Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Facultad Nacional de Salud Pública
versión impresa ISSN 0120-386X
Rev. Fac. Nac. Salud Pública vol.32 no.2 Medellín mayo/ago. 2014
Revisión de tema
The influence of breastfeeding on children’s health, well-being and development: A theoretical and empirical review
La influencia de la lactancia materna en la salud infantil, el bienestar y el desarrollo: una revisión teórica y empírica
Ana M. Rocha1; Raquel V. Oliveira2;Isabel Leal3
1 Instituto Superior de Psicologia Aplicada (ISPA).Correo electrónico: uipes@ispa.pt
2 Unidade de Investigação em Psicologia e Saúde. Correo electrónico: roliveira@ispa.pt
3 Instituto Superior de Psicologia Aplicada/Unidade de Investigação em Psicologia e Saúde. Correo electrónico: ileal@ispa.pt
Recibido: 14 de marzo de 2013. Aprobado: 30 de octubre de 2013.
Rocha AM, Oliveira R, Leal I. La influencia de la lactancia materna en la salud infantil, el bienestar y el desarrollo: una revisión teórica y empírica. Rev. Fac. Nac. Salud Pública 2014; 32(2): 103-114
RESUMEN
El objetivo fue examinar el efecto de la lactancia materna en la salud infantil, el bienestar y el desarrollo. La revisión de la literatura se acercó a varias dimensiones de la salud del niño y el desarrollo, a fin de evaluar en cuáles hay realmente beneficios de la leche materna y en cuáles no se encuentra una asociación positiva con la lactancia. La hipótesis general de la Organización Mundial de la Salud (oms) de recomendar la lactancia materna durante los primeros seis meses de vida del niño no parece estar confirmada por la literatura, ya que los estudios disponibles se centran en los efectos benéficos muy específicos de la lactancia materna. Por otra parte, las limitaciones de la literatura incluyen la existencia de resultados incongruentes y aspectos metodológicos menos sólidos que deben ser resueltos en futuras investigaciones. Dadas las implicaciones clínicas, sociales y culturales de las políticas referentes a la lactancia materna, es necesario explicar las discrepancias encontradas entre los estudios, y confirmar si la lactancia materna se correlaciona significativamente con la salud de los niños y su bienestar o si en realidad son creencias de salud.
Palabras clave: Lactancia Materna, Salud, Bienestar, Desarrollo
ABSTRACT
The objective was to examine the impact of breastfeeding on children's health, well-being and development. This literature review approached several dimensions of the child's health and development, in order to assess which ones actually benefit from the maternal milk, and which dimensions do not support a positive association with breastfeeding. The general assumption of the World Health Organization (WHO) of recommending breastfeeding during the first six months of the child's life does not seem to be confirmed by the literature, since the available studies are centred in very specific beneficial effects of maternal breastfeeding. Furthermore, the limitations of the literature include the existence of incongruent results and less solid methodological aspects that should be solved in future research. Given the clinical, social and cultural implications of the politics regarding maternal breast feeding, it is necessary to explain the discrepancies found between studies, and to confirm if maternal breastfeeding is significantly correlated with the children’s health and well-being or if they actually are health beliefs.
Key words: Breast feeding; Health; Welfare; Development
Introducción
The protection, promotion and support of breastfeeding are nowadays a priority for public health. These policies for the promotion and maintenance of the maternal breastfeeding have led to a series of political and legal implications (through the emergence of special prerogatives for women who breastfeed), introducing several changes in the healthcare system.
Therefore, there are some global guidelines for implementing programs directed to the promotion of breastfeeding, namely, the Global Strategy for Infant and Young Child Feeding [1], that launched the international focus on the protection, promotion and support of the breastfeeding, renewing what had been previously highlighted by the Code of Marketing of Breast-milk Substitutes [2], the Innocenti Declaration on Protection, Promotion and Support of Breastfeeding [3], the Protection, promotion and supporting breastfeeding: The important role of maternity services [4], and by the Baby Friendly Hospital Initiative [5].
Actually, several world organizations recommend that all women should have the opportunity to breastfeed during the first 6 months and, as complement, until the end of the 2nd year [6].
However, this movement on behalf of maternal breastfeeding has a fragile support from the research developed until the present date, regarding the fundamental reason for the breastfeeding practice: the child’s health and well-being [7, 8). There are actually few studies in this area, and many are methodologically discussable, focus on very specific aspects, and many present contradictory results [9].
It is our goal to present general literature revision since 2000, examining in a substantial way the theoretical and empiric frame concerning the role and impact of the breastfeeding on the child’s health, wellbeing and development.
Current status of knowledge
The Benefits of the Maternal Breast Feeding
Breastfeeding is considered in literature as the ideal food for the children, constituting a primary form of promoting the child’s health and development, given that it is perfectly adjusted to the infant’s nutrition necessities and growth, protecting babies from infections, due to the presence of antibodies and immunoprotective substances [3, 8, 10-15]. The studies also consider that no other nourishment has the same nutritional, protective, psychological and social benefits for the baby [7, 16].
Some authors report the advantages of maternal milk taking into account its immunological constitution and properties, and regarding its influence both on growth and weight in the first months of a child life [17], and on the prevention of illnesses in the short and long run. Also, other studies showed the existence of a positive association between maternal breastfeeding and the prevention of certain illnesses and medical conditions (table 1). Some examples are the prevention of: pain [18]; obesity [11, 14, 19-23], diabetes [11, 14, 19-21, 24, 25], buccal malformations [11], syndrome of the sudden death [11, 12, 15, 24], respiratory infections [12, 14, 20, 21, 24, 26-29], urinary infections [12, 14, 20, 21, 28], otitis [12, 14, 20, 23, 24, 26, 28], cardiac illnesses [23], atopic diseases, such as allergies and asthma [11, 14, 19, 20, 22-24, 26, 28, 30]; lymphomas [14, 20], gastrointestinal infections and diseases [12-14, 20-23, 25, 27-29, 31]; behavioural disorders [32, 33]; arteriosclerosis [34].
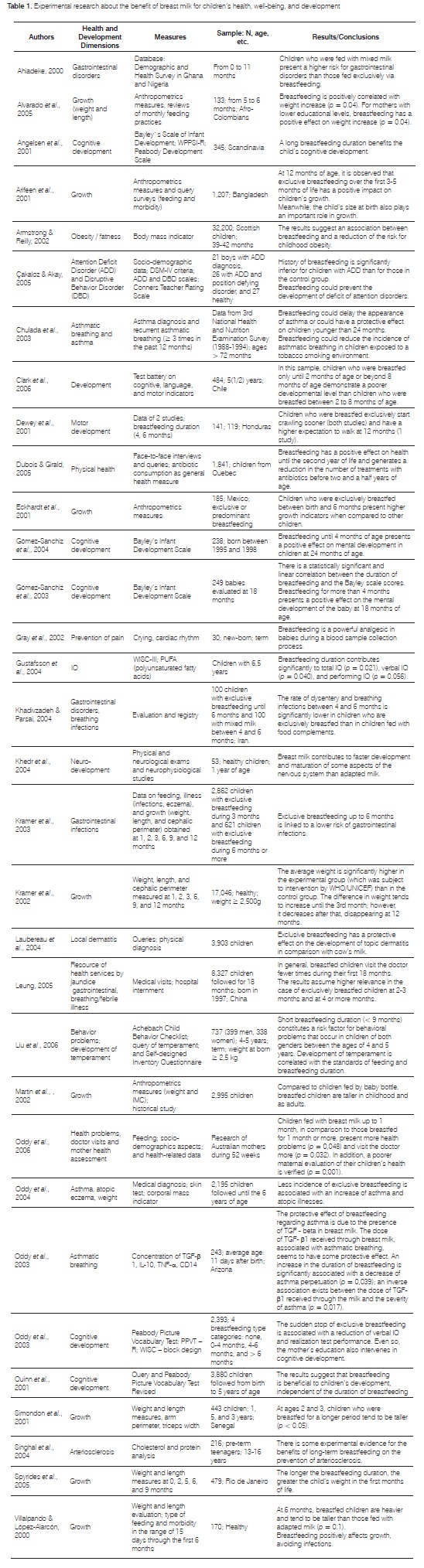
Some studies also refer to the importance of breastfeeding for the mother-child relationship [10, 14, 19-21], being that breastfeeding acts as an analgesic in stressful situations [35]. More recently, some authors have established a positive relation between breastfeeding, especially when exclusive, and intellectual development [11, 19, 20, 23-25, 36]; the brain’s development [31, 36]; the babies’ growth [37-40]; physical health [41, 42]; and cognitive and motor development [43-45].
Two different studies, one by Leung [46] and the other by Oddy, Scott [42], showed that breastfed children, and those who were breastfed for longer, seek medical assistance less frequently. Furthermore, Oddy, Scott [42] concluded that maternal evaluations of the child’s health were more positive in children who were breastfed.
The inconsistencies in the studies
Although the literature review, reported previously, indicated a positive association between breastfeeding and several aspects of health and child development, there are studies that do not support this connection. Filteau [47], questions if the practice of breastfeeding is maintained due to emotional reasons or to experimental evidence, given inconsistency in some results. This author refers that there are no significant differences regarding growth or intestinal problems between children who were breastfed partial or exclusively. He also refers that the immunisation factors of maternal milk exist to protect the mother and not the child; and further refers that maternal milk contains bacteria and viruses harmful to the baby’s health. Wang, Bates [48] through an economics analysis, report that the concerns about maternal milk in our society are diverse, varying from the presence of environmental chemicals in maternal milk, as well as the economic value of breastfeeding for society.
Moreover, other studies have detailed a series of critics about the advantages of maternal milk for health, and about the studies’ methodologies [9, 25]. The author refers that, in spite of existing a protector effect against obesity in a later stage of life, this effect is too small, moreover, no clear association between breastfeeding and cardiac illnesses or death has been asserted, and the effect of breastfeeding on the allergic illnesses remains inconclusive. Thus, the author considers that the effects of maternal milk do not have a significant weight in individual terms, but they are important at the population level [25]. Regarding the methodology, the authors refer that the most studies are observational investigations, making it difficult to establish causal effects, and confounding variables may be due to the added difficulty of differentiating the maternal factors from those that are associated to breastfeeding (e.g., obesity and mental development) [9, 25].
Other authors have concentrated on the influence of breastfeeding on the allergic illnesses; which is a controversial subject, given that some studies have shown that breastfeeding has a protective effect in the atopic illnesses, while others suggest it has an increased risk. Exclusive breastfeeding during the first four months did not disclose an increased risk of developing atopic dermatitis with or without family history of the illness.
However, a considerable amount of studies determined that breastfeeding may constitute a risk factor for atopic dermatitis, suggesting that it might also not be beneficial, or even harmful, to keep on breastfeeding babies that suffer from dermatitis and food allergies [49-51]. Friedman and Zeiger [52] sustain that the reason for this controversy includes the use of different methodologies, flaws in the studies, and also possible genetic differences between the subjects. However, a 20- year follow-up study, developed with 200 Finish infants, showed that, in infants with a family history of allergy, exclusive breastfeeding prolonged for 9 or more months, was associated to an increase in atopic dermatitis and food hypersensitivity symptoms during childhood [53].
Nevertheless, the results from a study developed by Kramer, Matush [54] did not support a protective effect of prolonged and exclusive breast feeding on asthma or allergy.
Despite the fact that specific evidence relating human milk to the appearance of dental cavities does not exist, circumstances related with prolong breastfeeding, namely nocturnal breastfeeding, are associated to the early appearance of dental cavities in infancy. Thus, factors such as frequency, duration and intensity of breastfeeding are extremely important in determining the risk of adverse effects for the child’s development and mouth health [55].
According to Pohl and Tylenda [56], the presence of chlorine based organic pesticides in the maternal milk, has been registered in many studies around the world, being that the interactions between chemicals in the maternal milk can influence its final toxicity. Moreover developing countries present a greater exposition index to these organochlorine pesticides, nevertheless knowledge on the reduced expositions is still scarce, although some studies indicate possible subtle effect.
Despite the consensus on maternal milk being the ideal and more complete food for babies, some studies have pointed out that children who are breastfed need supplements of vitamins D [23] and K [23], which contradicts the idea that maternal milk satisfies all the baby’s needs. The composition of maternal milk presents individual variations, which influence the actual success of breastfeeding in reducing the risk of disease [57]. Moreover, there are some situations or medical conditions where maternal milk is not recommended and may actually be contraindicated, having to be controlled when performed [10, 19].
Lothrop [11], who strongly supports breastfeeding when possible, refers that adapted milk formulas are perfectly adjusted to the baby’s needs, recognizing that children fed with adapted milk formulas develop without any growth disorders, deficiencies or diseases. Beyond the medical issues, several studies support that there are many other forms to establish the same type of proximity and affective bond that the baby has to the breast, through the baby bottle [11, 26].
Authors refer that the effects of maternal milk depend on the gestational age and clinical situation of the child. According to Reynolds [58], the effect of breastfeeding in the development of full term children seems to be minimum or insignificant, on the other hand, for healthy children; the differences are not substantial from the clinical point of view. Thus, the benefits of maternal milk can be more significant for premature or ill babies [11, 59], or in the case of full term children with low weight for their gestational age [60, 61].
In this way, and according to Pilkington [62], the politics of breastfeeding promotion must be cautiously adapted to the existing epidemiologist context, at a local level and in a small scale.
Specific information about the studies that do not support a positive association between maternal milk and the health, development and well-being of the child can be found on table 2. These studies do not consider breastfeeding to have an actual impact on the pain relief [63]; growth [37-40, 42, 64]; cognitive development [43- 45]; prevention of atopic diseases [22, 29]; haemophilia [65, 66]; respiratory infections [29]; cardiovascular diseases [64]; obesity [30]; and diabetes [67].

Furthermore, Leung [46] concluded that the breastfed children have more frequent doctor appointments, and are more frequently hospitalized due to jaundice than bottle-fed babies.
Conclusions
This literature review examined the way breastfeeding is related with the child’s health, well-being and development. The areas under analysis here included several dimensions: growth and weight, obesity, diabetes, buccal malformations, breathing infections, heart problems or diseases, atopic diseases, gastro-intestinal infections, motor and cognitive development, mother-baby relationship, pain prevention, physical health, and visits to doctors. These dimensions were approached both by studies about benefits of maternal breastfeeding, and by studies that contradict those findings.
Regarding the benefits of breast milk, the dimensions behaviour disorders, arteriosclerosis, syndrome of the sudden death, urinary infections, otitis and lymphomas were referenced in several studies. Also, Oddy, Scott [42] concluded that the maternal evaluation of the child’s health is more positive when the children are breastfed.
However, regarding these pathologies, the reviewed studies did not identify a positive association between breastfeeding and haemophilia [65, 66]. It is also highlighted that breastfed children are more frequently hospitalized due to jaundice [46], and present more frequently oral cavities during childhood [55].
Beyond the critics to the advantages of the breast milk, several studies have shown that it contains harmful substances to the baby’s health, such as bacteria, viruses and environmental chemical substances (e.g. chlorine based organic pesticides) [47, 48, 56]. Furthermore, these studies point out that the methodologies used by researchers are generally observational, making it difficult to establish concrete causal effects [25].
As we can observed, in spite of breastfeeding being a widely studied area, there still exists a great variety of pertinent aspects that need to be analysed, especially because most of the studies accomplished so far approach very specific variables, and in a repeated way.
However, the child’s nutritional needs are today more thoroughly known, and the importance of an adequate nutrition is universally recognized. Therefore, given the clinical, social and cultural implications of the politics for the promotion and maintenance of maternal breast feeding, it is necessary to explain the discrepancies between these studies, deepening the knowledge through the development of scientific research using thorough methodologies and instruments used (specifically regarding the development of longitudinal studies), in order to confirm if maternal breastfeeding is significantly correlated with the children’s health and well-being or if they actually are health beliefs [68, 69].
References
1 World Health Organization. Global Strategy for Infant and Young Child Feeding. Geneva: World Health Organization; 2003. [ Links ]
2 World Health Organization. International code of marketing of breast-milk substitutes. Geneva: World Health Organization; 1981. [ Links ]
3 United Nations Children’s Fund. Innocenti declaration on the protection, promotion and support of breastfeeding. New York: unicef’s Nutrition Cluster; 1990. [ Links ]
4 World Health Organization, unicef. Protection, promotion and supporting breastfeeding: The important role of maternity services. Geneva: World Health Organization; 1989. [ Links ]
5 World health Organization, unicef. Baby Friendly Hospital Initiative Geneva: World Health Organization; 1991. [ Links ]
6 unicef, World Health Organization, United Nations Educational SaCO, unfpa, undp, unaids, et al. Facts of Life. New York: United Nations Children’s Fund; 2010. [ Links ]
7 Gomes-Pedro J. Nutrição, desenvolvimento e bem-estar. Silva A, Gomes-Pedro J, editors. Lisboa: ACSM - Clínica Universitária de Pediatria - Hospital de Santa Maria; 2005. [ Links ]
8 Jackson K, Nazar A. Breasfeeding, the immune response, and long-term health. The Journal of the American Osteopathic Association 2006;106(4): 203-207. [ Links ]
9 Schack-Nielsen L, Michaelsen KF. Advances in our understanding of the biology of human milk and its effects on the offspring. The Journal of Nutrition. 2007;137(2):503S-10S [ Links ]
10 Fanaro S. The biological specificity and superiority of human milk. Scientific basis, guarantees and safety controls. Minerva Pediatric 2002;54(2):113-129. [ Links ]
11 Lothrop H. Vale a pena amamentar. In: Lothrop H, editor. Tudo sobre amamentação. Lisboa: Paz Editora; 2000. p. 19-47. [ Links ]
12 Oddy W. Breastfeeding and health in infants and children. Nutridate 2000;11(3):1-5. [ Links ]
13 Oddy W. The impact of breastmilk on infant and child health. Breastfeeding Review: Professional Publication of the Nursing Mothers’ Association of Australia 2002;10(3):5-18. [ Links ]
14 Schiff L. Breastfeeding makes for better health. Mount Sinai Journal of Medicine. 2006;73(2):571-2. [ Links ]
15 Hauck FR, Thompson JMD, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: A meta-analysis. Pediatrics 2011;128(1):103-110. [ Links ]
16 Pérez-Escamilla R, Vianna RPT. Breastfeeding and infant pneumonia in Brazil: the value of electronic surveillance information systems. Jornal de Pediatria. 2011;87(5):371-2. [ Links ]
17 Fulhan J, Collier S, Duggan C. Update on pediatric nutrition: Breastfeeding, infant nutrition, and growth. Current Opinion in Pediatrics 2003;15(3):323-332. [ Links ]
18 Gray L, Miller L, Philipp B, Blass E. Breastfeeding is analgesic in healthy newborns. Pediatrics 2002;109(4):590-594. [ Links ]
19 Leung AK, Sauve RS. Breast is best for babies. Journal of the National Medical Association 2005;97(7):1010-1019. [ Links ]
20 Levy L. Alimentação do lactente, aleitamento materno: filosofia, vantagens e práticas. In: Silva A, Gomes-Pedro J, editors. Nutrição Pediátrica: Princípios Básicos Lisboa: ACSM - Clínica Universitária de Pediatria - Hospital de Santa Maria; 2005. p. 69- 75. [ Links ]
21 Levy L. Aleitamento materno: Uma prioridade. In: Rosa J, Sousa S, editors. Caderno do bebé. Lisboa: Fim de Século; 2006. p. 37- 39. [ Links ]
22 Oddy W. A review of the effects of breastfeeding on respiratory infections, atopy, and childhood asthma. Journal of Asthma. 2004;41(6):605-621. [ Links ]
23 Turck D, Bocquet A, Bresson J, Briend A, Chouraqui J, Darmaun D, et al. Allaitement maternel : les bénéfices pour la santé de l’enfant et de sa mère. In: Ministére des Solidarités dlSedlF, Pédiatrie SFd, editors.: Parimage; 2005. p. 145-165. [ Links ]
24 Gartner L, Morton J, Lawrence R, Naylor A, O’Hare D, Schanler R, et al. Breastfeeding and the use of human milk. Pediatrics 2005;115(2):496-507. [ Links ]
25 Schack-Nielsen L. Breast feeding and future health. Current Opinion in Clinical Nutrition & Metabolic Care. 2006;9 (3):289-269. [ Links ]
26 Brazelton T, Sparrow J. A criança e a alimentação. Barcarena: Editorial Presença; 2004. [ Links ]
27 Fisk CM, Crozier SR, Inskip HM, Godfrey KM, Cooper C, Roberts GC, et al. Breastfeeding and reported morbidity during infancy: findings from the SouthamptonWomen’s Survey. Maternal and Child Nutrition 2011; 7:61-70. [ Links ]
28 Hanson L, Korotkova M, Haversen L, Mattsby-Baltzer I, Hahn- Zoric M, Silfverdal S, et al. Breastfeeding, a complex support system for the offspring. Pediatrics International. 2002;44(4):347-52. [ Links ]
29 Kramer M, Guo T, Platt R, Sevkovskaya Z, Dzikovich I, Collet J, et al. Infants growth and health outcomes associated with 3 compared with 6 months exclusive breastfeeding. The American Journal of Clinical Nutricion 2003;78(2):291-295. [ Links ]
30 Oddy W, Sherriff J, De Klerk N, Kendall G, Sly P, Beilin L, et al. The relation of breastfeeding and body mass index to asthma and atopy in children: a prospective cohort study to age 6 years. American Journal of Public Health 2004;94(9):1531-1537. [ Links ]
31 Semba R, Juul S. Erytropoietin in human milk: physiology and role in infant health. Journal of Human Lactation: Official Journal of International Lactation Consultant Association. 2002;18(3):252- 261. [ Links ]
32 Çakaloz B, Akay A. The effect of prenatal, perinatal and postnatal problems and breast feeding duration, on the development of psychopathology in attention deficit and disruptive behaviour disorders. Cocuk Ve Gençlik Ruh Sagligi Dergisi 2005;12(1):3-10. [ Links ]
33 Liu F, Ma L, Yi M. Association of breastfeeding with behavioral problems and temperament development in children aged 4-5 years. Chinese Journal of Contemporary Pediatrics 2006;8(4):334- 337. [ Links ]
34 Singhal A, Cole T, Fewtrell M, Lucas A. Breastmilk feeding and lipoprotein profile in adolescents born preterm: follow-up of a prospective randomised study. Lancet 2004;363 (9421):1571- 1578. [ Links ]
35 Potter B, Rindfleisch K. Breastfeeding reduces pain in neonats. Journal of Family Practice 2003;52(5):349-352. [ Links ]
36 Jedrychowski W, Perera F, Jankowski J, Butscher M, Mroz E, Flak E, et al. Effect of exclusive breastfeeding on the development of children’s cognitive function in the Krakow prospective birth cohort study European Journal of Pediatrics 2012;171:151-158. [ Links ]
37 Eckhardt C, Rivera J, Adair L, Martorell R. Full breastfeeding for at least four months has differential effects on growth before and after six months of age among children in a Mexican community. Journal of Nutrition 2001;131:2304-2309. [ Links ]
38 Martin R, Smith G, Mangtani P, Frankel S, Gunnel D. Association between breast feeding and growth: The Boyd-Orr cohort study. Archives of Disease in Dhildhood Fetal and Neonatal Edition 2002;87:193. [ Links ]
39 Simondon K, Simondon F, Costes R, Delaunay V, Diallo A. Breastfeeding is associated with improved growth in length, but not weigt, in rural Senegalese toddlers. American Journal of Clinical Nutrition 2001;73(5):959-967. [ Links ]
40 Spyrides M, Struchiner C, Barbosa M, Kac G. Amamentação e crescimento infantil : um estudo longitudinal em crianças do Rio de Janeiro, Brasil, 1999/2001. Caderno Saúde Pública 2005;21(3):756-766. [ Links ]
41 Dubois L, Girald M. Breastfeeding, day-care attendence and the frequency of antibiotic treatments from 1.5 to 5 years: a population- based longitudinal study in Canada. Social Science & Medicine 2005;60(9):2035-2044. [ Links ]
42 Oddy W, Scott J, Graham K, Binns C. Breastfeeding influences on growth and health at one year of age. Breastfeeding Review: Professional Publication of the Nursing Mothers’ Association of Australia 2006;14(1):15-23. [ Links ]
43 Angelsen N, Vik T, Jacobsen G, Bakketeig L. Breast feeding and cognitive development at age 1 and 5 years. Archives of Disease in Childhood 2001;85:183-188. [ Links ]
44 Gómez-Sanchiz M, Cañete R, Rodero I, Baeza E, Ávila O. Influence of breastfeeding on mental and psychomotor development. Clinical Pediatrics 2003;42(1):35-43. [ Links ]
45 Gómez-Sanchiz M, Cañete R, Rodero I, Baeza E, González A. Influence of breastfeeding and parental intelligence on cognitive development in the 24-month-old child. Clinical Pediatrics. 2004;43(8):753-761. [ Links ]
46 Leung G. Health consequences of breastfeeding: doctors’visits and hospitalizations during the first 18 months of life in Hong Kong Chinese infants. Epidemiology 2005;16(3):328-335. [ Links ]
47 Filteau SM. Role of breastfeeding in managing malnutrition and infectious disease. The Proceedings of the Nutrition Society 2000;59(4):565-572. [ Links ]
48 Wang R, Bates M, Goldstein D, Haynes S, Hench K, Lawrence R. Human milk research for answering questions about human health. Journal of Toxicology & Environmental Health: Part A. 2005;68(20):1771-1801. [ Links ]
49 Bonilla S, Kaplan M. Effects of breastfeeding of the development of atopic dermatitis during the first 3 years of life-results from the gini-birth cohort study. Pediatrics 2005;116:539-540. [ Links ]
50 Böttcher M, Jenmalm M. Breastfeeding and the development of atopic disease during childhood. Clinical and Experimental Allergy 2002;32:159-161. [ Links ]
51 Han Y, Chung S, Kim J, Ahn K, Lee S. High sensitization rate to food allergens in breastfed infants with atopic dermatitis Annals of Allergy, Asthma & Immunology 2010;103(4):332–336. [ Links ]
52 Friedman N, Zeiger R. The role of breastfeeding in the development of allergies and asthma. The journal of Allergy and clinical Immunology 2005;115(6):1238-1248. [ Links ]
53 Pesonen M, Kallio MJ, Ranki A, Siimes MA. Prolonged exclusive breastfeeding is associated with increased atopic dermatitis: a prospective follow-up study of unselected healthy newborns from birth to age 20 years.Clinical & Experimental Allergy 2006;36 (8):1010- [ Links ]1018.
54 Kramer M, Matush L, Vanilovich I, Platt R, Bogdanovich N, Svekovskaya Z, et al. Effect of prolonged and exclusive breast feeding on risk of allergy and asthma: Cluster randomised trial. British Medical Journal 2007;335(7624 ):815-818. [ Links ]
55 Sanchez O, Childers N. Breastfeeding and infant oral health. American Family Physician. 2000;63(3):506-507. [ Links ]
56 Pohl H, Tylenda C. Breastfeeding exposure of infants to selected pesticides: a public health viewpoint. Toxicology and Industrial Health 2000;16:65-77. [ Links ]
57 Hoppu U, Kalliomaki M, Laiho K, Isolauri E. Breast milk immunomodulatory signals against allergic diseases. Allergy 2001;56:23-26. [ Links ]
58 Reynolds A. Breastfeeding and brain development. Pediatric Clinics of North America 2001;48(1):159-171. [ Links ]
59 Nascimento M, Issler H. Breastfeeding: making the difference in development, health and nutrition of term and preterm newborn. Revista do hospital das Clínicas, Faculdade de Medicina São Paulo. 2003;58(1):49-60. [ Links ]
60 Daniels M, Adair L. Breastfeeding influences cognitive development in Filipino children. Journal of Nutrition. 2005;135(11):2589- 2595. [ Links ]
61 Rao M, Hediger M, Levine R, Naficy A, Vik T. Effect of breastfeeding on cognitive development of infants born small for gestational age. Acta Paediatrica. 2002;91(3):267-274. [ Links ]
62 Pilkington H. Should we encourage exclusive breastfeeding at all cost? Lancet. 2003;362(9379):247. [ Links ]
63 Bilgen H, Ozek E, Cebeci D, Ors R. Comparison of sucrose, expressed breast milk, and breastfeeding on the neonatal response to heel prick. The Journal of pain: Official Journal of the American Pain Society. 2001;2(5):301-305. [ Links ]
64 Martin R, Holly J, Smith G, Ness A, Emmett P, Rogers I, et al. Could associations between breastfeeding and insulin-like growth factors underline associations of breastfeeding with adult chronic disease? The Avon Longitudinal Study of Parents and Children. Clinical Endocrinology. 2005;62:728-37. [ Links ]
65 Jansen I, Fischer K, Van Der Bom J, Van Der Berg H. No protective effect of breastfeeding on inhibitor formation in severe hemophilia. Pediatric Hematology and Oncology 2005;22(7):575-580. [ Links ]
66 Knobe K, Tengborn L, Petrini P, Ljung R. Breastfeeding does not influence the development of inhibitors in haemophilia. Haemophilia 2002;8:657-659. [ Links ]
67 Sadauskaite-Kuehne V, Ludivigsson J, Padaiga Z, Jasinskiene E, Samuelsson U. Longer breastfeeding is an independent protective factor against development of type 1 diabetes mellitus in childhood. Diabetes/Metabolism Research and Reviews 2004;20(2):150-157. [ Links ]
68 Shirley S. Nós e a metadona: atitudes e crenças dos profissionais de saúde face ao tratamento de manutenção com metadona (MMT). Lisboa: Instituto Superior de Psicologia Aplicada; [ Links ] 2004.
69 Simara A. Crenças de saúde e comportamentos sexuais de risco face ao VIH/SIDA em estudantes universitários Angolanos e Portugueses - Um estudo comparativo. Lisboa: Instituto Superior de Psicologia Aplicada; 2002. [ Links ]













