
The median number of cases per resident was 978 (IQR [943-110]). Distribution by specialty is shown in Figure 2. Specialties to which residents were most frequently exposed were general surgery and orthopedic surgery with a median of 175 (IQR [152-219]) and 161 (IQR [138-186]), respectively. It is worth highlighting that the residents performed a large number of obstetric cases (125, IQR [67-149]), taking into account that this is an extramural rotation. There was higher exposure to procedures in adult patients, with a mean of 688 (IQR [648-819]) (Figure 3).
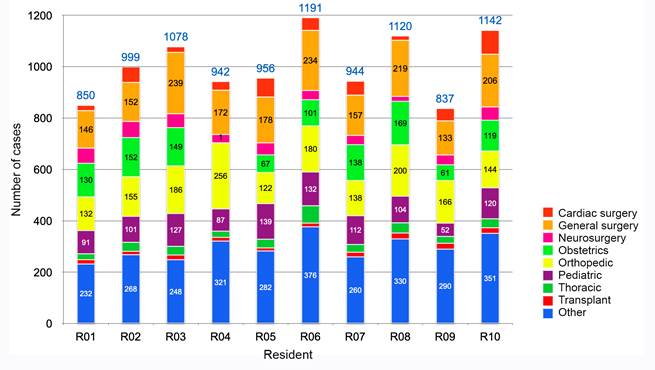
Others: Dermatology, Pain, Electrophysiology, Gastroenterology, Gynecology, Interventional cardiology, Hepatobiliary surgery, Pulmonology, Dentistry, Ophthalmology, Oncology, Plastic surgery, Radiology, Organ procurement, Urology and Vascular Surgery. Source: Authors.
Figure 2 Case distribution with resident participation by surgical specialty.
The complexity of the patients who received anesthesia with resident involvement was assessed in accordance with the ASA risk classification. Residents were primarily involved in cases classified as ASA II, median 389.5 cases (IQR [371430]), ASA I, 297.5 cases (IQR [232-304]), and ASA III, 276 casos (IQR [254-313]), and had a lower exposure to ASA IV patients, 31 cases (IQR [27-45]).
Anesthetic techniques
The most frequent anesthetic technique used in cases in which residents were involved was general balanced anesthesia. This technique was used by the residents in a median of 772 cases (IQR [660-829]), followed by spinal anesthesia with a median of 104 cases (IQR [94-116]), sedation in 80 cases (IQR [65-86]), peripheral nerve block in 65 cases (IQR [61-70]), peridural anesthesia in 46 cases (IQR [(40-49]), and total intravenous anesthesia (TIVA) in 29 cases (IQR [18-33]).
Airway management
In terms of airway management, orotracheal intubation was the most frequent, used in a median of 654 cases (RIC [568-705]), followed by laryngeal mask (LMA) placement in 89 cases (IQR [77-111]). On the other hand, the laryngoscope was the most frequently used device for orotracheal tube placement in 614.5 cases (IQR [551-669,5]), followed by the videolaryngoscope in 23 cases (IQR [17-30]), Bonfils in 19 cases (IQR [14-34]), and fiberoptic bronchoscope in 9 cases (RIC [8-20]), used most of the time to confirm that the double lumen tube was correctly placed.
Invasive monitoring
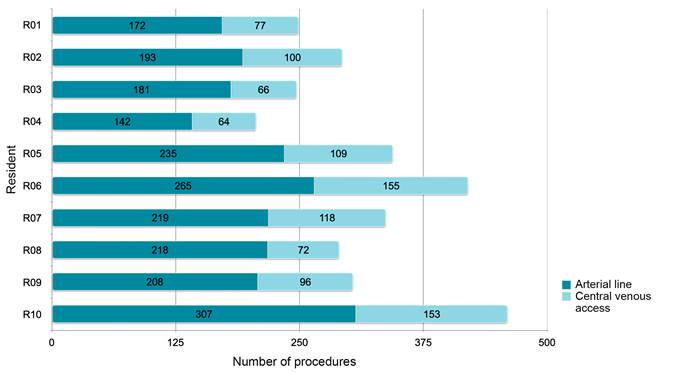
Some form of invasive monitoring was required in 21.3% of cases (Figure 4). Arterial catheter was the most frequently used arterial access for invasive monitoring in anesthetic procedures in which the residents in the study group were involved, with a median of 213 cases (IQR [184231]). Ultrasound guidance was used for placement of 20% of the arterial lines, versus 41% of central venous lines.
Comparison with ASCOFAME and ACGME
When comparing the number of procedures performed versus the ASCOFAME suggestion, exposure was the same or greater than recommended in 6 of the 10 surgical specialties reviewed. The emergency category was not analyzed because it was not entered in the log. The same applied to maxillofacial surgery which was included under dentistry, hindering discrimination of only maxillofacial procedures.
In terms of compliance with the minimum proposed numbers, only in 3 specialties did 100% of the cohort achieve the number, while in 3 specialties none of the residents complied with the requirements. In terms of specialty-specific procedures, 100% exceeded the threshold suggested by ASCOFAME (Table 1).
Table 1 Comparison between cases and procedures with involvement of the residents included in the study and minimum numbers recommended by ASCOFAME.
| Criterion | Minimum number of procedures ASCOFAME | Study group (Median) | Percentage of the cohort that met the requirement |
|---|---|---|---|
| Specialty | |||
| Emergencies in different surgical specialties | 200 | Not available | |
| General surgery | 200 | 175 | 40.00 % |
| Obstetrics | 200 | 146 | 0 % |
| Pediatric surgery | 100 | 108* | 70.00 % |
| Orthopedics | 100 | 185* | 100 % |
| Gynecology | 50 | 20 | 30.00 % |
| Plastic surgery | 40 | 24 | 0 % |
| Ophthalmology | 40 | 12 | 0 % |
| Otolaryngology | 40 | 42* | 60.00 % |
| Urology | 40 | 31 | 20.00 % |
| Neurosurgery | 40 | 43* | 60.00 % |
| Maxillofacial surgery | 20 | Not available | |
| Thoracic surgery | 20 | 34* | 100 % |
| Cardiovascular | 10 | 49* | 100 % |
| Specific procedures | |||
| Local and regional anesthesia | 40 | 65* | 100 % |
| Central venous catheterization | 30 | 98* | 100 % |
| Arterial catheterization | 30 | 213* | 100 % |
| TOTAL | 1200 | 978 |
* Exceeded criterion.
Source: Authors.
When benchmarking against ACGME criteria, the study population completed the minimum number of cases proposed for the age group, in the obstetric anesthesia and cardiac surgery categories. The recommended minimum was not reached for major vascular surgery, which was the category with the lowest completion percentage by the study group (only 20%), followed by pediatric surgery (70%), the use of cardiopulmonary bypass (80%) and neurosurgery (90%). Finally, 100% had adequate exposure in all the specialty-specific procedure categories (Table 2).
Table 2 Comparison between cases performed by the residents and the minimum criteria proposed by the Accreditation Council for Graduate Medical Education.
| Reviewed criterion | Minimum number of procedures ACGME | Study group (Median) | Percentage of the cohort that met the requirement |
|---|---|---|---|
| Specialty | |||
| Pediatric surgery | 100 | 108 | 70 %* |
| Under 3 months of age | 5 | 17 | 100 % |
| 3 months to 3 years | 20 | 72 | 100 % |
| 3 to 12 years | 75 | 126 | 100 % |
| Obstetrics | 60 | 125 | 100 % |
| Vaginal delivery | 40 | 44 | 100 % |
| Cesarean section | 20 | 81 | 100 % |
| Cardiac surgery | 20 | 49 | 100 % |
| Cardiopulmonary bypass | 10 | 25 | 80 %* |
| Major vascular surgery | 20 | 17* | 20 %* |
| Non-cardiac thoracic surgery | 20 | 34 | 100 % |
| Neurosurgery | 20 | 43 | 90 %* |
| Specific procedures | |||
| Peridural catheter | 40 | 46 | 100 % |
| Spinal anesthesia | 40 | 104 | 100 % |
| Peripheral nerve block | 40 | 65 | 100 % |
* Not exceeded.
Source: Authors.
DISCUSSION
This is the first time exposure to cases and specialty-related procedures in a graduate anesthesia program is described in detail in Colombia. It is important to note that no data collection tool designed for comparison with ASCOFAME or ACGME was created at the start of the study. The residents performed a median number of 978 cases, which is less than the 1200 cases proposed by ASCOFAME; however, it is not clear whether the numbers proposed by this organization should be counted from an exclusionary perspective, because one same patient may be adjudicated exclusively in one category or, on the contrary, may be counted in several, overestimating the total number of cases. This is an important flaw of the proposed criteria given the lack of clear guidance on how to analyze them, which could explain why residents did not accomplish the proposed minimum numbers in seven of the thirteen surgical categories. Moreover, reporting emergency cases was not possible because this category was not considered in the database used as the source to obtain resident records.
In a similar study conducted in a three-year anesthesia program in the United States, one case could be included in several categories, reporting a median of 1,373 patients for the 2013 cohort and 1,394 for the 2014 cohort 11. In this study, cases were exclusionary, which could explain the difference in relation with the aforementioned study; also, at the time of performing the study, the limit in the United States was 80 hours per week, as described by Yamamoto 12.
Cardioinfantil is a high-complexity institution focused on comprehensive care of cardiovascular diseases and transplants, a favorable setting for the development of an anesthesia program. Residents are constantly exposed to patients in all age groups during their training, as well as to most surgical specialties, except those that are not an important focus, such as obstetrics and gynecology and maxillofacial surgery. A case in point is cardiovascular surgery, which has a time assignment in a rotation; however, it is not uncommon for a resident to participate in a case of this specialty at any point in time without being part of the rotation. This is a way to ensure exposure to sufficient and diverse numbers of cases during training, meeting the majority of the ACGME criteria, especially those pertaining to age groups, which were performed in sufficient numbers by the residents. Notwithstanding, it is important to highlight that, even though all the students met the criteria for patients under 3 months and 3 years, the number of cases in this group is not high, creating doubt on whether these criteria can actually be met in three-month pediatric anesthesia rotations.
Historically, tracking resident activity is considered a tool to monitor student activity with two aims in mind: first, ensure sufficient exposure to specific cases so that the students can acquire the necessary competencies for practice; second, as an indirect indicator of the quality of medical-surgical residency programs, given that it allows an objective comparison between two programs of a same specialty. 7 However, it is not easy to access or verify this information in Colombia, largely because of the absence of standardized systems for entering cases in the different residency programs, pointing to an opportunity of improvement in the specialty.
The study results provide an exposure baseline both in terms of numbers and types of cases in a residency program in Colombia. Although case numbers are not necessarily a guarantee of competency acquisition, they do allow to determine sufficient opportunities to acquire such competencies and establish a minimum nationwide requirement to be considered by the regulatory agencies, based on real data. Consequently, these results must be analyzed taking into consideration the limitations of this study, as described below.
To start with, the log was completed by the residents themselves and although it was a mandatory requirement, six of them (37%) had to be excluded from the study because of missing information; this was due to the fact that the database was stored in each of the mobile devices and data were retrieved periodically for analysis. This creates two significant limitations: partial loss of data if a resident loses the device before data migration, and potential underreporting and memory bias when data entry during the case is not mandatory. Other authors have described underreporting in up to 11% of cases when logs are filled by the residents 13, hence the recommendation to use a combined database that allows to verify the entries made by the resident against the administrative information of the department, as is being done currently with the second version of our database, revised to address this problem in our service 14. Second, since the parameters of the database were not consistent with the ASCOFAME categories, comparing the emergency procedure category was not possible.
This study represents only a single academic program carried out in a high-complexity hospital focused especially on the pediatric population, a characteristic that offers exposure to a diverse population in terms of age groups, surgical specialties and complexity level, enabling resident exposure to the minimum number suggested by ACGME during a three-year period. However, this might not be possible in programs carried out in lower complexity hospitals, hence the need to replicate the work in other programs in order to garner additional data.
It is important to point to the substantial variations in the number of procedures performed by the 10 residents in several categories: for example, in central vascular access, the resident with the highest number had 42% more exposure than the resident with the lowest number in that category. This finding was aso documented by Yamamoto 11, who argues that it can be explained on the basis of personal motivations of some residents who actively look for subspecialty or higher complexity cases. This underscores the importance of academic program coordinators to regularly review student logs and intervene promptly to ensure that the residents have sufficient exposure to acquire certain specific competencies. Finally, only resident exposure to different cases, patient types and specialty-associated procedures is described, without determining resident involvement in each of them. If the degree of involvement is determined, competency acquisition could be measured and it would also be possible to identify the residents who need help in acquiring certain skills.
CONCLUSION
This study sets a baseline of the number of cases performed by residents in a three-year anesthesia program in Colombia, meeting the minimum criteria established by the ACGME. This work can be used as reference for further research in this area.
ETHICAL RESPONSIBILITIES
Ethics Committee approval
The cross-sectional study was approved by the Ethics Committee of Universidad del Rosario, under entry DVO005 953-CV1129, of the 6th of November, 2019.
Protection of animals and human subjects
The authors declare that no experiments were performed on animals for this study. The authors declare that the procedures followed were in accordance with the ethical standards of the Responsible Human Experimentation Committee and of the World Medical Association and the Declaration of Helsinki.











 texto em
texto em